Introduction
Chronic parotid sialadenitis is an uncommon benign inflammatory disorder characterised by recurrent painful swelling of the gland, often associated with eating. It is more common in females, with a peak incidence between 40 and 60 years old.Reference Harbison, Liess, Templer, Zitsch and Wieberg1 The pathophysiology is unclear and aetiology likely multifactorial. Reduced salivary secretion is considered to be an important patho-aetiological factor as it results in stasis and inspissation of secretions, predisposing to retrograde bacterial contamination of the ductal system.Reference Bhatty, Piggot, Soames and McLean2 Progressive sialectasis and acinar destruction ensues.
Approximately 50 per cent of patients can be managed with conservative treatment including sialagogues, gland massage, good dental hygiene, analgesics and occasionally antibiotics.Reference Moody, Avery, Walsh, Sneddon and Langdon3 However, some patients may develop intractable symptoms due to parenchymal fibrosis resulting from repeated inflammatory episodes. This results in significant morbidity and requires surgical management for definitive treatment. However, because surgery is performed relatively infrequently for this condition, there are limited case series in the literature, and controversy exists over the most appropriate surgical intervention, specifically the extent of parenchymal resection required to achieve a cure whilst minimising morbidity (superficial vs near-total parotidectomy).
We report the clinical outcomes of patients treated with superficial parotidectomy for chronic parotid sialadenitis in our institution and review the literature on the surgical management of this challenging condition.
Materials and methods
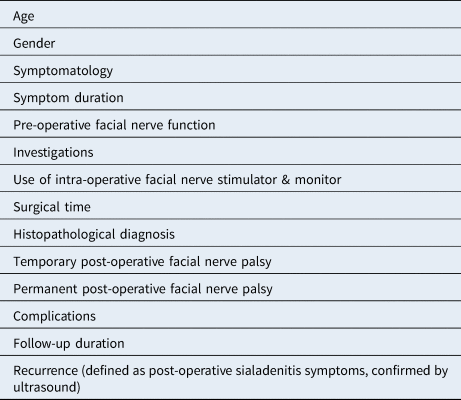
All patients undergoing parotidectomy for chronic parotid sialadenitis at Bradford Teaching Hospitals NHS Foundation Trust between 2009 and 2018 were retrospectively identified from a prospectively collated computerised database. The clinicopathological data recorded are outlined in Table 1. The primary outcomes were recurrence and complications including temporary and permanent facial nerve palsy. A literature review using PubMed was subsequently undertaken.
Table 1. Clinicopathological data
Results
A total of 18 patients were included in this study. Fifteen patients were referred by their general practitioner (10 routine, 3 fast-track for suspected malignancy and 2 urgent referrals), one from the emergency department during an acute attack and two from other specialties. There were 11 women and 7 men, with an average age at presentation of 52 years (range, 19–72 years).
The commonest presentation was pain and swelling whilst eating (n = 14). One patient complained of intermittent facial swelling and cheek numbness, and three patients presented with a parotid mass. There were no cases of facial nerve palsy at the time of presentation. The duration of symptoms prior to first consultation varied considerably, with a mean duration of 8.28 months (range, 4–24 months).
A clinical diagnosis of chronic parotid sialadenitis was made based on symptomatology and ultrasound characteristics of the affected gland. The three patients presenting atypically with a parotid mass had undergone ultrasound-guided fine needle aspiration. Magnetic resonance imaging (MRI) was performed for all patients prior to surgical intervention.
All patients underwent an initial period of conservative treatment with suboptimal results. This included a combination of oral hygiene measures, analgesics, sialagogues, external gland massage and antibiotics when required. The minimum symptom duration prior to surgical intervention was 11 months.
The decision to operate was clinically based after failure of a trial of conservative treatment. The decision was made in conjunction with the patients, who all had significant ongoing symptoms to an extent that they wished to proceed with surgical intervention. Eighteen superficial parotidectomies were performed with intra-operative facial nerve monitoring and stimulation. The mean surgical time was 2 hours and 24 minutes (range, 1 hour and 20 minutes to 4 hours).
The diagnosis of chronic parotid sialadenitis was confirmed by histopathological examination of the resected specimen (Table 2).
Table 2. Histopathological diagnosis
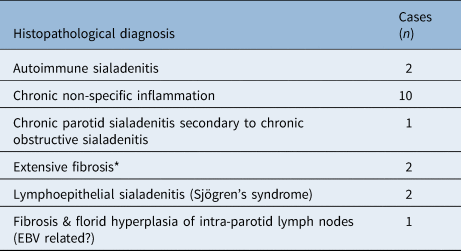
*Post-radioactive iodine treatment for papillary thyroid carcinoma. EBV = Epstein–Barr virus
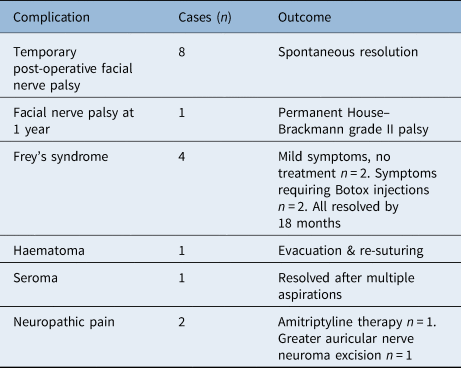
Nine patients experienced complications (Table 3). There were eight temporary post-operative facial nerve palsies (House–Brackmann grade I–III); however, by 18 months, only one patient had an ongoing, permanent facial nerve palsy (House–Brackmann grade II). There was one post-operative wound haematoma and one seroma. Four patients developed Frey's syndrome approximately six months post-operatively, of which two required Botox® injections. Two patients suffered from neuropathic pain, with one of these patients subsequently requiring surgical excision of a greater auricular nerve neuroma. One wound infection required oral antibiotics.
Table 3. Post-operative complications and their outcome
All patients were routinely reviewed three to four weeks post-operatively, and followed up for at least nine months or until free of complications (range, 9–24 months). Complete symptom resolution occurred in 17 patients. There was only one recurrence, albeit of a milder form of the disease, requiring no specific treatment.
Discussion
Chronic parotid sialadenitis results from a reduction in the salivary secretion rate, with subsequent ductal stasis, infection and eventual fibrosis.Reference Moody, Avery, Walsh, Sneddon and Langdon3 Obstructive causes include ductal strictures, calculi, mucus plugs, extrinsic compression, ductal injury or congenital abnormalities. Non-obstructive causes, as highlighted by our series, may be idiopathic, or associated with immune-mediated disease, radiotherapy or radioactive iodine treatment. Despite the different aetiologies, 17 of our 18 patients had complete symptom resolution following superficial parotidectomy.
It is generally accepted that the initial management of chronic parotid sialadenitis should be conservative. Watkin and HobsleyReference Watkin and Hobsley4 studied the natural history of the condition, and showed that oral hygiene measures, sialagogues, gland massage, analgesics and antibiotics could improve symptoms in 38 per cent of patients, and could completely resolve symptoms in 6 per cent. All patients in this series had symptoms for at least 11 months prior to surgical intervention, which reflects our practice of an initial trial of conservative management in the absence of localised mechanical obstruction. It is only when conservative therapy has failed, or when a tumour cannot be excluded, that surgical intervention becomes appropriate.
Chronic parotid sialadenitis is largely a clinical diagnosis and the ideal radiological investigation is controversial. Historically, in the presence of ‘classical’ symptoms in the early phases of disease, sialography was the cornerstone of radiological imaging. Ultrasonography is now used more frequently, as it is less invasive, provides a higher diagnostic yield without radiation exposure, can be utilised in acute inflammation and is ideal for follow up. Our patients had a range of radiological investigations with no set investigation protocol, in part a result of investigations being requested by other specialties or the general practitioner prior to referral. However, all patients in our series had a diagnostic ultrasound scan with or without fine needle aspiration (in patients presenting with a fibrotic mass), followed by MRI to determine the extent of the inflammatory process, prior to surgical intervention.
The goal of surgery for chronic parotid sialadenitis is to achieve symptom eradication with minimal morbidity. Historically, parotid duct ligation has been trialled in an attempt to induce pressure atrophy and prevent retrograde ductal infection; however, there is no histological evidence that atrophy occurs, and there is a high risk of recurrence, fistula formation and facial nerve injury.Reference Morgan5,Reference Nichols6 Tympanic neurectomy has also been discredited because of ineffective and unreliable results.Reference Nichols6 Several studies have shown good results with parotidectomy for chronic parotid sialadenitis, which is now widely considered the treatment of choice for medically refractory disease.Reference Moody, Avery, Walsh, Sneddon and Langdon3,Reference Bates, O'Brien, Tikaram and Painter7,Reference Amin, Bailey and Patel8 However, there is still debate regarding superficial versus near-total techniques. The latter procedure involves performing a superficial parotidectomy with subsequent ‘piece-meal’ excision of the deep lobe parenchyma from between branches of the facial nerve.
Owing to the chronic inflammation and parenchymal fibrosis, parotidectomy for chronic parotid sialadenitis is more challenging than for other benign disease. Within our study and nine other case series reported in the literature over the last 30 years (Table 4),Reference Bhatty, Piggot, Soames and McLean2,Reference Moody, Avery, Walsh, Sneddon and Langdon3,Reference Bates, O'Brien, Tikaram and Painter7–Reference Arriaga and Myers13 permanent facial nerve palsy occurred in 1.1 per cent of cases (4 out of 350 cases). Bates et al.Reference Bates, O'Brien, Tikaram and Painter7 and Patel et al.Reference Patel, Low, Gao and O'Brien9 each report a single case of permanent palsy; however, these patient populations overlap, and neither study states whether the patients with a permanent palsy had a superficial or near-total parotidectomy. SharmaReference Sharma10 and Nouraei et al.Reference Nouraei, Ismail, McLean, Thomson, Milner and Welch11 reported zero and one case of permanent palsy following superficial parotidectomy respectively. Therefore, it appears the incidence of a permanent facial nerve palsy following parotidectomy performed for chronic parotid sialadenitis is low, and comparable with parotidectomy carried out for other benign parotid disease.Reference Sharma10–Reference Van der Lans, Lohuis, van Gorp and Quak12
Table 4. Summary of case series between 1990 and 2020

However, there are mixed results in the literature comparing the incidence of temporary facial nerve palsy following parotidectomy performed for chronic parotid sialadenitis versus other benign parotid disease. With respect to temporary facial nerve palsy, eight patients in our cohort were affected. This is within the range reported by other case series in the literature over the last 30 years (Table 4). Van der Lans et al.Reference Van der Lans, Lohuis, van Gorp and Quak12 performed 5 superficial and 41 near-total parotidectomies, and found no significant association between the extent of the parenchymal resection and the incidence of temporary facial nerve palsy. Similar conclusions were drawn by Patel et al.Reference Patel, Low, Gao and O'Brien9 and Nouraei et al.Reference Nouraei, Ismail, McLean, Thomson, Milner and Welch11 Hence, there seems to be no clear evidence to substantiate the misconception that a near-total parotidectomy is associated with a higher incidence of either a permanent or temporary facial nerve palsy.
Although our permanent facial nerve palsy rate was acceptably low, other recognised complications of parotidectomy occurred relatively frequently. An exception to this was the incidence of Frey's syndrome (n = 4), which is lower than the incidence reported in the literature for benign parotid disease, albeit a small sample size. Two out of the four patients with the syndrome required a single treatment with Botox for symptom resolution.
Table 4 reports the results of case series for ‘chronic parotitis’ managed with parotidectomy over the last 30 years. Analysis of the results shows that symptom recurrence occurred in 26 out of 350 patients (7.4 per cent). One patient in our series suffered a recurrence, albeit a milder form of the disease not requiring further surgical intervention. This is in keeping with other studies in the literature, which report a recurrence rate between 0 and 16.7 per cent (Table 4). Van der Lans et al.Reference Van der Lans, Lohuis, van Gorp and Quak12 reported recurrence in six patients (13 per cent), three undergoing superficial parotidectomy and three near-total. Four of these patients were managed conservatively, one opted for salvage near-total parotidectomy and one declined any further treatment. Nouraei et al.Reference Nouraei, Ismail, McLean, Thomson, Milner and Welch11 reported a 5 per cent treatment failure incidence following superficial parotidectomy, but none of these patients required salvage near-total parotidectomy. However, neither of the above studies found a significant difference between the extent of surgery and recurrence. This result is corroborated by four other studies in the literature detailing enough information to allow statistical analyses (p > 0.1–0.3).Reference Patel, Low, Gao and O'Brien9,Reference Van der Lans, Lohuis, van Gorp and Quak12,Reference Beahrs, Devine and Woolner14,Reference Casterline and Jaques15
• Surgical management of chronic parotid sialadenitis should be considered only when conservative therapy has failed
• Studies have shown good results with parotidectomy, widely considered the choice treatment for medically refractory chronic parotid sialadenitis
• Risk of permanent facial nerve palsy with superficial parotidectomy is low and comparable with parotidectomy for other benign parotid disease
• This study demonstrates that superficial parotidectomy is safe and effective for medically refractory chronic parotid sialadenitis
• Superficial parotidectomy obviates the need for a more extensive parenchymal resection associated with increased morbidity
Therefore, although recurrence is likely due to the presence of residual parotid tissue, it would appear that superficial parotidectomy removes enough parenchyma to attain a satisfactory therapeutic outcome. Furthermore, superficial parotidectomy is associated with a shorter operative time, results in better cosmesis and may be associated with a reduced incidence of first bite syndrome when compared with near-total parotidectomy.Reference Linkov, Morris, Shah and Kraus16 Despite this, some authors argue successful management requires removal of as much of the parotid parenchyma as possible, whilst preserving the facial nerve.Reference Moody, Avery, Walsh, Sneddon and Langdon3,Reference Bates, O'Brien, Tikaram and Painter7 Furthermore, advocates of near-total parotidectomy contest the presumed higher risk of facial nerve injury, which is supported by the results of some case series in the literature.Reference Moody, Avery, Walsh, Sneddon and Langdon3,Reference Patel, Low, Gao and O'Brien9,Reference Beahrs, Devine and Woolner14
Conclusion
Our series supports the theory that superficial parotidectomy is sufficient to control patients’ symptoms, avoiding the increased morbidity associated with near-total parotidectomy. There is a risk of recurrence of a milder form of the condition, although this has also been reported following near-total parotidectomy. Furthermore, the literature does not point to a clear difference in the incidence of recurrence, or temporary and permanent facial nerve palsy, between the two procedures. The symptoms attributed to recurrence are often not severe enough to warrant salvage near-total parotidectomy, a procedure which poses a greater risk of some of the recognised complications of parotid surgery.
Competing interests
None declared






