Introduction
Radiologically guided balloon dilatation of lower oesophageal strictures is common practice. However, other than some early reports from our own centre, little has been published regarding radiologically guided dilatation of pharyngeal and upper oesophageal strictures, and less still on radiological balloon dilatation of neopharyngeal strictures following total laryngectomy and pharyngolaryngectomy. For such strictures, bouginage under general anaesthesia is standard practice. However, balloon dilatation is less traumatic and can be performed under sedation.
Patients and methods
The study was approved by the St George's clinical ethics committee.
Table I shows details of patients’ age, sex, diagnosis, stage and treatment of malignant disease, balloon dilatation procedures and outcome, and follow up.
Table I Patient characteristics, procedures and results
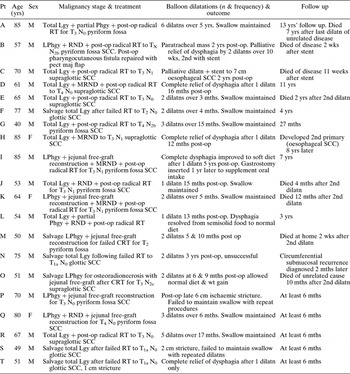
Lgy = laryngectomy; Phgy = pharyngectomy; LPhgy = laryngopharyngectomy; post-op = post-operative; RT = radiotherapy, T = tumour; N = node; dilatn = balloon dilatation; yrs = years; mths = months; wks = weeks; RND = radical neck dissection; MRND = modified radical neck dissection; SCC = squamous cell carcinoma; pect maj = pectoralis major muscle; CRT = chemoradiotherapy
This information was obtained from two sources.
Firstly, hospital episode statistics data were used to generate a list of patients who had undergone laryngectomy and/or pharyngectomy between 1989 (when hospital episode statistics data collection commenced) and 2006. During this period, 112 patients had undergone total laryngectomy, nine with total pharyngectomy and reconstruction with either free jejunum or tubed antero-lateral thigh free flap, and 18 with partial pharyngectomy. Fifteen of these 112 patients were identified as having undergone radiologically guided balloon dilatation of a post-operative pharyngeal stricture. These patients' case notes were reviewed. Information regarding these 15 patients is shown in Table I (patients A to O).
Secondly, a report of balloon dilatations of pharyngeal strictures undertaken between 1986 and 1992 was produced by our unit and published in 1993.Reference Rowe-Jones, George, Moore-Gillon and Grundy1 This report included dilatation undertaken for strictures with a variety of aetiologies, both benign and malignant. Of the 13 patients included in this report, six met the criteria for inclusion in the current study (i.e. balloon dilatation of neopharyngeal strictures in patients who had undergone laryngectomy). The remaining seven patients had undergone dilatation of the pharynx for strictures of other aetiology, or had undergone dilatation of a more distal site. One of these patients had also been identified by hospital episode statistics, and as such was included within patients A to O. Information on the remaining five suitable patients, obtained from the 1993 publication, is also included in Table I (patients P to T). These five patients were treated between 1986 and 1989.
Collectively, we identified 20 consecutive patients (patients A to T) with pharyngeal stricture and dysphagia following total laryngectomy or pharyngolaryngectomy who had undergone therapeutic balloon dilatation of the stricture under radiological guidance. These patients comprised 17 men and three women; their ages ranged from 40 to 84 years.
All patients were initially investigated with a barium study and direct pharyngoscopy at presentation with dysphagia, in order to elucidate the nature of the problem. Further barium studies and/or direct pharyngoscopy were not necessarily performed prior to all additional balloon dilatations, unless the behaviour of the stricture was noted to have changed during any subsequent dilatations, or a change was clinically suspected during follow up.
The main outcome – swallowing maintenance – was assessed at regular follow up. The patients were weighed and seen by a head and neck surgeon, oncologist, dietician, and speech and language therapist, as appropriate.
Balloon dilatation was performed under radiological guidance, using a conventional fluoroscopy unit. The patient's pharynx was anaesthetised with topical Xylocaine spray and the patient sedated with intravenous diazepam. Balloon catheters were passed orally, and the patient was asked to swallow to encourage passage. When necessary, a guide wire was passed prior to the catheter, and occasionally a steerable guide was used to negotiate particularly difficult strictures.
Two types of catheter were used: the Lunderquist–Owman dilatation system (William Cook Europe, Bjaeverskov, Denmark) and the Rigiflex Soft-Tip Microvasive (Milford, MA, USA). Both catheters had balloons 80 mm in length and 20 mm in diameter. Balloon inflation was carried out under fluoroscopic control, using a solution of Conray 280 (May and Baker, Melbourne, Australia) contrast medium at 50 per cent strength. Up to three inflations, of 30 seconds each, were performed until the initial banding at the stricture sight disappeared and the contour of the balloon was smooth. Patients remained nil by mouth for four hours after the procedure. Chest radiographs and contrast studies were not performed routinely after an uncomplicated dilatation.
Two patients had Nitinol stents (Ultraflex, Microvasive, Milford, MA, USA) inserted using a standardised technique.
Results
Five patients (D, H, J, L and T) gained relief from their dysphagia with one balloon dilatation only. All of these patients had undergone total laryngectomy, but without partial or total pharyngectomy. All had received radical doses of radiotherapy. None received chemotherapy. They were followed up for between four months and 11 years.
Nine patients required more than one dilatation in order to maintain swallowing so that per-oral dietary intake alone would be sufficient to increase or maintain weight (A, E, F, G, K, M, O, Q and R). The greatest number of dilatations administered was five, received over 17 months in one patient. Five patients required only two dilatations to maintain swallowing. One patient received six dilatations over six years.
One patient (I) had complete dysphagia, which failed to improve with surgical bouginage performed during initial assessment with direct pharyngoscopy. Balloon dilatation improved swallowing to allow a soft diet, and this level was maintained. A gastrostomy was inserted one year later to supplement this patient's oral intake.
Two patients (B and C) underwent balloon dilatation procedures and stent insertion for palliative relief of dysphagia due to known recurrent malignant disease.
Three patients failed to maintain swallowing despite repeat dilatations. One of these patient (S) underwent two balloon dilatations, to 20 and 17 mm, over a two-month period with some success. However, on the next two occasions (at weekly intervals) his stricture was difficult to dilate and response was poor. Another patient (P) underwent five dilatations to 20 mm over a five-month period, again with some benefit, but his stricture was very tight and tortuous and became difficult to negotiate. The third patient (N) was treated with balloon dilatation, ostensibly for benign disease following barium swallow and direct pharyngoscopy. Repeated direct pharyngoscopy and oesophagoscopy failed to show mucosal disease; however, subsequent computed tomography (CT) guided fine needle aspiration (FNA) analysis demonstrated circumferential submucosal recurrence.
No patients suffered any significant complications, such as perforation, related to the dilatation procedures.
Discussion
Dysphagia has been reported to occur in 16 per cent of patients who have undergone total laryngectomy.Reference Jung and Adams2 Approximately one-third of these cases are the result of a benign stricture.Reference Balfe, Koehler, Setzen, Weyman, Baron and Ogura3 Balloon dilatation offers distinct advantages for the treatment of oesophageal strictures, compared with bouginage: the symptom-free intervals are longer, it is well accepted by patients, and the rate of perforation is lower.Reference Starck, Paolucci, Herzer and Crummy4–Reference Hernandez, Jacobson and Harris6 Bouginage is considered to increase the likelihood of complications, as it produces a longitudinal shearing force up to seven times that applied in balloon dilatation.Reference McLean and LeVeen7 Balloon dilatation reduces the risk of perforation, since only readily controlled, transverse forces are applied.Reference Starck, Paolucci, Herzer and Crummy4 Balloon catheters are also better suited to negotiating tortuous strictures, and may be successfully applied to strictures not responsive or accessible to standard bougie techniques.Reference Whitworth, Richardson and Larson8
However, missing a malignant stricture would be an adverse event resulting in as much or more harm than a perforation. Contrast radiology may be helpful, but it is not as definitive as direct examination. In our unit, patients who presented with stricture were initially assessed with direct rigid endoscopy. Patients who responded to dilatation were followed up in a routine manner. Patients who developed new symptoms, such as increasing pain, delayed dysphagia or dysphagia at another level, underwent further investigation. For example, patient N presented with increasing dysphagia three years after his operation. Initial rigid endoscopy did not reveal a mucosal lesion. After he failed to respond to two balloon dilatations in short succession, further endoscopy was performed. Still, no mucosal lesion was seen. Computed tomography demonstrated a submucosal, circumferential recurrence, confirmed on FNA. Patient H developed a metachronous tumour eight years after initial laryngectomy. Balloon dilatation was performed for both benign stricture and palliation of dysphagia due to known recurrence. Vigilant, close follow up meant that there were no ‘missed’ or significant delays in the detection of recurrences in any of our patients as a result of our practice of radiologically guided balloon dilatation.
Balloon dilatation has been used in the management of strictures in many areas of the gastrointestinal tract.Reference Grundy9 Only eight reports of balloon dilatation of the pharynx have been published, four of which were from our centre.Reference Rowe-Jones, George, Moore-Gillon and Grundy1, Reference Whitworth, Richardson and Larson8–Reference Thornton, Conlon and Timon15
Vaghela and Moir described successful repeated hydrostatic dilatation of a benign pharyngeal stricture in a laryngectomy patient under local anaesthetic, without radiological guidance.Reference Vaghela and Moir14
The use of retrograde, endoscopic balloon dilatation to achieve oesophageal dilation under direct visualisation in patients with total, or near total, upper oesophageal stenosis (secondary to advanced head and neck cancer treated with combined chemotherapy and radiation) has been described by two separate groups.Reference Lew, Shah, Chalian, Weber, Williams and Kochman12, Reference Steele, Tokayer and Smith13 A gastrostomy is required for these techniques, in order to advance a flexible endoscope in a retrograde fashion to the distal edge of the stenotic segment.
Two patients in the current study underwent palliative balloon dilatation and subsequent stent placement for malignant stricture. The procedures were well tolerated and improved swallowing function. Thornton et al. placed stents in four laryngectomy patients: one with an inoperable malignant stricture and three with problematic benign strictures.Reference Thornton, Conlon and Timon15 However, the latter three stents had to be removed, as a result of pain in two patients and interference with prosthetic speech production in the third. The patient with inoperable tumour recurrence, who received a stent for palliative measures, tolerated the stent well until his death three weeks later. No other series, prior to the current study, has concentrated on balloon dilatation for laryngectomy patients.
• Dysphagia is common after laryngectomy
• One-third of such cases result from benign stricture
• Balloon dilatation may be performed under sedation to relieve dysphagia in post-laryngectomy patients
Perforation has been reported in up to 8 per cent of patients undergoing oesophageal bouginage with a rigid scope, and in 0.25 to 0.9 per cent with a flexible endoscope.Reference Bacon and Hendrix16–Reference Tulman and Boyce18 In comparison, oesophageal balloon dilatation is reported to cause perforation in 0 to 2 per cent of patients.Reference Rowe-Jones, George, Moore-Gillon and Grundy1, Reference McLean, Cooper, Hartz, Burke and Meranze19, Reference Maynar, Guerra, Reyes, Mayor, Garcia and Fascal20
The present study detected no serious adverse events following radiologically guided balloon dilatation. We previously reported a perforation rate of 1.8 per cent (one out of 55 dilatations).Reference Rowe-Jones, George, Moore-Gillon and Grundy1 This occurred in a patient who had not undergone laryngectomy. Grundy described two laryngectomy patients, included in the present series, who experienced severe reflex coughing during the dilatation, probably due to vagal excitation.Reference Grundy9
Conclusions
Radiologically guided balloon dilatation is minimally invasive and safe. It is well tolerated. It may be repeated frequently, and can successfully relieve strictures of the pharynx in patients who have undergone total laryngectomy or pharyngolaryngectomy.



