Introduction
Treatment of frontal sinus fractures remains a clinical challenge. The primary goals of the treatment are closure of the cerebrospinal fluid (CSF) leak, achievement of an acceptable aesthetic result and prevention of any long-term complications. The overall wellbeing of the patient should, of course, also be taken into consideration. These fractures are frequently accompanied by many other injuries, requiring a multidisciplinary team approach and prioritisation of treatment.
There is a limited number of studies on the delayed complications of frontal sinus fracture repair,Reference Gonty, Marciani and Adornato1–Reference Chen, Chen, Mardini, Tsay and Chen4 and they do not report on complications as a result of a specific repair type.
Materials and methods
A retrospective chart review of patients with frontal sinus fracture admitted to our tertiary trauma centre from 2000 to 2017 was performed after obtaining institutional review board approval.
The study included patients with radiological follow-up of at least six months. Institutional policy for surgical treatment of frontal sinus fracture remained the same throughout the study period: anterior wall reconstruction for forehead deformity only, obliteration for nasofrontal outflow tract obstruction with or without forehead deformity, and cranialisation for posterior wall fracture with a CSF leak persisting for longer than a week after the trauma.
In order to identify a control group, we also collected data for patients treated non-surgically because of a poor general condition or because they did not meet the institutional computed tomography (CT) criteria for surgery.
Demographics and data on laterality of the frontal sinus fracture, presence of CSF leak, type of frontal sinus fracture management, and fixation technique were compiled. Documented late complications included chronic frontal sinusitis, mucocele formation, contour irregularity, and plate removal for palpability or visibility.
The primary outcome of the study was the rate of these late complications. The secondary outcome was the possibility of a correlation between the complications and the method of fracture repair. Given the small number of cases with complications, statistical analysis was not applicable.
This study was approved by the institutional review board, and all participants signed an informed consent agreement according to the guidelines of the Helsinki Declaration.
Results
During the study period, 338 patients with frontal sinus fracture were admitted to our facility. Seventy-seven of these patients were treated surgically and were available for early analysis of complications. The remaining patients were treated conservatively. Only four of them had long radiological follow-up. This cohort was not sufficient to serve as a control group; the corresponding data can be found in Table 1. Thirty patients met the inclusion criteria for long-term outcome analysis and late complications following surgery. The average follow-up duration was 37 months (range, 6–132 months).
Table 1. Long-term results of frontal sinus fracture management

Extent of frontal sinus fractures
The numbers of unilateral and bilateral fractures were equal. Posterior wall fracture was seen in 19 patients. In six of them, it resulted in CSF leak. Ten patients had nasofrontal outflow tract injury, as confirmed in the operating theatre.
Management
Frontal sinuses were reconstructed in 14 patients. Obliteration was performed in nine patients: two with bone, six with abdominal fat, and one with fat and pericranium. The obliteration technique was chosen by the attending surgeon. Seven patients underwent cranialisation. Only one frontal sinus with an injured nasofrontal outflow tract in our series was amenable to reconstruction. Titanium microplates (Synthes, Zuchwil, Switzerland) were used in 22 patients and the CranioFix clamp system (Aesculap, Tuttlingen, Germany) was used in 6 patients for fracture fixation. One anterior wall fracture was fixed with wire, and another was only approximated without rigid fixation following sinus obliteration. Cranioplasty with methyl methacrylate was used in the early period of our series in two cases of severe cranium loss.
Early complications
Although this study aimed to report on late complications and long-term outcomes, mention of the early complications is valuable. Two of the patients experienced an upper lid abscess after obliteration with abdominal fat (one and three months after surgery). Both patients who underwent reconstruction with methacrylate (one following cranialisation and the other following obliteration with fat) experienced allograft infection. The patient with a posterior wall fracture developed a frontal lobe abscess a week after obliteration with fat and pericranium. He underwent debridement and cranialisation with delayed reconstruction.
Late complications and long-term outcome
Twelve (83 percent) of the 14 patients who underwent sinus reconstruction regained aeration (Figure 1). Five of these patients had a posterior wall fracture. Ten years post-operatively, one patient developed a mucocele, and underwent marsupialisation into the patent frontal sinus and outflow tract. Another patient retained aeration in the reconstructed sinus, but entrapment of its mucosa through the sinus floor caused the development of an orbital mucopyocele, which consequently required removal of infected microplates and sinus obliteration five years following the previous surgery.

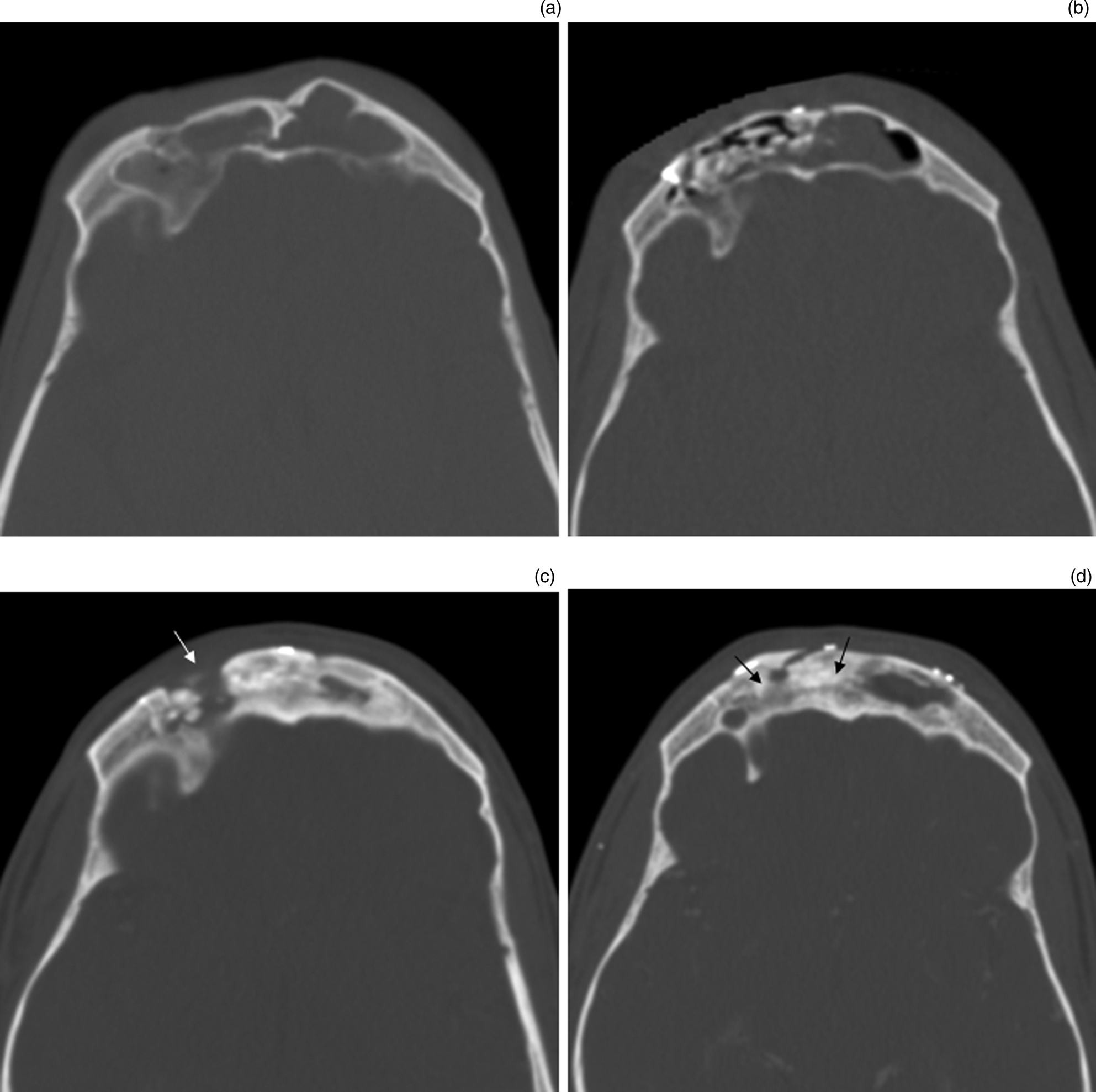
Fig. 1. Consecutive axial computed tomography images of a patient who suffered bilateral anterior wall frontal sinus fractures: (a) initial imaging after the accident before intervention (bilateral fracture of the anterior wall of the frontal sinus); (b) post-operative scan after obliteration with bone, and anterior wall repositioning and fixation with microplates, 3 days after the accident; (c) follow-up scan 3 years after obliteration, showing mucocele formation with bone resorption (white arrow); and (d) follow-up scan 2 years after re-obliteration with fat, showing partial ossification of fat (black arrows) and good external contour continuity.
Seven of nine patients had well-obliterated sinuses following primary obliteration. One patient, whose anterior wall fracture was not rigidly fixated after obliteration with fat, experienced forehead disfiguration due to bone resorption. A single patient was diagnosed with a mucocele three years after obliteration with bone and was successfully re-obliterated with fat (Figure 1). Seven patients who underwent cranialisation had an uneventful course. Of the entire study cohort, three patients (10 percent) developed mucoceles, all of which were successfully treated. The long-term results are summarised in Table 1.
Discussion
Rohrich and Hollier grouped complications following frontal sinus fracture repair into early complications (less than six months post-treatment) and late complications (more than six months post-treatment).Reference Rohrich and Hollier5 These time frames were used in the seminal paper published by Rodriquez et al., which reviewed their 26 years of experience in treating frontal sinus fractures. Taking into account the outcomes of these studies, we decided to adhere to the same definitions.Reference Rodriguez, Stanwix, Nam, St Hilaire, Simmons and Christy6
In our cohort of 77 patients there were 5 early complications: brain abscess in 1 patient a week after obliteration with abdominal fat and pericranium; upper lid abscess in 2 patients after obliteration with fat (one and three months after surgery); and methyl methacrylate allograft infection in another 2 patients. The latter required allograft removal and replacement with a calvarial bone graft. Based on this, we have concluded that the use of methyl methacrylate should be avoided in the management of frontal sinus fracture. The total rate of early complications in this series is 6 per cent, similar to that reported by Rodriguez et al.Reference Rodriguez, Stanwix, Nam, St Hilaire, Simmons and Christy6 and Strong et al.Reference Strong, Pahlavan and Saito7 These two studies, however, did not specifically address late complications.
Thirty of 77 patients underwent a follow-up CT at six months or longer after surgery. Our study is the first to report on long-term results as a function of repair type. As shown in the results section, 12 of 14 patients who underwent reconstruction regained sinus aeration, and 2 presented with a mucocele at 58 and 122 months after the reconstruction. Seven patients had the desired result at their most recent follow up after cranialisation. Seven of nine patients exhibited well-obliterated sinuses following obliteration. One of the two remaining patients developed mucocele 40 months following obliteration with bone, and was successfully re-obliterated with abdominal fat. Another patient experienced a cosmetic defect due to bone resorption. Anterior sinus wall fragments in this patient had been repositioned without rigid fixation. It is best to avoid this method.
Methodological considerations and limitations
The late complications in our series, similar to other frontal sinus fracture series, have to be evaluated carefully because these complications usually follow an indolent course. The fact that patients with a more complicated frontal sinus fracture and/or co-morbidities tend to continue follow up adds bias to our series, possibly indicating an even lower complication rate. However, one needs to be cautious in drawing such a conclusion, as mucocele formation and other complications can present many years after the injury. Suffice it to say that our follow-up period has its shortcomings.
Koudstaal et al. documented mucocele formation 35 years after frontal sinus trauma.Reference Koudstaal, van der Wal, Bijvoet, Vincent and Poublon2 They concluded that a lifelong awareness of this complication and appropriate patient education on the development of associated symptoms are needed.
• This study is the first to report long-term results of surgery for frontal sinus fracture as a function of repair type
• Half of the study cohort underwent frontal sinus reconstruction
• Of the remaining patients, similar numbers underwent either obliteration or cranialisation
• Average follow-up duration was 37 months (range, 6–132 months)
• Mucocele developed in 10 percent of patients, 40–122 months after surgery
• Anterior sinus wall fragment repositioning without rigid fixation should be avoided
In a series of 10 patients treated for frontal sinus fractures with long-term follow up, Fox et al. reported on a number of complications that we did not encounter in our series, including palpable hardware (e.g. plates and screws), altered sensation, frontalis weakness and headaches.Reference Fox, Garza, Dusch, Hwang and Girod3 We did not specifically address the issue of long-term headaches or pain, but it may be assumed that the patients presenting with mucopyoceles did have pain symptoms. Our series did not report any complaints of sensation loss or weakness of the frontalis branch of the facial nerve.
Only a few other studies specifically addressed long-term complications after frontal sinus fracture repair, all of which reported mucocele formation. Contour deformities and even recurrent CSF leaks were also reported in some cases (these were not experienced by any of our patients).Reference Fox, Garza, Dusch, Hwang and Girod3,Reference Chen, Chen, Mardini, Tsay and Chen4 Reviewing frontal sinus injury and complications, Metzinger et al. attributed immediate and delayed complications to disruption of the nasofrontal ostium or duct.Reference Metzinger and Metzinger8 Another possible limitation of our study is that all the cases were managed with an open approach. Grayson et al. reported on a single long-term complication (nasofrontal outflow tract obstruction) in a series of 46 transnasal endoscopic repairs of frontal sinus fractures with a mean follow up of 26 months (range, 0.5–79 months); however, their cohort lacked radiological follow up.Reference Grayson, Jeyarajan, Illing, Cho, Riley and Woodworth9
Acknowledgement
We are grateful to Mr Anton Zakharov for his generous help with language editing.
Competing interests
None declared