Introduction
Sudden onset sensorineural hearing loss (SNHL) is defined as a 30 dB loss in three consecutive frequencies occurring over less than 72 hours. It is most commonly idiopathic in nature, although there are numerous suggested aetiologies, including immune, vascular and infective causes.Reference Schreiber, Agrup, Haskard and Luxon1 Current guidelines suggest treating such patients with oral or intratympanic steroid therapies.
The American Academy of Otolaryngology – Head and Neck Surgery (AAO-HNS) published guidelines for the investigation, management and follow up of patients presenting with sudden SNHL in August 2012.Reference Stachler, Chandrasekhar, Archer, Rosenfeld, Schwartz and Barrs2 In 2019, they published an update to this original guidance.Reference Chandrasekhar, Tsai Do, Schwartz, Bontempo, Faucett and Finestone3 ENT-UK have also recently published guidance on this area.4 It is suggested, through these guidelines and the literature, that patients should initially be treated with a course of oral steroids following sudden SNHL. This is typically 1 mg/kg (maximum of 60 mg) for 7 days, followed by a tapering dose for a further 7 days. The AAO-HNS guidelines recommend that patients who have incomplete recovery from sudden SNHL should be offered salvage intratympanic steroids. ENT-UK guidance states that if there is no improvement from oral steroids after 7–14 days, salvage intratympanic steroid injection therapy should be considered.
As a direct result of the AAO-HNS guidelines, an ENT department instigated salvage intratympanic steroid injection therapy. This study followed the results of this treatment, in a real-world scenario within a busy teaching hospital, to provide a UK perspective on the benefits of this regimen. We hope this will educate other departments as to how we instigated this service and the initial results obtained.
Materials and methods
Ethical considerations
A retrospective case series of consecutive sudden SNHL cases treated with salvage intratympanic steroid injection was undertaken, registered and approved by our hospital's audit and clinical research department (approval number: 4817).
Service's technical and logistical details
As detailed in Figure 1, our department reviews patients within 72 hours of onset for an audiogram and assessment. If patients are deemed to have sudden SNHL, they are given oral prednisolone. Two weeks later, audiometry is repeated within an emergency clinic. If hearing thresholds have not improved by an average of 30 dB relative to the unaffected ear, patients are offered intratympanic steroid injection therapy. This constitutes three intratympanic steroid injections, of 0.4–0.8 ml of 40 mg/ml methylprednisolone, injected into the middle ear through a phenol-anaesthetised tympanic membrane segment, with patients placed in a recumbent position facing away from the affected side and asked not to swallow for 30 minutes.

Fig. 1. Protocol in use between 2015 and 2019 for sudden sensorineural hearing loss (SNHL) treatment. PPI = proton pump inhibitor; ITS = intratympanic steroid; TM = tympanic membrane; MRI = magnetic resonance imaging; IAM = internal acoustic meatus
Injections are undertaken in a specialty doctor-run minor operations clinic, which runs for half a day each week, allowing up to four injections per session. Injections are given a week apart. After six weeks, a final pure tone average (PTA) is performed to qualitatively assess changes in hearing. Magnetic resonance imaging is conducted to exclude retrocochlear pathology.Reference Spear and Schwartz5
Study design
Patients seen in the ENT minor procedures clinic between June 2015 and December 2019, who were receiving salvage intratympanic steroid injection therapy for sudden SNHL, were identified from the examination of clinic records, coding records and patient notes. All patients fulfilled the criteria for sudden SNHL and completed treatment within an eight-week timeframe. This yielded 38 patients, 32 of whom were included, with 6 patients being excluded because of incomplete notes. Data were anonymised throughout.
Average PTA values were calculated as a mean of four frequencies (0.5, 1, 2 and 4 kHz). The PTAs were compared before and after oral and intratympanic steroid injection treatment, with final PTAs undertaken six weeks following the last intratympanic steroid injection. Speech audiograms were not routinely available for patients on this emergency pathway. We acknowledge this as a limitation to the study.
Hearing recovery was assessed using the standardised format detailed by Gurgel et al.Reference Gurgel, Jacklet, Dobie and Popelka6 ‘Complete recovery’ was defined as a return of hearing to within 10 dB of the unaffected ear. ‘Partial recovery’ was defined as a greater than 10 dB gain in hearing on the affected side but not returning to within 10 dB of the unaffected ear. This outcome was then further sub-categorised according to whether the ear was rendered serviceable or not. ‘No recovery’ was defined as less than a 10 dB improvement in the affected ear.
Statistical analysis
Data were collected from patients’ physical notes, and were analysed using Excel spreadsheet software (Microsoft, Redmond, Washington, USA) and GraphPad Prism 7 statistical analysis software (GraphPad Software, La Jolla, California, USA).
Results
This study included a total of 32 patients, comprising 18 females and 14 males, with a mean age of 61 years (range, 25–87 years). Hearing loss was right-sided in 14 patients, left-sided in 17 patients and bilateral in 1 patient. No autoimmune cause was identified for the patient presenting with bilateral sudden SNHL.
The incidence of sudden SNHL in this study, for 2019, was 9 per 100 000, in keeping with the reported incidence of 5–27 per 100 000 outlined in the 2012 AAO-HNS guideline.Reference Stachler, Chandrasekhar, Archer, Rosenfeld, Schwartz and Barrs2
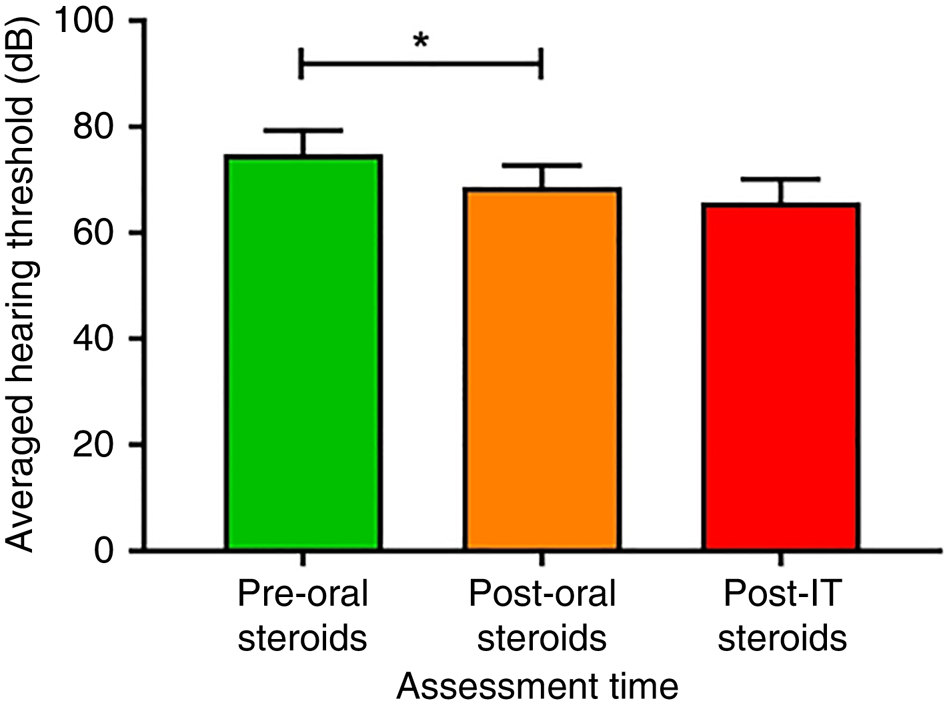
Table 1 and Figure 2 reveal mean averaged hearing thresholds (on the affected side), at presentation, of 74.8 ± 25.6 dB (range, 35–120 dB). Following oral steroid therapy, mean averaged thresholds were 68.6 ± 23 dB (range, 30–108 dB). This resulted in a mean averaged threshold improvement of 6.2 dB (range, −13.8–33.8 dB) following oral steroid therapy, which was found to be statistically significant (p < 0.05). Mean averaged thresholds following intratympanic steroid injection were 65.7 ± 25.1 dB (range, 22–120 dB), demonstrating a mean average threshold improvement of 2.9 dB (range, −22.5–61.3 dB). This mean improvement was not deemed to be statistically significant.

Fig. 2. Mean averaged hearing thresholds (for 0.5, 1, 2 and 4 kHz) before and after treatment. *Indicates significant difference. IT = intratympanic
Table 1. Mean averaged hearing threshold data pre- and post-treatment

SD = standard deviation
Figure 3 shows the sub-analysis results for hearing thresholds before and after oral steroids, and after intratympanic steroid injection, based on initial hearing thresholds at presentation (less than 70 dB or over 70 dB). These graphs display individual patient trends.

Fig. 3. Mean averaged hearing thresholds (for 0.5, 1, 2 and 4 kHz) before and after treatment, according to severity of hearing loss at presentation: (a) average presenting threshold of 30–70 dB, and (b) average presenting threshold of over 71 dB (representing severe idiopathic sudden sensorineural hearing loss). *Indicates significant difference. IT = intratympanic
Using the standardised criteria reported by Gurgel et al.,Reference Gurgel, Jacklet, Dobie and Popelka6 where the hearing thresholds of the unaffected side are used as a comparison for potential recovery, 3 patients (12 per cent) had complete recovery, 3 patients (12 per cent) had partial recovery and 19 patients (76 per cent) had no recovery following intratympanic steroid injection. This therefore gave a combined recovery rate for salvage intratympanic steroid injection therapy of 24 per cent. This analysis was undertaken in 25 out of 32 patients in the study, where unaffected hearing threshold data were available.
Discussion
Synopsis of new findings
The results revealed a limited clinical benefit of intratympanic steroid injection, with a mean improvement of only 2.9 dB. There is some evidence of individual patients having more marked improvements, but it was difficult to identify the favourable prognostic factors to target these patients, although it is likely to be those with hearing worse than 70 dB on presentation.
Study strengths and comparisons with other studies
This study represents a real-world experience of sudden SNHL for which salvage intratympanic steroid injection therapy was utilised. The mean average threshold improvement following intratympanic steroid injection therapy of 2.9 dB in this study is significantly lower than expected based upon other studies. A control study conducted in 2006, by Xenellis et al., demonstrated that hearing improved by 14.9 dB with intratympanic steroid injection therapy, compared to a deterioration of 0.8 dB in the control group who had no treatment.Reference Xenellis, Papadimitriou, Nikolopoulos, Maragoudakis, Segas and Tzagaroulakis7 The authors recommended intratympanic steroid injection as a safe and effective treatment.Reference Xenellis, Papadimitriou, Nikolopoulos, Maragoudakis, Segas and Tzagaroulakis7 A limited meta-analysis by Spear and Schwartz (based on 32 studies) revealed a mean improvement of 13.3 dB for intratympanic steroid injection salvage treatment versus placebo.Reference Spear and Schwartz5
Recent AAO-HNS guidelines also state that most studies show improvement in hearing following intratympanic steroid injection.Reference Chandrasekhar, Tsai Do, Schwartz, Bontempo, Faucett and Finestone3 All five of the randomised, controlled trials referenced used the latest AAO-HNS recommended paradigm of at least four injections over two weeks, within two to six weeks of symptom onset. This is a slightly accelerated protocol in comparison to the three injections over three weeks utilised in this study, mainly because it was based on guidance published prior to this recent 2019 update, perhaps contributing to the greater improvements in hearing recovery. The mean length of time in this study between the first oral steroid dose and the first intratympanic steroid injection was 17.4 days.
• This retrospective case series investigated patients presenting with idiopathic sudden sensorineural hearing loss
• It examined the role of salvage intratympanic steroid injections in these patients following poor response to initial oral steroid treatment
• Pure tone thresholds were reviewed before treatment, after oral steroid therapy and six weeks after intratympanic steroid injections
• After oral steroid therapy alone, mean average threshold change was 6.2 dB HL, statistically significant in severely affected patients (average presenting threshold of over 71 dB)
• Mean average threshold improvement after intratympanic steroid therapy was 2.9 dB (not statistically significant)
• Some patients experienced moderate improvement following intratympanic steroid therapy, but no specific subgroup benefitted more
Clinical applicability
This study showed salvage intratympanic steroid injection therapy to be effective in a minority of patients (15–24 per cent); however, for these patients it represents a final attempt at treating sudden SNHL. Intratympanic steroid injection therapy can be uncomfortable for patients and can sometimes provoke feelings of dizziness post-procedure. The procedure itself is known to carry a small risk of tympanic membrane perforation. In this study, only one patient was documented to have evidence of tympanic membrane perforation six weeks following intratympanic steroid injection.
This study provides further evidence of a trend towards greater improvement being more likely in those with a greater degree of hearing loss. It offers valuable real-world experience that will enable balanced discussion with the patient regarding the likely risks and benefits of salvage intratympanic steroid injection therapy. Additionally, this study will guide future departmental decision-making regarding our management of sudden SNHL. This may involve implementing a more accelerated intratympanic steroid injection regimen or selectively offering intratympanic steroid injection therapy only to those with more severe hearing loss.
Limitations
The inaccessibility of speech audiograms in this study limits the ability to formally assess functional hearing recovery amongst the sample population.
Data availability statement
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Competing interests
None declared