Introduction
Benign paroxysmal positional vertigo (BPPV) is a self-limiting peripheral vestibular disorder characterised by recurrent brief episodes of vertigo that last less than a minute.Reference You, Instrum and Parnes1,Reference Kao, Parnes and Chole2 The symptoms are precipitated with a change of head position because of otoconia displacement with respect to gravity. The pathology can involve any of the three semicircular canals but most commonly involves the posterior semicircular canal.Reference Messina, Casani, Manfrin and Guidetti3 Benign paroxysmal positional vertigo has been hypothesised to occur because of degeneration of otoconia. The otoconia are dense calcium carbonate nanocomposites embedded in the gelatinous matrix (composed of glycoprotein and glycosaminoglycan) of the otolithic organs. The recently discovered matrix proteins otolin-1 and otoconin-90 are the major core proteins of the otoconial matrix. These proteins constitute the structural framework of otoconia, maintain its integrity and assist with its physiological functions. Otolin-1 is a scaffolding glycoprotein restricted to the inner ear (especially the utricular or saccular maculae, semicircular canal cristae, organ of Corti and stria vascularis marginal cells).Reference Andrade, Lins, Farina, Kachar and Thalmann4–Reference Hołubowicz, Wojtas, Taube, Kozak, Ozyhar and Dobryszycki7
There has been a recent upsurge in research work involving the role of inner-ear proteins as diagnostic and prognostic serum biomarkers for various inner-ear diseases. In particular, there has been a focus on the significance of otolin-1 as a biomarker in BPPV and its correlation with the risk factors for BPPV, such as aging, osteoporosis, vitamin D deficiency and post-menopausal status.Reference Parham, Kuchel, McElhaney and Haynes8–Reference Yang, Gu, Sun, Li, Wu, Burnee and Zhuang11 Other inner-ear disorders that are being investigated with regard to the usefulness of inner-ear proteins as serum biomarkers include sudden sensorineural hearing loss, acoustic trauma and ototoxicity.Reference Parham, Sacks, Bixby and Fall5,Reference Doğan, Şahin and Kurtulmuş12,Reference Sun, Xuan, Zhou, Yuan and Xue13
Parham et al.Reference Parham, Sacks, Bixby and Fall5 found that one third of their patients with BPPV had serum otolin-1 values above the control group. However, the patients in the study by Parham et al.Reference Parham, Sacks, Bixby and Fall5 had their most recent episode of BPPV up to two years before the serum marker sampling. Nevertheless, their study established the blood–labyrinth permeability of otolin-1 and its potential as a biomarker for inner-ear disorders involving otolithic organs. In terms of pharmacokinetics, the temporal evolution of serum otolin-1 in humans still remains to be understood. In order to better characterise the serum level of otolin-1, we sought to test the hypothesis that there was a significant rise in circulating otolin-1 in patients presenting to us with an active episode of BPPV. The objective of the current study was to evaluate the serum otolin-1 levels in patients with active BPPV and to compare it to individuals without BPPV.
Materials and methods
This study was conducted in the Department of Otorhinolaryngology, All India Institute of Medical Sciences, New Delhi, India, at our tertiary referral centre and in association with the Department of Biochemistry, All India Institute of Medical Sciences, New Delhi, after approval from the ethical committee (approval number: IEC-506/05-10-2018, RP-14/2018).
The recruited individuals were assigned to the following two groups: (1) patients with active BPPV (patients with posterior semicircular canal BPPV; n = 40, recruited sequentially); and (2) a control group (healthy individuals without BPPV; n = 30, recruited randomly from consenting individuals without BPPV).
Inclusion and exclusion criteria
Adult male and female patients ranging from 18 to 75 years of age who provided their consent were included in the study. The exclusion criteria were: patients below 18 years or above 75 years of age; patients with active ear diseases, patients with a history of previous ear surgery, patients with hearing loss, and patients suffering from systemic diseases (such as hypertension, hyperlipidaemia, hypothyroidism, hyperparathyroidism, diabetes mellitus or cardiac diseases).
Diagnostic evaluation
The diagnosis of the posterior semicircular canal BPPV was made based on clinical history (intermittent and brief vertiginous episodes lasting less than 60 seconds and occurring secondary to change in head position with respect to gravity, without additional otologic complaints) and physical examination including the confirmatory positional manoeuvres (Dix–Hallpike manoeuvre). Otoscopy of the ears was carried out to exclude other local pathologies, and a complete neurotological examination was conducted. When appropriate, additional audiological tests including pure tone audiometry, impedance audiometry, brainstem evoked response audiometry and otoacoustic emissions tests were carried out to document hearing and to rule out a retrocochlear pathology. The testing was performed in patients with an acute episode of BPPV after stabilisation and before the patients were discharged from the out-patient department.
Assay procedure for serum otolin-1 levels
Human otolin-1 was assessed in serum samples by enzyme-linked immunosorbent assay (category number: MBS772738; MyBiosource, San Diego, California, USA), which employs the principle of biotin double antibody sandwich technology. A series of standards (solution containing a precisely known concentration of otolin-1) corresponding to 0, 50, 100, 200, 400, 600, 800 and 1000 pg/ml were used to prepare a standard graph.
The standards and samples were loaded onto antibody-coated plates, and the conjugate reagent was added to the wells, covered and gently shaken and was then incubated at 37°C for 60 minutes. After incubation, the plates were washed multiple times. The colour was developed by adding 50 μl of chromogen solution to the wells, mixed by gentle shaking and incubated for 15 minutes at 37°C away from light. After the incubation period, 50 μl of Stop Solution (MyBiosource, San Diego, USA) was added to each well to stop the reaction, and the absorbance (optical density) of the plate was measured at a wavelength of 450 nm. According to the concentration values of the standard solutions (with known values as mentioned above) and the corresponding optical density values, the linear regression equation of the standard curve was calculated, and according to the optical density value of samples, the concentration of the corresponding sample was calculated.
Statistical analysis
The data analysis was performed with Stata 14.0 (Stata Corp, Texas, USA) and presented as mean (± standard deviation (SD)), median, range and percentage. Categorical variables were compared using the chi-square or Fischer's exact test. Continuous variables following normal distribution were compared by using the independent t-test, and the data with skewed distribution were analysed using the Wilcoxon rank sum test (Mann–Whitney U test). A p-value of less than 0.05 was taken as statistically significant.
Results
A total of 70 individuals were recruited for the study (cases = 40, controls = 30). The demographic details (gender and age distribution) of the patients are presented in Table 1. The cases and controls were well matched for age (p = 0.9). The ratio of male to female patients with BPPV was 1:2.1.
Table 1. Demographic details of the individuals participating in the study

BPPV = benign paroxysmal positional vertigo
The analysis of serum otolin-1 levels showed the mean levels to be 236.2 pg/ml (± SD, 43.5; range, 189–370 pg/ml; median, 225 pg/ml) in the control group and 636.8 pg/ml (± SD, 203.4; range, 259–981 pg/ml; median, 602.5 pg/ml) in the BPPV group. The difference in the otolin-1 levels between the cases and the controls was statistically significant (p = 0.0000). The results are elaborated in Figure 1 and Table 2. The serum otolin-1 levels were significantly higher in the cases with BPPV compared with the controls when analysed separately with respect to the gender distribution (p = 0.0000).
Table 2. Details of serum otolin-1 values in the study population

*n = 14; †n = 16; ‡n = 30; **n = 13; §n = 27; #n = 40. The difference in the serum otolin-1 values between the two groups was statistically highly significant (p = 0.0000) when calculated for the entire cohort as well as separately for the male and female subsets. The difference in the serum otolin-1 values between the male BPPV patients and the female BPPV patients was not statistically significant. BPPV = benign paroxysmal positional vertigo; SD = standard deviation
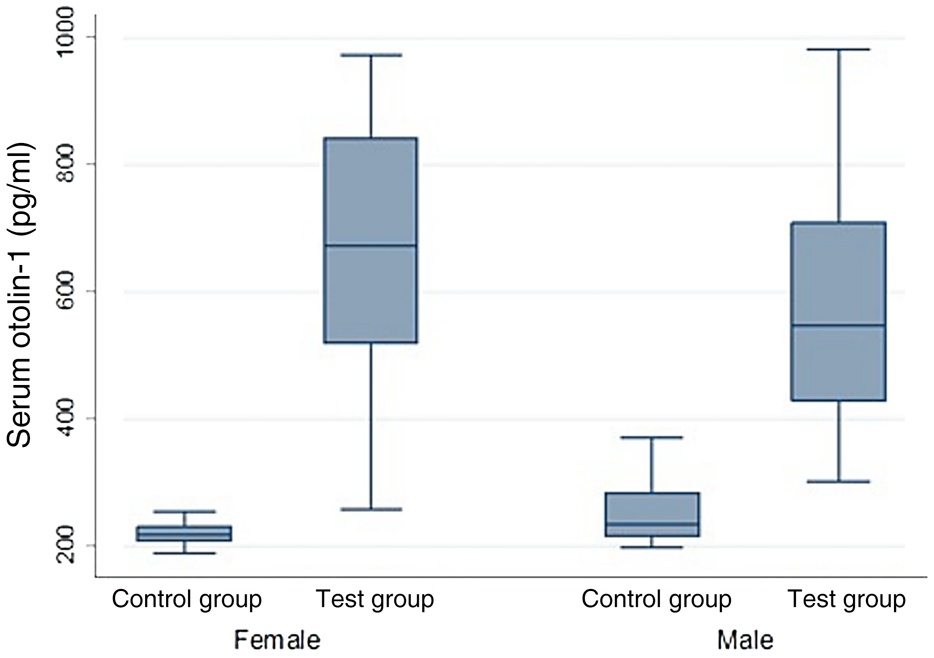
Fig. 1. Box and whisker plot showing the gender-specific comparison of serum otolin-1 levels between the patients with benign paroxysmal positional vertigo (BPPV; test group) and individuals without BPPV (control group). Horizontal lines at the end of the whiskers denote the range of serum otolin-1 (in picograms per millilitre), and the line within the box represents the median value. The median is significantly lower for the control group compared with the BPPV group for males as well as females.
Discussion
The use of biomarkers for inner-ear diseases is a relatively recent development and is an upcoming area of research being used to gain insight into inner-ear physiology. A biomarker for otoconial degeneration can be useful as a potential diagnostic modality. From a clinical perspective, biomarkers can enable prediction of disease, therapeutic targeting and monitoring of therapeutic response for the otoconial matrix, which is not well understood.
When there is an insult to the otoconial matrix, for example with the demineralisation of the calcium carbonate layer in BPPV, the scaffold protein otolin-1 is released from the bound state with the defragmentation of otoconia. Otolin-1 can cross the blood–labyrinth barrier and appear in the circulation.Reference Parham, Sacks, Bixby and Fall5,Reference Thalmann6,Reference Sacks and Parham10 The circulating otolin-1 can therefore be used as a serum biomarker to assess the diagnosis and therapeutic correlation in various inner-ear disorders.
The detection of circulating otolin-1 in humans was performed for the first time by Parham et al.Reference Parham, Sacks, Bixby and Fall5 in a study involving 24 patients (14 post-menopausal women with BPPV and 10 post-menopausal women without any history of otological disease). The authors found that otolin-1 could be identified in the serum of all the patients but was higher in patients with BPPV. Because otolin-1 is an inner-ear specific protein, the results supported the blood–labyrinth barrier permeability of the protein. The authors concluded that this protein can be used as a serum biomarker for BPPV to diagnose and assess therapeutic prognosis. Recently, Doğan et al.Reference Doğan, Şahin and Kurtulmuş12 studied the relationship between serum otolin-1 and acoustic trauma during mastoidectomy. The authors found raised levels of serum otolin-1 in the patients who had undergone operations, which correlated positively with the duration of bone drilling. Another recent study by Wu et al.,Reference Wu, Han, Yan, Lu, Zhou and Li14 performed on patients with active episodes of BPPV (both posterior canal and horizontal canal BPPV), showed the mean levels of serum otolin-1 in the patients to be significantly higher than the control population (324.55 pg/ml vs 259.54 pg/ml). A serum otolin-1 value of 299.45 pg/ml was shown to discriminate the BPPV patients from control patients with a sensitivity of 67.9 per cent and specificity of 72.7 per cent.
In the present study, the mean age of the participants was 46.7 years (± SD, 11.8; range, 24–68 years) and the ratio of male versus female BPPV patients was 1:2.1 (compared with nearly similar distribution (14:16) in the controls), suggesting female predominance of the disease. In general, the prevalence of BPPV is higher in female patients (male-to-female ratio = 1:2) as evidenced in the literature, especially in post-menopausal women, which is possibly because of hormonal influences.Reference Ogun, Büki, Cohn, Janky and Lundberg15
The level of serum otolin-1 in our patients with BPPV (mean, 636.8 pg/ml) was significantly higher than in the individuals without BPPV (mean, 236.2 pg/ml). When serum otolin-1 levels were compared for the gender-specific values between the two groups (BPPV patients vs the controls), the otolin-1 levels were significantly higher in the BPPV patients (both males and females) compared with the controls (though the male-to-female distribution in the two groups was dissimilar). However, the intra-group comparison between the male BPPV patients and female BPPV patients did not show a statistically significant difference (p = 0.33). There was an overlap in the serum otolin-1 values in the male subgroup between the control and BPPV cases (198–370 vs 301–981), whereas there was no overlap in the female subgroups in the two groups (189–254 vs 259–973). However, matching age and gender does not rule out overlapping in the range because it is possible there are factors other than gender and age at play.
Correlation between BPPV and osteoporosis has been investigated in multiple epidemiological studies.Reference Yu, Liu, Cheng and Wang16,Reference Yang, Kim, Lee and Park17 Benign paroxysmal positional vertigo has been shown to occur at a greater frequency (approximately 1.82 times in a nationwide study) in osteoporosis or osteopenia patients compared with those without osteoporosis.Reference Chan, Tsai, Yang, Chen and Chang18 Likewise, osteoporosis has been seen to occur more commonly in patients with BPPV (odds ratio, 1.29).Reference Lai19
Vitamin D has been proposed as a possible common link in the association of the two disorders, but the causation remains a matter of debate because there have been conflicting results in the literature regarding the role of vitamin D in the pathogenesis of BPPV.Reference Parham, Kuchel, McElhaney and Haynes8,Reference Karatas, Yuceant, Yuce, Hacı, Cebi and Salviz20–Reference Jeong, Kim, Shin, Kim, Lee and Lee22 Nevertheless, recurrent BPPV does seem to be associated with a negative vitamin D balance.Reference Rhim23,Reference AlGarni, Mirza, Althobaiti, Al-Nemari and Bakhsh24 Biomarker-based investigations can be used to unveil the pathophysiological correlates of inner-ear diseases. The causality between osteoporosis and BPPV was questioned by Sacks and Parham who carried out a biomarker-based comparison between BPPV (using otolin-1) and osteoporosis (using markers of bone turnover, N-terminal propeptide of type 1 collagen and N-terminal telopeptide of type 1 collagen). The authors found no relationship between the serum levels of biomarkers of BPPV and osteoporosis and concluded that although there is an association between BPPV and osteoporosis, it is not causal.Reference Sacks and Parham10
The prevalence of BPPV is higher in the geriatric population.Reference You, Instrum and Parnes1 For testing the hypothesis of age-related degeneration of otoconia, Tabtabai et al.Reference Tabtabai, Haynes, Kuchel and Parham9 studied otolin-1 levels in various age groups and found that the levels of otolin-1 were significantly higher in individuals more than 65 years of age compared with younger individuals. When compared with previously published data, they found that the values for their patients were much lower than the patients with BPPV and osteoporosis. They proposed a value of 300–350 pg/ml as the upper limit of normative otolin-1 values in their study, after excluding the outliers. Our patients were age-matched, and therefore the effect of age as a confounding parameter was removed from the analysis.
• Otolin-1 is a protein restricted to the inner ear with limited blood–labyrinth barrier permeability
• Serum otolin-1 has a potential to serve as a biomarker for inner-ear disorders
• Patients with posterior canal benign paroxysmal positional vertigo tend to have higher serum levels of otolin-1 compared with healthy individuals
The present study highlights that levels of otolin-1 are significantly raised in BPPV patients compared with controls. However, it is clear from the literature review that high levels of otolin-1 can be found in other conditions as well (osteoporosis or osteopenia, advanced age, vitamin D deficiency, acoustic trauma), which may be associated with increased risk of BPPV or inner-ear insult. Because the establishment of otolin-1 as a clinically reliable biomarker is still in the evolving phase, there is an unmet need for characterising the various temporal patterns of expression of the marker with varying disease activity and in various disease conditions affecting the inner ear (traumatic vs autoimmune) before its translation from the research domain to clinical practice. Further research in the area should focus on analysing the effect of various risk factors for BPPV (including vitamin D level and osteopenia or osteoporosis) on the patterns of otolin-1 expression in large patient cohorts and the temporal variation (acute vs chronic) in the levels of the marker in follow-up studies.
Conclusion
In our study, BPPV was seen to occur more commonly in female patients. The mean level of otolin-1 in patients with BPPV was found to be higher than in patients without BPPV. Within the BPPV group, the difference between the levels in males and females was not statistically significant. Further characterisation of otolin-1 in other inner-ear disorders and the conditions giving predisposition to BPPV should be addressed in future studies.
Acknowledgements
I extend my sincere thanks to Research Section, All India Institute of Medical Sciences, New Delhi, for their support for this project and Ashish Upadhyay (Assistant Professor, Department of Biostatistics, All India Institute of Medical Sciences, New Delhi) for his support with the statistical analysis. This study was funded by the Research Section, All India Institute of Medical Sciences, New Delhi (project code: A–643, No. F.8-643/A-643/2018/RS, dated 15 November 2018).
Competing interests
None declared





