Introduction
Sore throat is a common symptom associated with acute upper respiratory viral infection or common cold. Most cases of sore throat cause only minor disturbance and are self-medicated with commonly available medicines such as analgesics, throat lozenges and antiseptic gargles. However, in some children and young adults sore throat may be associated with recurrent tonsillitis.
The clinical guidelines for tonsillectomy in both the UK and USA use the incidence of sore throat or throat infection as an indication for tonsillectomy.1, Reference Baugh, Archer, Mitchell, Rosenfeld, Amin and Burns2 It is therefore important to better understand the mechanism of sore throat and throat infection, and the involvement of tonsillar tissue. This review will provide basic information for the clinician about the pathophysiology of sore throat by discussing the causes and mechanisms of sore throat, with special reference to tonsil involvement.
Literature review approach
This was not a systematic review as there was no research question to study. The review instead aimed to provide basic information for the clinician about the mechanism of sore throat. As such, this review covered a range of fields, with information about anatomy, microbiology, neurophysiology, pharmacology and molecular biology.
Causes of sore throat
Sore throat associated with tonsillitis is most commonly caused by viral or bacterial infections. Fungal infections may also cause sore throat but these are usually associated with previous antibiotic therapy or conditions such as diabetes that affect immunityReference Chan3 and will not be discussed further.
Viral infections are by far the most common cause of sore throat.Reference Chan3 The respiratory viruses that cause common cold and flu symptoms are common causes of sore throat.Reference Eccles4 These include rhinovirus, corona virus, adenovirus, parainfluenza, influenza, respiratory syncytial virus, Coxsackie virus, bocavirus and metapneumovirus.Reference Weber, Eccles and Webber5 Other viruses that cause sore throat include herpes simplex virus, Epstein–Barr virus and human immunodeficiency virus.Reference Bisno6
There are several hundred different viruses responsible for sore throat, with more than 100 serotypes of rhinovirus. The list of common cold viruses continues to grow, with metapneumovirus identified in 2001 and human bocavirus discovered in 2005.Reference Weber, Eccles and Webber5 Common colds occur at a rate of 2–5 per person per year in adults, and schoolchildren (aged 9–11 years) have a higher rate with 7–10 colds per child per year.Reference Johnston, Holgate, Myint and Taylor-Robinson7 If only a fraction of these colds are accompanied by a severe sore throat, the high incidence of colds means that viral sore throat is a very common condition. This is reflected in the fact that sore throat (acute pharyngitis) is one of the most common illnesses for which patients visit primary care physicians in the USAReference Bisno6 and in the UK.Reference Chan3
Certain viruses may have a special role in causing tonsillitis because they infect immune cells such as lymphocytes. Adenoviruses, as the name implies, were initially believed to have a special role in infecting adenoid tissue, but it is now known that they infect a wide range of tissues, causing diseases as diverse as conjunctivitis and gastroenteritis.Reference Foy, Evans and Kaslow8 The Epstein–Barr virus is another virus that infects lymphocytes and is often associated with tonsillitis. The Epstein–Barr virus does have a special role in infecting the oropharynx but infection is not restricted to the tonsils; salivary tissue and lingual epithelium are also infected.Reference Niederman, Evans, Evans and Kaslow9
Bacteria commonly involved in causing sore throat include: various streptococci, Corynebacterium diphtheriae, Neisseria gonorrhoeae, Chlamydia pneumoniae and Mycoplasma pneumoniae.Reference Chan3 Group A streptococcus is reported to be the most common bacterial cause of sorethroat, accounting for approximately 15–30 per cent of cases in children and 5–10 per cent of cases in adults.Reference Chan3 These figures represent the incidence of bacterial infection in patients presenting to physicians; the incidence of bacterial infections as a cause of sore throat in the community is likely to be much less, as the majority of infections will be viral infections associated with common cold.
The presence of group A streptococcus in the throat does not mean that this is the cause of the sore throat. Group A streptococcus is a common commensal bacteria in the throat flora, and over 25 per cent of asymptomatic schoolchildren are carriers of group A streptococcus in the pharynx.Reference Ozturk, Yavuz, Kaya and Yucel10 The normal bacterial flora of the tonsils includes a range of bacteria such as Streptococcus salivarius, Streptococcus mitis, Streptococcus parvulus, Streptococcus constellatus, Streptococcus intermedius, and other species of bacteria such as enterobacteria, pseudomonas, and Klebsiella.Reference Ozawa and Sawamura11 The ecology of these different bacteria may be important with regard to the infection of tonsillar tissue, and the presence of any one bacteria species does not necessarily imply that it is causative in any infection of the tonsil.Reference Ozawa and Sawamura11 Indeed, the normal bacterial flora of the upper airways has been described as an important defence mechanism against infection.Reference Suzuki, Baba, Soyano and Kinoshita12
Sore throat may be caused by infection of tonsillar tissue, adenoids, eustachian tube orifice, posterior pharynx, uvula and soft palate. Inflammation in any of these areas will be perceived by the patient as a sore throat. The soreness or pain will be increased on swallowing, as inflamed tissues are physically stretched and slide over one another. Although sore throat is often described as pharyngitis, nasopharyngitis may be a more common cause of sore throat than pharyngitis as the nasopharynx is the first site of viral infection in common cold.Reference Gwaltney13 The tonsillar tissue in the adenoids and palatine tonsils is a common site of viral infection as these tissues contain intercellular adhesion molecule-1, which is the cellular receptor for 90 per cent of rhinovirus serotypes, and it is believed that common cold infections usually originate in tonsillar tissues.Reference Gwaltney13
It is difficult to predict the viral or bacterial cause of sore throat on a clinical basis.Reference Evans and Dick14 The Centor clinical prediction scoreReference Centor, Witherspoon, Dalton, Brody and Link15 is often used to assist diagnosis of a group A streptococcus infection, but even with the highest score, the likelihood of streptococcal infection varies between 25 and 86 per cent.1 In addition, the scoring system does not work well in the primary care setting where the prevalence of group A streptococcus infection is low.Reference Centor, Witherspoon, Dalton, Brody and Link15, Reference Aalbers, O'Brien, Chan, Falk, Teljeur and Dimitrov16
Inflammation and pain associated with sore throat
Inflammation associated with viral and bacterial infection of the upper airway is linked to the local generation of inflammatory mediators, such as prostaglandins and bradykinin, which act on sensory nerves in the nasopharynx and pharynx to cause sore throat.Reference Eccles4
Both intranasal and oropharyngeal administration of bradykinin cause a sensation of sore throatReference Rees and Eccles17 as a result of sensory nerve stimulation in the nasopharynx and oropharynx. It has been suggested that the early symptom of sore throat in common cold is due to the effects of bradykinin in the nasopharynx.Reference Rees and Eccles17 Intranasal challenge with prostaglandin 2 alpha and prostaglandin D2 has also been shown to elicit a sensation of sore throat.Reference Doyle, Boehm and Skoner18
Sore throat is caused by the inflammatory response to viral or bacterial infection. This inflammatory response is the result of a complex mix of inflammatory mediators, but the dominant mediators are bradykinin and prostaglandins.Reference Enna and Steranka19, Reference Sperber20 Bradykinin is a potent stimulant of pain nerve fibres and also causes vasodilation and increased capillary permeability resulting in tissue swelling.Reference Steranka, Manning, DeHaas, Ferkany, Borosky and Connor21
The immune response to tonsillar infection triggers the generation of a complex mix of cytokines. These cytokines are responsible for the systemic symptoms of infection, such as fever and mood changes, which are sometimes collectively referred to as the ‘sickness response’.Reference Eccles4, Reference Viamontes22, Reference Moon, McNeil and Freund23 Sickness behaviours such as malaise, lethargy and anorexia are driven by cytokines, and are an integral part of the sickness response initiated by immune cells.Reference Moon, McNeil and Freund23 The systemic cytokine response to tonsillar infection, and the associated sickness response, is important as it may be responsible for the patient missing days of school or work.
The sore throat pain associated with tonsillitis is assumed to originate in the adenoid and palatine tonsils. However, it is likely that the pain is due to a more generalised inflammatory response of all the lymphoid tissue in the upper airway that comprise Waldeyer's ring. The tonsils may be only one of the sites of inflammation associated with any viral or bacterial infection of the upper airway that causes sore throat. The inflammatory mediators generated by infection of the upper airway stimulate sensory nerves in the airway to cause the sensation of sore throat.
Sensory nerve supply to upper airway and sensation of sore throat
The anatomy and innervation of the tonsils has been described as constituting part of the anatomy of Waldeyer's ring.Reference Suarez24 Waldeyer's ring describes a ring of lymphoid tissue around the pharynx. It consists of the adenoid and palatine tonsils, and also includes lymphoid tissue around the opening of the eustachian tube (tubal tonsil) and lingual tonsils. In addition, there is some mucosa-associated lymphoid tissue between these tonsils.
The adenoid tonsils are innervated by sensory afferents from the pharyngeal branch of the maxillary division of the trigeminal nerve, and by the pharyngeal plexus of the glossopharyngeal and vagus nerves. The sensory innervation of the palatine tonsil stems from the lesser palatine nerves (from the maxillary branch of the trigeminal nerve) and from the glossopharyngeal nerve. The lingual tonsils consist of 30–100 irregular lymphoid follicles at the posterior third of the tongue dorsum. They receive their sensory innervation from the glossopharyngeal nerve and possibly from the superior laryngeal branch of the vagus nerve.
The sensation of sore throat is probably primarily mediated by the branches of the glossopharyngeal nerves, as disease processes limited to the oral cavity, which is mainly innervated by the trigeminal nerve, do not typically elicit a complaint of sore throat.Reference Chan3 Glossopharyngeal nerve block has been shown to reduce pain associated with tonsillectomy.Reference Park, Hwang, Park, Jeon, Bahk and Oh25 One cannot exclude contributions to the sensation of sore throat pain from the trigeminal and vagus nerves that supply the tonsillar tissue, but there is no evidence in the literature to support their involvement in sore throat pain.
Neurophysiology of sore throat
Apart from the specialised olfactory and gustatory receptors, the remaining sensory innervations of the upper airway consist of bare nerve endings without any specialised terminal receptors. The bare nerve endings serve as transducers for a wide range of stimuli, such as physical and chemical stimulation, changes in temperature and pressure, and stimuli that are associated with inflammation and infection that play a role in the sensation of sore throat.
The bare nerve endings of the upper airway mediate pain and temperature sensations that are modulated by transient receptor potential ion channels. The transient receptor potential channels were first described in 1969 having been observed in the fruit fly (drosophila) to modulate photoreceptor activity in the eye of the fly.Reference Cosens and Manning26 The first mammalian transient receptor potential receptor was discovered in 1997; this receptor was shown to modulate pain and temperature sensation induced by the pepper substance capsaicin (transient receptor potential vanilloid 1).Reference Caterina, Schumacher, Tominaga, Rosen, Levine and Julius27, Reference Story28 Since the discovery of transient receptor potential vanilloid 1, around 30 members of mammalian transient receptor potential channels have been cloned.
The transient receptor potential vanilloid 1 positive nerves innervate the entire respiratory tract, from the upper airways (nose, larynx and trachea) to lung parenchyma. These sensors play an important role in pain sensation.Reference Banner, Igney and Poll29 The ingestion of capsaicin has been shown to cause throat irritation, with the glossopharyngeal and vagal nerve endings responding more to capsaicin than the trigeminal nerves.Reference Rentmeister-Bryant and Green30 Although transient receptor potential vanilloid 1 is the most important and most studied transient receptor potential receptor involved in pain modulation, there are other receptors implicated in pain, such as transient receptor potentials ankyrin 1 and vanilloids 3 and 4. The reader is directed to recent reviews on this topic for the latest information in a rapidly moving field of research.Reference Chung, Jung and Oh31
Inflammatory mediators such as bradykinin and prostaglandins that are implicated in the mechanism of tonsillitis are known to act as sensitisers of transient receptor potential vanilloid 1.Reference Banner, Igney and Poll29 The fact that capsaicin – a natural plant substance – is a pain stimulant, has led to the search for endogenous biochemicals that naturally stimulate pain in response to inflammation. Bradykinin can activate phospholipase in sensory nerve endings and cause the formation of arachidonic acid metabolites.Reference Hwang, Cho, Kwak, Lee, Kang and Jung32, Reference Shin, Cho, Hwang, Jung, Shin and Lee33 These metabolites are known to trigger pain pathways. In addition, they have a similar three-dimensional structure to capsaicin, which indicates that they may be endogenous pain biochemicals.Reference Hwang, Cho, Kwak, Lee, Kang and Jung32 It has therefore been proposed that lipoxygenase products might be the natural capsaicin-like stimulus of the pain pathway.Reference Hwang, Cho, Kwak, Lee, Kang and Jung32, Reference Shin, Cho, Hwang, Jung, Shin and Lee33 A diagrammatic representation of some of the factors involved in sore throat pain is illustrated in Figure 1.
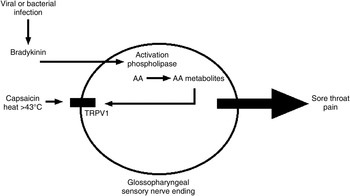
Fig. 1 Factors involved in the development of throat pain (as described in Neurophysiology of sore throat). AA = arachidonic acid; TRPV1 = transient receptor potential vanilloid 1
The transient receptor potential vanilloid 1 receptor is stimulated by capsaicin and by thermal stimuli above 43°C. Bradykinin is known to sensitise the transient receptor potential vanilloid 1 receptor so that it is activated at normal body temperature to cause the sensation of pain.Reference Chung, Jung and Oh31 This pain sensation may be increased by the calor (heat) of inflammation and will be reduced by cooling the inflamed tissue so that it is below body temperature. This could explain why ice treatments such as ice lollies are effective in relieving post-tonsillectomy sore throat pain.Reference Sylvester, Rafferty, Bew and Knight34 Ice treatments for tonsillectomy pain may work in two ways: firstly, by lowering the temperature of pain nerve endings and reducing the thermal activation of transient receptor potential vanilloid 1, and secondly, by activating transient receptor potential melastin 8 cold receptors. Transient receptor potential melastin 8 is a menthol receptor, which evokes a cool sensation when activated by temperatures below 25°C. Its activation has been shown to elicit analgesia in several different pain models.Reference Chung, Jung and Oh31 Transient receptor potential melastin 8 cold receptors will be activated by any cold stimulus in the mouth, such as ice lollies. It is interesting that menthol lozenges, which give a cool sensation in the mouth, are one of the most popular treatments for sore throat; the mechanism of their analgesic activity may be the activation of transient receptor potential melastin 8 receptors.
Prostaglandins such as prostaglandin E2 are important inflammatory mediators in infection and are responsible for some of the sore throat pain. Prostaglandin E2 has been shown to sensitise transient receptor potential vanilloid 1 receptorsReference Banner, Igney and Poll29 and may be the main mechanism underlying pain associated with infection. The inhibition of prostaglandin synthesis by analgesics such as paracetamol, ibuprofen and aspirin is one of the most effective treatments of sore throat pain.Reference Eccles, Loose, Jawad and Nyman35, Reference Eccles36
Role of tonsils in sore throat
The palatine and adenoid tonsils are situated at the entrances of the digestive and respiratory systems. They sample food and air for antigens associated with pathogens such as viruses, bacteria and fungi. The tonsils are part of Waldeyer's ring, the basic function of which is antibody formation against pathogens. The tonsils are small at birth and reach a peak size in children aged 4–8 years old, before regressing in size.Reference Akcay, Kara, Dagdeviren and Zencir37 The immune system components of Waldeyer's ring are still present in the adult, but the peak immune activity of this tissue appears to occur during early childhood when there is the initial exposure to common pathogens.
The tonsils may present a more common target for infection than the surrounding tissues of the upper airway because of the crypts that penetrate the tonsil. The squamous epithelium of the pharynx is less likely to be infected than the tonsil as it has a smooth surface that is lubricated with saliva containing antiviral and antibacterial biochemicals such as immunoglobulins and lysozyme. Chewing, swallowing and salivation mechanically cleanse the squamous epithelium of the pharynx and make it difficult for viral and bacterial attachment, whereas the crypts of the tonsils act as traps for ingested food and airborne materials that may contain pathogens. By serving as sampling organs for pathogens, the tonsils may become prime targets for upper airway infection, and tonsillitis is a common cause of sore throat.
Because of their pathogen sampling function, the tonsils are probably the most commonly infected site in the upper airway. However, removal of the palatine and adenoid tonsils does not prevent the symptom of sore throat, which demonstrates that these tissues form only a component of the upper airway tissues prone to infection.
Sore throat after tonsillectomy
The incidence of severe sore throat episodes is reduced after tonsillectomy, but severe sore throat may still occur. This indicates that tissues other than the tonsils may also cause sore throat pain. The Scottish Intercollegiate Guidelines Network states that tonsillectomy can prevent recurrent attacks of tonsillitis (which seems self-evident), but that tonsillectomy does not prevent recurrent sore throats due to other causes.1 The guidelines also stress that it is important to differentiate tonsillitis from ‘generalised pharyngitis’. However, the use of the term ‘generalised pharyngitis’ demonstrates our lack of understanding in the aetiology of sore throat, as one would expect generalised pharyngitis to also involve the tonsils and include tonsillitis.
Surgical removal of the adenoid and palatine tonsils will still leave much lymphoid tissue in the upper airway. Infection and inflammation of this remaining tissue is the most likely explanation for the occurrence of sore throat after tonsillectomy.
Discussion and conclusions
Sore throat is of special interest to otolaryngologists because severe recurrent episodes of sore throat may be treated by tonsillectomy. The term ‘sore throat’ implies a painful condition, and this review has focused on pain rather than other aspects of a throat infection such as hypertrophy of tonsils that may cause airway obstruction and sleep disorders. This review was undertaken because there is little information in the literature on the pathophysiology of sore throat and the mechanism of throat pain associated with tonsillitis.
Because of the role of the tonsils in sampling pathogens presented to the digestive and respiratory systems, it is inevitable that tonsillitis will be a common condition, especially during childhood. Respiratory infection is at a peak during childhood as the immune system interacts with large numbers of pathogens for the first time. Despite the common nature of sore throat, the mechanism of inflammation and pain associated with sore throat has not been specifically studied, but one can draw much information on these topics from the general literature.
Bradykinin and prostaglandins play an important role in the generation of inflammation and pain. The common and effective use of prostaglandin synthesis inhibitors (e.g. ibuprofen) in the treatment of sore throat supports a role for these mediators in sore throat pain.
Recent research has documented the importance of transient receptor potential vanilloid 1 receptors in the modulation of pain. This is a fast moving field that may soon give rise to a new generation of analgesics. The fact that transient receptor potential vanilloid 1 receptor activity may be modulated by changes in temperature is of specific interest to otolaryngologists who have traditionally used ice products to alleviate sore throat pain after tonsillectomy. The cold receptor transient receptor potential melastin 8 has also been shown to modulate pain, and it is again of interest to otolaryngologists that one of the most potent transient receptor potential melastin 8 agonists, menthol, has been used for over 100 years to treat sore throat pain. In 1890, the otolaryngologist Dr Frank Hamilton Potter recommended a throat spray containing menthol for treatment of sore throat, and concluded that ‘while menthol seems to be a drug with a future of great usefulness, it needs to be carefully studied and investigated’.Reference Potter38 Now, over 100 years later, we have only recently discovered the mechanism underlying the effects of menthol on pain.Reference Chung, Jung and Oh31



