Introduction
The incidence of organised haematoma, which is a benign, non-neoplastic haemorrhagic condition, is increasing.Reference Kim, Oh and Kwon 1 Although it is a benign condition, organised haematoma develops in the nasal cavity and sinus, and induces bone thinning and destruction similar to malignant diseases. Therefore, organised haematoma is often mistaken radiologically as a malignant disease.Reference Choi, Seo, Rha and Kim 2 , Reference Unlu, Mutlu, Ayhan and Tarhan 3 However, the aetiology of organised haematoma is unclear.
Partial resection does not efficiently control organised haematoma that is growing.Reference Choi, Seo, Rha and Kim 2 , Reference Pang, Hu, Wang, Sha, Ma and Wang 4 , Reference Park, Ahn, Kwon do and Kwun 5 In addition, it is not easy to confirm organised haematoma, even with pathological diagnosis after complete resection. Complete surgical resection is recommended for the diagnosis and treatment of organised haematoma.
Although organised haematoma mainly arises from the maxillary sinus, maxillary organised haematoma is usually resected with: surgery using a Caldwell–Luc approach,Reference Choi, Seo, Rha and Kim 2 , Reference Yagisawa, Ishitoya and Tsukuda 6 – Reference Tabaee and Kacker 9 lateral rhinotomy,Reference Unlu, Mutlu, Ayhan and Tarhan 3 , Reference Yoon, Kim and Cho 10 a Denker's operation,Reference Yagisawa, Ishitoya and Tsukuda 6 , Reference Lee, Park and Heo 11 , Reference Song, Jang, Chung and Lee 12 or endoscopic surgery with canine fossa approaches.Reference Choi, Seo, Rha and Kim 2 , Reference Pang, Hu, Wang, Sha, Ma and Wang 4 In recent years, a purely transnasal endoscopic approach has been employed.Reference Choi, Seo, Rha and Kim 2 , Reference Pang, Hu, Wang, Sha, Ma and Wang 4 , Reference Kim, Kim, Chung, Dhong, Kim and Yim 7 , Reference Yoon, Kim and Cho 10 , Reference Song, Jang, Chung and Lee 12 , Reference Suzuki, Inaba, Hiraki, Hashida, Wakasugi and Kadokawa 13 This is because of the potential complications associated with the aforementioned procedures, which include post-operative facial numbness, tooth numbness, facial tingling and other adverse phenomena.Reference DeFreitas and Lucente 14 – Reference Byun, Lee and Baek 17 However, it is very difficult to resect organised haematoma in the maxillary sinus with an endoscopic approach alone, especially in the anterior, inferomedial or lateral regions of the maxillary sinus, even if wide middle meatal antrostomy is performed with a microdebrider.Reference Choi, Seo, Rha and Kim 2 , Reference Pang, Hu, Wang, Sha, Ma and Wang 4 , Reference Suzuki, Inaba, Hiraki, Hashida, Wakasugi and Kadokawa 13 , Reference Tanna, Edwards, Aghdam and Sadeghi 18 – Reference Robey, O'Brien and Leopold 20 Furthermore, organised haematoma develops anteriorly, inferomedially and laterally, with bone thinning, and adhesions occur. Considering this, the development of a safer and more effective endoscopic approach is needed for resecting organised haematoma in the maxillary sinus.
We recently reported a new method, modified transnasal endoscopic medial maxillectomy, which involves an approach through the anterior side of the nasolacrimal duct.Reference Suzuki, Nakamura, Nakayama, Inagaki, Murakami and Takemura 21 This is a safe and effective way to obtain wide and straight access to the maxillary sinus for the resection of inverted papilloma. With this approach, the nasolacrimal duct and the inferior turbinate can be preserved, and direct access to the maxillary sinus can be achieved through the anterior side of the nasolacrimal duct.
This report presents the clinical features of patients with organised haematoma in order to elucidate disease state. It also describes cases in which this approach was successfully employed as an alternative for the resection of organised haematoma in the maxillary sinus, enabling a better view and more space for resection with straight endoscopes and instruments.
Materials and methods
Patients at our hospital with pathologically proven sinonasal organised haematoma, treated between January 2006 and November 2015, were included in this study. Pre-operative data from the nasal endoscopic examination, computed tomography (CT), magnetic resonance imaging (MRI) and biopsy were evaluated. Post-operative outcomes were also assessed. The university ethics committee approved the study.
Surgical procedure
Modified transnasal endoscopic medial maxillectomy was performed to resect organised haematoma in the maxillary sinus (Figure 1a). First, a purely transnasal endoscopic method was applied through the middle meatus and ostium, from the posterior side of the nasolacrimal duct. Modified transnasal endoscopic medial maxillectomy was employed when patients rejected an extranasal approach and when resection could not be performed with wide middle meatal antrostomy using a purely transnasal endoscopic approach.
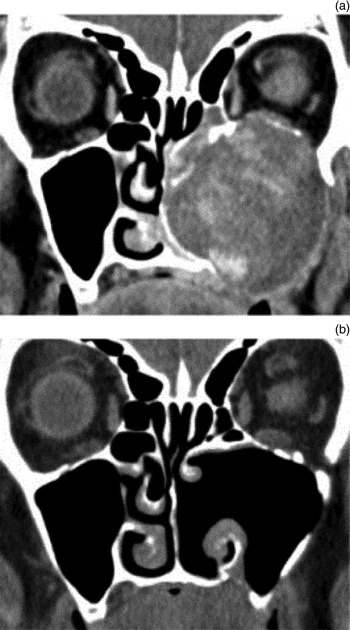
Fig. 1 Coronal sections of computed tomography (CT) scans of organised haematoma before (a) and after (b) modified transnasal endoscopic medial maxillectomy. Lateral development with bone thinning was observed on pre-surgery CT (a).
The operations were performed in accordance with the methodology for modified transnasal endoscopic medial maxillectomy that we previously reported for the resection of inverted papillomas.Reference Suzuki, Nakamura, Nakayama, Inagaki, Murakami and Takemura 21 An incision was made along the anterior margin of the inferior turbinate. After the lateral nasal mucosa was exfoliated (Figure 2a), osteotomy of the medial maxillary wall was performed, with conservation of the inferior turbinate and nasolacrimal duct (Figure 2b). The preserved inferior turbinate and nasolacrimal duct were shifted medially to enable wider access to the maxillary sinus.

Fig. 2 During modified transnasal endoscopic medial maxillectomy: (a) exfoliation of lateral nasal mucosa; (b) identification of the nasolacrimal duct and osteotomy of the medial maxillary wall; (c) identification of organised haematoma and entry to maxillary sinus from anterior to inferior turbinate; (d) exfoliation of organised haematoma; and (e) view of inferior turbinate and maxillary sinus after resection of organised haematoma.
After confirmation of organised haematoma in the maxillary sinus (Figure 2c), the capsule of the organised haematoma was separated from the maxillary sinus mucosa with a suction elevator (Figure 2d). Removal of the entire organised haematoma was performed with instruments (Figure 1b and 2e).
Results
Between January 2006 and November 2015, we treated 14 patients with pathologically proven sinonasal organised haematoma at our hospital. Two of the patients had recurrent organised haematoma. These two patients had undergone surgery using a primary endoscopic approach in other hospitals and visited our hospital when the organised haematoma recurred. One patient had undergone a Caldwell–Luc operation for the treatment of sinusitis about 30 years previously.
Patients’ features
The primary complaints were: nasal bleeding, in six patients; nasal obstruction, in four patients; double vision, in two patients; and cheek pain, in two patients (Table I).
Table I Patients’ features

Y = years; M = male; R = right; F = female; L = left
The mean age of the patients was 51.9 years, with a range of 22–87 years (Table I). There were eight men and six women (Table I). The sinonasal organised haematoma was on the right side in 8 of the 14 cases and on the left in 6 cases (Table I). One of the patients was a frequent flier and three patients had been in traffic accidents in the past.
Nasal endoscopic examination
All patients underwent nasal endoscopic examination. Bloody discharge was found in 7 of 14 patients. Nasal polyps or polypoid mucosa was observed in six patients. Crusting was found in four patients and tumour-like lesions were found in three patients. Displacement of the lateral wall to the nasal septum was evident in two patients.
Computed tomography
All patients underwent CT (Figure 1a). Computed tomography provided important information on the characteristics of the lesions. Bone thinning or destruction was observed in all patients. Contrast-enhanced CT also showed heterogeneous enhancement in all patients, but no calcification was found. All patients had organised haematoma in the maxillary sinus. Organised haematoma of the nasal cavity was present in all patients, and organised haematoma of the ethmoid sinus was apparent in nine patients. Maxillary bone thinning or destruction was observed at the medial wall (14 patients), lateral wall (9 patients), upper wall (9 patients), inferior wall (6 patients), anterior wall (6 patients) and posterior wall (7 patients). The nasal septum was compressed and deviated in 7 of 14 patients.
Magnetic resonance imaging
Nine of 14 patients underwent MRI. T2-weighted images demonstrated heterogeneous, mixed hypointense, isointense and hyperintense signals in all patients. The T2-weighted images also showed hypointense peripheral rims surrounding the lesion in all nine patients. Contrast-enhanced T1-weighted images showed irregular enhancement in all patients.
Mucosal inflammation and sinus mucosa thickening, which were caused by the organised haematoma obstruction, were easily distinguished from organised haematoma on T2-weighted images. Magnetic resonance imaging provided important information on the extent of organised haematoma.
Pathological finding
Pre-operative biopsies are useful to exclude malignancy. Biopsies were performed for all patients because lesions could be observed in the nasal cavity in all patients. The biopsies showed pathological findings, such as fibrin, haemorrhage, necrotic tissue, vascularisation and vascular dilatation. Fibrin was seen in the biopsy results for 8 of 14 patients and haemorrhage was found in 7 patients, but no malignancy was found. However, a confirmed diagnosis of organised haematoma could not be obtained pre-operatively for all patients.
Treatment
Surgery is necessary as a first-line treatment to remove organised haematoma. A Caldwell–Luc approach was performed in 3 of 14 patients in this study. Three patients underwent an endoscopic approach with wide middle meatal antrostomy. In these three patients, neither bone thinning nor destruction were seen at the anterior, inferior or lateral walls of the maxillary sinus. In addition, there was no adhesion found in the anterior, inferior or lateral regions of the maxillary sinus in three patients. Bone thinning or destruction was observed in the anterior, inferior or lateral walls of the maxillary sinus in all eight patients who underwent a modified transnasal endoscopic approach (Figure 1a). Adhesions were also observed in the anterior, inferior or lateral regions of the maxillary sinus in all eight patients. All patients had a capsule surrounding the organised haematoma. No patients required a blood transfusion. Chief complaints and other symptoms disappeared in all patients after surgery.
Two patients, in whom organised haematoma recurred after an endoscopic approach with wide middle meatal antrostomy, underwent a modified transnasal endoscopic approach as a secondary operation. In one patient, the organised haematoma could not be resected completely. One year later, the remaining organised haematoma increased in size, with frequent nasal bleeding. In the other patient, organised haematoma recurrence was found by endoscope one year after surgery, and had increased in size two years later, with frequent nasal bleeding.
The follow-up period of the 8 patients who underwent modified transnasal endoscopic medial maxillectomy ranged from 4 to 70 months (mean, 31.6 months). The nasolacrimal duct and inferior turbinate were preserved in all patients (Figure 3a). The inferior turbinate remained unchanged, without atrophy, during follow up. Good ventilation of the maxillary sinus was observed after surgery (Figure 3b). Complications such as facial numbness, tooth numbness, facial tingling, lacrimation and eye discharge were not evident following surgery. In addition, there was no recurrence.

Fig. 3 Endoscopic view of the inferior turbinate (a) and the middle meatus (b) after modified transnasal endoscopic medial maxillectomy.
Dissection of the apertura piriformis and anterior maxillary wall was not necessary in any of the eight patients, although we previously reported that such dissection may be performed for the resection of inverted papillomas.Reference Suzuki, Nakamura, Nakayama, Inagaki, Murakami and Takemura 21 This suggests that dissection of the apertura piriformis and anterior maxillary wall is not necessary for the resection of organised haematoma, in contrast to the resection of inverted papillomas.
Discussion
Organised haematoma develops in the nasal cavity and the maxillary sinus, and causes severe symptoms such as recurrent nasal bleeding, cheek swelling, cheek pain and double vision. These symptoms are similar to those caused by malignant diseases. Therefore, organised haematoma is often mistaken as a malignant disease.Reference Choi, Seo, Rha and Kim 2 , Reference Unlu, Mutlu, Ayhan and Tarhan 3 To avoid misdiagnosis, determining the likelihood of organised haematoma, using nasal endoscopic examination, CT, MRI and pathological findings, is important.
Wu et al. reported that a hypointense outer rim on T2-weighted MRI led to a positive diagnosis of organised haematoma.Reference Wu, Ting, Borgie, Busaba, Sadow and Juliano 22 In this study, a hypointense peripheral rim on T2-weighted images was found in nine patients, suggesting that T2-weighted images are useful in determining organised haematoma. Although Wu et al. reported that pre-operative biopsy and CT do not provide helpful information for differentiating organised haematoma from neoplastic lesions,Reference Wu, Ting, Borgie, Busaba, Sadow and Juliano 22 contrast-enhanced CT showed heterogeneous enhancement in all patients in this study. Pre-operative biopsy also showed fibrin in 8 of 14 patients. These findings suggest that contrast-enhanced CT and biopsy are useful when determining the likelihood of organised haematoma.
Although it is difficult to confirm pre-operatively, organised haematoma can be suspected based on pre-operative CT, MRI and biopsy findings. It is necessary to determine the complete absence of malignant cells in the total removed specimen in order to confirm organised haematoma. Therefore, a microdebrider should be used as little as possible, as it is not easy to collect tissue resected by microdebrider. Even if tissue is collected when a microdebrider is used, the location of tissue is not clear and resection is piecemeal. Therefore, en bloc resection should be performed as much as possible for organised haematoma.
No patients required a blood transfusion in this study, although the chief complaint was nasal bleeding in six patients. Choi et al. reported that one patient, who underwent a Caldwell–Luc approach and endoscopic resection, required a blood transfusion because of intra-operative and post-operative bleeding.Reference Choi, Seo, Rha and Kim 2 Considering this, better visualisation and more space for manipulation is necessary.
Recently, transnasal endoscopic surgery has been applied in maxillary organised haematoma cases,Reference Choi, Seo, Rha and Kim 2 , Reference Pang, Hu, Wang, Sha, Ma and Wang 4 , Reference Yoon, Kim and Cho 10 , Reference Suzuki, Inaba, Hiraki, Hashida, Wakasugi and Kadokawa 13 because endoscopic management provides excellent magnification and there is no external incision. Resection of organised haematoma with an endoscopic approach alone has been performed through wide maxillary antrostomy, with an oblique endoscope and curved forceps/microdebrider. However, more than half of the maxillary sinus is not accessible through wide maxillary antrostomy, because over half (64 per cent) of the sinus is inferior to the lateral insertion of the inferior turbinate.Reference Tanna, Edwards, Aghdam and Sadeghi 18 It has also been indicated that the area localised laterally in more than one-third of the orbital floor cannot be managed using only a transnasal middle meatus approach.Reference Hinohira, Yumoto and Shimamura 19 Therefore, organised haematoma is sometimes resected through the inferior meatus in transnasal endoscopic surgery, although the area of the orbital floor that can be reached through the inferior meatus is 25–50 per cent, smaller than that reached through the middle meatus.Reference Robey, O'Brien and Leopold 20 Moreover, this access through the middle or inferior meatus does not give direct access to anterior lesions of the maxillary sinus. Considering the above, resection of organised haematoma in the anterior, inferior or lateral regions of the maxillary sinus is likely to be very difficult with a purely transnasal endoscopic approach.
Suzuki et al. described three cases of organised haematoma in the maxillary sinus.Reference Suzuki, Inaba, Hiraki, Hashida, Wakasugi and Kadokawa 13 The three patients underwent endoscopic sinus surgery. The lesions were curetted piecemeal via endoscopic middle meatal antrostomy, with the assistance of a microdebrider. The lesions were eradicated as thoroughly as possible, but tissue remained, particularly on the anterior and inferomedial walls in the sinus. The authors reported that this remaining tissue was eventually cured. However, two patients in the current study had recurrent maxillary organised haematoma after an endoscopic approach with wide middle meatal antrostomy. In both patients, the size of the organised haematoma increased, with frequent nasal bleeding, suggesting that radical resection is necessary for the control of organised haematoma. Choi et al. also reported that a female patient experienced recurrence five years later.Reference Choi, Seo, Rha and Kim 2 In addition, Park et al. reported a case in which organised haematoma continued to expand, and symptom aggravation and recurrent bleeding were observed, after an organised haematoma was only partially removed.Reference Park, Ahn, Kwon do and Kwun 5 They strongly recommended radical resection of organised haematoma with the surrounding capsule.
Lateral rhinotomy is one method to resect organised haematoma, specifically via open medial maxillectomy. An endoscopic medial maxillectomy called transnasal endoscopic medial maxillectomy, which includes the resection of the lateral nasal wall and the inferior turbinate, has been documented for the resection of inverted papillomas in the maxillary sinus.Reference Kamel 23 However, this approach has the disadvantage of sacrificing the inferior turbinate, which serves to warm and humidify inhaled air. The nasolacrimal canal, if not resected, prevents access to anterior lesions of the maxillary sinus. Therefore, modified transnasal endoscopic medial maxillectomy has been reported for the resection of inverted papillomas in the maxillary sinus.
Using modified transnasal endoscopic medial maxillectomy, it is possible to preserve the inferior turbinate and the nasolacrimal canal. The advantages of this approach include: (1) no external scar; (2) less buccal discomfort; (3) direct access to and management of the maxillary sinus through space anterior to the nasolacrimal duct, resulting in an easier operation with a straight endoscope and instruments; (4) easy management of anterior, inferomedial and lateral regions; and (5) easy post-operative observation with an endoscope.
The surgical procedure should be chosen depending on the size of the organised haematoma. An endoscopic approach with wide middle meatal antrostomy is considered the first-line treatment, although limitations exist. In this study, three patients underwent an endoscopic approach with wide middle meatal antrostomy. In these three patients, bone thinning or destruction, and adhesion, were not seen at the anterior, inferior or lateral walls of the maxillary sinus. However, there was bone thinning or destruction in the anterior, inferior or lateral walls of the maxillary sinus in all eight patients who underwent the modified transnasal endoscopic approach (Figure 1a). Adhesions were also observed in the anterior, inferior or lateral regions of the maxillary sinus in all eight patients, although adhesion of organised haematoma has not been reported on previously. It is difficult to separate adhesions in the anterior, inferior or lateral regions of the maxillary sinus by endoscopic approach with wide middle meatal antrostomy.
Hence, modified transnasal endoscopic medial maxillectomy should be considered in maxillary organised haematoma with bone thinning or destruction of the anterior, inferior or lateral walls. Modified transnasal endoscopic medial maxillectomy should be also considered in patients who have recurrent organised haematoma following an endoscopic approach with wide middle meatal antrostomy.
-
• Organised haematoma, a benign condition, often induces bone thinning and destruction, similar to malignant diseases
-
• Organised haematoma can be suspected based on computed tomography, magnetic resonance imaging and biopsy findings
-
• Surgery is necessary as a first-line treatment to remove organised haematoma
-
• An endoscopic approach with wide middle meatal antrostomy is useful for organised haematoma resection, but limitations exist
-
• Modified transnasal endoscopic medial maxillectomy is useful for organised haematoma resection in selected patients
-
• Apertura piriformis and anterior maxillary wall dissection is not necessary for organised haematoma resection, unlike inverted papilloma resection
Additional dissection of the apertura piriformis and anterior maxillary wall was not necessary in any of the eight patients. This suggests that dissection of the apertura piriformis and anterior maxillary wall is not necessary for the resection of organised haematoma, in contrast to the resection of inverted papilloma.






