Introduction
Surgical treatment for chronically troubled ears is a widely discussed subject. Troubled cavities are defined as cavities with cerumen accumulation that need frequent cleaning at the out-patient clinic, are intolerant to water, and have frequent infection and otorrhoea.Reference Choi, Cho, Lee, Lee, Chung and Hong 1 Surgical problems of radical cavities include a narrow meatus, high facial ridge and residual mastoid cells.Reference Choi, Cho, Lee, Lee, Chung and Hong 1 Since Blake first described mastoid cavity obliteration in 1906,Reference Blake 2 several revision radical cavity surgery techniques have been proposed. For example, mastoid obliteration was proposed by Yung et al.Reference Yung and Smith 3 Such obliteration techniques have become more popular in recent decades because they might prevent residual or recurrent cholesteatoma growth into the mastoid cavity.Reference Choi, Cho, Lee, Lee, Chung and Hong 1 Moreover, relatively new visualisation techniques such as diffusion-weighted magnetic resonance imaging (MRI) facilitate adequate follow up.Reference Yung and Bennett 4 Yung et al. published the most recent overview of different obliteration techniques and materials in 2007, in which they reported a dry ear rate of 95 per cent in the total cohort and 100 per cent in the five-year follow-up group using their own technique. Since 2007, the same technique has been used at the Department of Otorhinolaryngology, Academic Medical Center, a tertiary referral centre for otology in the Netherlands. The first objective of this study was to confirm the published results in a cohort of patients who presented at the Department of Otolaryngology, Academic Medical Center, for revision surgery because of persistent troublesome and draining cavities. Age-related outcomes were also evaluated. Patients with troublesome cavities are characterised by the need for multiple operations and multiple visits to an out-patient clinic each year. As well as affecting the troubled ear, the disorder also restricts patients’ activities and social interactions.Reference Choi, Cho, Lee, Lee, Chung and Hong 1 , Reference Baumann, Gerendas, Plinkert and Praetorius 5 , Reference Jung, Cho, Hong, Chung, Lee and Hong 6 The second objective was to grade troublesome cavities using the standardised format of Merchant et al.Reference Merchant, Wang, Jang, Glynn, Rauch and McKenna 7 Results of added canaloplasty and/or meatoplasty to revision radical cavity surgery was also reviewed. In line with a previous suggestion by the senior author that changing the shape of the ear canal could be favourable in chronic otitis externa,Reference Van Spronsen, Geerse, Mirck, Van der Baan, Fokkens and Ebbens 8 this procedure was considered likely to be favourable for treating the present cohort.
Materials and methods
Patients
All patients with chronically troubled and/or draining mastoid cavities who underwent the obliteration technique (described by Yung et al.Reference Yung and Smith 3 ) at the Department of Otolaryngology, Academic Medical Centre, between 2007 and 2013 were included in this study. Patients with canal wall up mastoidectomy and revision radical surgery without obliteration were excluded. The cohort was divided into paediatric, adult and elderly patient groups to evaluate possible age-related differences in outcome.
Study design
The medical records of all patients were retrospectively analysed. Patient characteristics, surgical indication, presence of dry ears, epithelialisation time, presence of residual or recurrent disease, and complications were recorded.
Surgical technique
The surgical technique of Yung et al. was used because it had previously produced good results regarding to dry ears and residual cholesteatoma.Reference Yung and Smith 3 Surgery was performed by four different otologists. In all patients, a retroauricular incision was first made to prepare a vascularised mid-temporal flap. Revision of the modified radical cavity was then performed to eradicate all cholesteatoma and/or debris. The main filler used for obliteration was hydroxyapatite granules (1–2 mm diameter; TekniMed Ceraform®, soaked in ofloxacin eardrops (Trafloxal®)), sometimes combined with bone dust. A new posterior external auditory canal wall was then created using autologous tragal and/or conchal cartilage and the mid-temporal flap. One slight modification to Yung and colleagues’ technique was made: only the mid-temporal flap (and not the second inferiorly based periosteal flap) was used.Reference Yung and Smith 3 When required, canaloplasty (as previously described by Van Spronsen et al.) and/or meatoplasty (as previously described by Mirck) was performed.Reference Van Spronsen, Ebbens, Mirck, Van Wettum and van der Baan 9 , Reference Mirck 10
Patients underwent routine post-operative follow up at two weeks, four weeks, three months, six months and then annually. Interval diffusion-weighted MRI of the mastoid bone was performed after one year, three years and between five and six years.
Grading of troubled cavities
Cavities were graded pre- and post-revision radical cavity surgery with mastoid obliteration as described by Merchant et al.Reference Merchant, Wang, Jang, Glynn, Rauch and McKenna 7 : grade 0, a completely dry ear; grade 1, subjective feeling of wetness or one episode of otorrhoea of less than two weeks’ duration; grade 2, worsening of otorrhoea and presence of granulation tissue; and grade 3, a clear failure to control infection or a need for revision surgery. Merchant et al. suggested that post-operative grading should be done at 4–6, 7–12, 13–24 and 25–36 months.Reference Merchant, Wang, Jang, Glynn, Rauch and McKenna 7 In the present study, grading was also performed after at least 36 months and at the 5-year follow up. It was decided to stratify patient groups by the time of last contact rather than including all patients until they dropped out.
Statistical analysis
Data were analysed using Microsoft Office Excel 2010 (Microsoft, Redmond, Washington, USA) and are expressed as n (percentage) and median (range). Kaplan–Meier analysis was used to evaluate the residual cholesteatoma rate. Chi-square analysis was used to evaluate the results and to compare patient subgroups with and without canaloplasty and/or meatoplasty.
Results
Patients
Between 2007 and 2013, 121 patients (122 ears) underwent revision radical cavity surgery with mastoid obliteration. Patient demographics and age-related outcomes are shown in Table I. In this cohort, the main presenting symptom was therapy-resistant otorrhoea (112 ears; 92 per cent). Residual cholesteatoma without otorrhoea was present in four patients. All patients had previously undergone surgery at least once and a maximum of six times (Figure 1). The median number of previous procedures was two (range one to six) and overall one-third of the total cohort had undergone at least three procedures. Figure 1 provides an overview of the previous number of procedures per age group: paediatric, less than 18 years old; adult, 18–64 years old; and elderly, more than 64 years old.
Table I Participant characteristics and age-related outcome

Data are n (%) except where otherwise indicated. Paediatric group, age ≤ 16 years; adult group, age 17–64 years; elderly group, age ≥ 65 years. 5yFU = five-year follow up; TLC = time of last contact

Fig. 1 Pie charts showing the percentage of each patient group (paediatric, adult, elderly) that had previously undergone different types of ENT surgery. Numbers 1–6 indicate the number of previous operations for each ear.
Table II lists pre-operative and outcome parameters for the total cohort and the five-year follow-up group. The present cohort and that of Yung et al.Reference Yung and Smith 3 were similar regarding patient numbers, time for complete epithelialisation and dry ear rate. The present cohort had significantly more draining cavities prior to surgery compared with the cohort of Yung et al. (p < 0.05).Reference Yung and Smith 3 Residual and/or recurrent cholesteatoma was observed during surgery in 30 per cent of the current cohort.
Table II Outcome of revision radical cavity surgery with mastoid obliteration

Data are n (%) except where otherwise indicated. Pre-op = pre-operative; post-op = post-operative; 5yFU = five-year follow up; FU = follow up; peri-op = peri-operative
Canaloplasty and meatoplasty
Canaloplasty was performed in 50 per cent of all ears and meatoplasty in 27 per cent of all ears. There was no significant difference in dry ear and troublesome ear rates in patients who had additionally undergone canaloplasty only, meatoplasty only, canaloplasty plus meatoplasty or neither (Table III). However, there was a trend in favour of canaloplasty over no canaloplasty and/or meatoplasty in the dry ear group (p = 0.053).
Table III Dry ear rate by additional procedure

Data are n (%). *At 13–24 months of follow up.
Re-epithelialisation time
The average time to complete re-epithelialisation in the five-year follow-up group (eight weeks) was comparable to that of the cohort of Yung et al.Reference Yung and Smith 3
Complications and revision surgery
No major iatrogenic surgical complications such as dead ear, facial palsy or prolonged dizziness were observed. In four ears (3 per cent), the soft-tissue flap was trimmed in an out-patient setting because of tip necrosis. Revision surgery was needed in 15 ears (12 per cent): residual cholesteatoma (3 ears), eardrum perforation (4 ears), second look tympanoplasty (4 ears), meatoplasty (2 ears), canaloplasty (1 ear) and subtotal petrosectomy (1 ear). Subtotal petrosectomy was performed because a defect in the posterior canal wall resulted in loss of hydroxyapatite granules.
Dry ear rate
The presence of dry ear was scored pre- and post-revision radical cavity surgery with mastoid obliteration using the Merchant grading system (Table II).Reference Merchant, Wang, Jang, Glynn, Rauch and McKenna 7 Pre-operatively, 92 per cent of the total cohort had a chronically draining ear. Post-operative results in follow-up groups were stratified by the time of last contact (Table IV). Dry ear rates at 4–6, 7–12, 13–24, 25–36 and over 36 months were 100 per cent, 89 per cent, 100 per cent, 92 per cent and 90 per cent, respectively. Dry ear rates were 97 per cent at 5 years of follow up and 93 per cent for the total cohort. The dry ear rate was significantly lower in the elderly group at the time of last contact compared with the adult group (p < 0.05). There were no significant differences among the paediatric group, the adult group and the total cohort. There was no significant difference in dry ear rates between the total cohort and the five-year follow-up group.
Table IV Post-operative dry ear rate

*Using the grading system of Merchant et al.Reference Merchant, Wang, Jang, Glynn, Rauch and McKenna 7 Data are n (%). FU = follow up; 5yFU = 5-year follow up
Recurrent or residual disease
There was no cholesteatoma recurrence in the present cohort. Residual cholesteatoma was detected in three ears (2 per cent): 2 in the epitympanum, detected 29 and 35 months post-operatively; and 1 in the hypotympanum, detected 61 months post-operatively (Figure 1). One residual cholesteatoma was detected at a routine out-patient follow up. Follow-up diffusion-weighted MRI detected nine lesions suspicious for residual cholesteatoma: three were confirmed during revision surgery; one led to revision surgery but turned out to be fibrous tissue rather than residual cholesteatoma; and the other five were either refuted by otoscopic examination or are still being followed up. These different outcomes were due to cerumen along with some skin tissue in the ear canal, which could be cleaned easily. The cholesteatoma-free rates for ears in the present study were 98 per cent at three years and 97 per cent at five years. There were more residual cholesteatomas in the five-year follow-up group of Yung et al.Reference Yung and Smith 3 compared with the five-year follow-up group in the present study (4 vs 1), but the difference was not statistically significant (p = 0.086; Figure 2). In the present study, three inclusion cholesteatomas were enclosed by the tympanic membrane and could be removed otoscopically at the out-patient clinic.
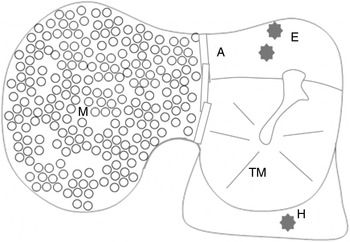
Fig. 2 Diagram showing the location of residual cholesteatomas (n = 3), indicated by grey stars. A = antrum; E = epitympanum; H = hypotympanum; M = mastoid (obliterated); TM = tympanic membrane
Discussion
Yung et al. included cases of both primary and revision surgery,Reference Yung and Smith 3 but the present study aimed to confirm the success of this technique in the most challenging population: patients with very troublesome cavities. The high percentage of discharging ears, the 33 per cent residual cholesteatoma rate and the average of more than two previous procedures indicate that the study cohort had very challenging ears. The primary surgical goal was to create a safe, dry ear. Since hearing improvement was not the primary goal, hearing results are not included in this article.
The proportion of female patients was similar in Yung and colleagues’ cohort and in the present study, but the former included a higher proportion of children.Reference Yung and Smith 3 However, as no significant difference was found between the paediatric and adult group in the present study, the results of both studies can be compared. The elderly group had a lower post-operative dry ear success rate, possibly due to compromised tissue healing in the older population. This contrasts with the data of Ahn et al. and Saito et al., who found no difference between young and elderly groups.Reference Ahn, An, Bae and Kim 11 , Reference Saito, Tanaka, Tokuriki, Shibamori, Yamamoto and Noda 12 Yung et al. reported a lower rate of pre-operative dry ear compared with the present study.Reference Yung and Smith 3 However, both studies had a similar approach to follow up, and similar numbers of patients were followed up for five years or more.
Given the variety of obliteration techniques, it is very difficult to decide which technique should be used for a specific patient attending a specific out-patient clinic. As previously done by Charachon et al. Reference Charachon, Gratacap and Tixier 13 , Solomons et al. Reference Solomons and Robinson 14 , Hartwein et al. Reference Hartwein and Hörmann 15 and Saunders et al. Reference Saunders, Shoemaker and McElveen 16 for the Palva flapReference Palva and Mäkinen 17 , the present study aimed to confirm the successful results of Yung et al.Reference Yung and Smith 3 Black et al. first described the use of a mid-temporal flap for reconstructing the posterior canal wall skin; for obliteration, they used the Palva or Popper flap.Reference Palva and Mäkinen 17 – Reference Popper 19 O'Sullivan et al. and Singh et al. also used a mid-temporal flap, but only for obliterating cavities.Reference O'Sullivan and Atlas 20 , Reference Singh and Atlas 21 Mahendran et al. used a mid-temporal flap for reconstructing the posterior canal wall, but only in one patient.Reference Mahendran and Yung 22 Yung et al. were the first to describe the use of this particular technique in a larger group of patients.Reference Choi, Cho, Lee, Lee, Chung and Hong 1 The group had used the surgical technique for 10 years before establishing the cohort for their study. The present study's cohort comprises the first 121 patients to undergo this surgical technique at this institution and therefore represents a learning curve. To identify which technique performs best, it is first necessary to determine whether the results are reproducible in different settings. Unfortunately, reported results are often heterogeneous, which prevents conclusions being drawn. The results in the present study were structured to allow comparison with those of Yung et al., and were indeed shown to be comparable.Reference Yung and Smith 3 This is consistent with previous reports that the technique can produce very good, reproducible results. The present data support the hypothesis that adequate meatoplasty and canaloplasty have additional beneficial effects in this type of surgery. This hypothesis was postulated by Berçin et al. for revision cavity surgery and also seems to be important when reconstructing the ear canal,Reference Berçin, Kutluhan, Bozdemir, Yalçiner, Sari and Karamese 23 as previously reported by the present authors.Reference Van Spronsen, Van Waegeningh, Geerse, Fokkens and Ebbens 24
The Merchant grading system (grades 0–3) was useful for both grading troublesome ears and making a straightforward distinction between wet and dry ears. The senior author has already reported the use of grade combinations (0 plus 1 and 2 plus 3) rather than individual grades,Reference Van Spronsen, Van Waegeningh, Geerse, Fokkens and Ebbens 24 and the same modified grading scheme was used in the current study to establish wet and dry ear rates. The dry ear rate in the total cohort was not significantly different from the rate described by Yung et al.Reference Yung and Smith 3 After five years of follow up, all patients in Yung and colleagues’ cohort had dry earsReference Yung and Smith 3 ; in the present study, one patient was still suffering from otorrhoea five years post-operatively. The present study used the Merchant grading system to score ear complaints and otoscopic abnormalities in a standardised way.Reference Merchant, Wang, Jang, Glynn, Rauch and McKenna 7 It is likely to be very difficult to compare results without using a standardised method for grading dry ears and a clear description of the grading method. For example, using the same grading system and combining grades 0 and 1, Singh et al. reported similar results to the first groups of follow up in the present study.Reference Singh and Atlas 21 However, they had poorer outcomes compared with the final outcomes for the total cohort and five-year follow-up group.
-
• Several reconstructive techniques have been described for troublesome cavities
-
• The present study used a modified technique to treat 121 patients (122 ears) with very troublesome cavities
-
• The dry ear rate and Merchant grades were recorded pre- and post-revision surgery
-
• In the five-year follow-up group, 97 per cent had dry ears after six minor revisions and 97 per cent were cholesteatoma free
-
• Of the total cohort, 93 per cent had dry ears after nine revisions and 98 per cent were cholesteatoma free
-
• This study successfully reproduced the good results of Yung et al.Reference Yung and Smith 3
The success rate for residual cholesteatoma in the present study was similar to the rate described by Yung et al.Reference Yung and Smith 3 More importantly, all residual cholesteatomas were restricted to the middle ear (Figure 1). Some surgeons are concerned about the possibility of residual cholesteatoma in an obliterated mastoid cavity; however, the present study does not support that concern and instead confirms the safety of obliteration techniques.
Conclusion
In a cohort with challenging cavities, the obliteration technique achieved very satisfactory results regarding long-term dry ears, long-term management of residual cholesteatomas and time to complete re-epithelialisation. Successful reconstruction of a new posterior canal wall with cartilage and a mid-temporal flap and obliteration of a cavity with hydroxyapatite granules reproduces the results of Yung et al.Reference Yung and Smith 3 The present study, which has a level of evidence 2B, is believed to be the first to confirm this technique in a large population of patients. Mastoid cavity obliteration was found to be safe because residual cholesteatoma only occurred in the tympanic region.
Acknowledgements
The authors thank Dr P G Mirck for his contribution in operating a substantial part of the cohort of interest for the current study.








