Introduction
Many surgeons are adopting an increasingly conservative approach to septal surgery, such that only the deviated portion of the septum is addressed by the surgery. A number of centres are practising endoscopic techniques to perform septal surgery. Following removal of the deviated cartilage or bony septum, a dead space exists. In order to reduce this dead space, and therefore reduce the risk of developing a septal haematoma, surgeons have used nasal packing and suturing techniques. Several suturing techniques have been described to approximate the mucosal flaps after septal procedures,Reference Sessions1–Reference Jan Beekhuis3 in order to reduce the complication rate. Many surgeons use interrupted sutures using absorbable suture materials to keep the flaps together. In 1984, SessionsReference Sessions1 reported continuous suture quilting, using 4.0 plain catgut on a small cutting needle to approximate the mucosal flaps. A similar technique using a curved needle was described by Lee and Vukovic.Reference Lee and Vukovic2
These techniques also help to close any mucosal tears and support the remaining cartilage. Many surgeons use suturing techniques to obviate the need for packing after surgery.Reference Sessions1 In addition, this suturing technique can be used to stabilise the middle turbinates during the healing process, preventing early lateralisation of the turbinate with adhesion formation.
We describe a new, endoscopic suturing method for septal mucosal flaps following septal surgery.
Method
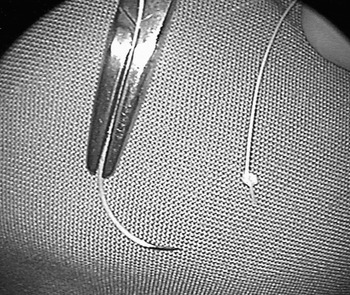
We use a 0° Hopkins rod endoscope for septoplasty and for the suturing of the septum. A 3.0 Vicryl rapide (undyed) suture (Ethicon, San Angelo, Texas, USA) on a small, curved cutting needle (PS-2) is used for suturing. A knot is placed in the distal end of the suture material. A small needle holder is used and the needle is held along the shaft of the needle holder (Figure 1) so that the force of pushing the needle through the tissue is applied directly behind the needle.
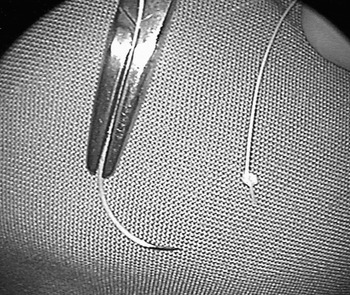
Fig. 1 The needle is held in the needle holder so that the shaft of the needle and the natural curve is in the same plane as the handle of the needle holder.
The initial placement of the suture is at the posterior part of the septum and is performed under endoscopic guidance. The first suture may pass just anterior to the middle turbinates or, if the middle turbinates are unstable, may be passed through the middle turbinate, septum and middle turbinate on the opposite side. If this is done, counter pressure from the scope needs to be placed on the middle turbinate on the second side, in order to allow the needle to be passed through the bone of the middle turbinate. The needle is passed back through the septum, just anterior to the middle turbinate, to the opposite side. A space of a few centimetres is then left before passing the needle through the septum, creating the quilting effect (Figure 2). Using continuous suturing technique, flaps are approximated as the needle is advanced towards the caudal end of the septum. As the septal incision is approached, the needle is passed through the septum behind the incision from the opposite nasal cavity and then anterior to the incision so that the suture closes the septal incision (Figure 3). The final pass of the suture is placed just anterior to the incision site through the skin of the vestibule. To tie the suture on itself, toothed forceps are used to hold a fold of skin while the needle passes through. The suture is knotted on itself (Figure 4). The vestibular skin is preferred to nasal mucosa for the anterior knot, as the skin has greater tensile strength and the suture is less likely to cut through.

Fig. 2 The sutures are placed so that when the suture is tightened it plicates the septal flaps together, removing the dead space.

Fig. 3 As the suture is brought forward, the stitch is placed so that the incision is closed by the suture.

Fig. 4 The septal suture is tied on itself through the skin of the nasal vestibule. The toughness of the skin prevents the suture from tearing through the tissue. Note the suture closing the Killian's incision on the septum.
Discussion
The most difficult part of suturing the septal mucosa is placing a knot in the posterior part of the septum. Placing the knot prior to passing the needle through the septum and continuous suturing technique overcomes these difficulties. Furthermore, endoscopic septal suturing technique is more precise and reduces the risk of needle trauma to the turbinates. Lee and VukovicReference Lee and Vukovic2 described the technique of continuous suturing using 4.0 chromic catgut as a haemostatic suture. The slightly curved needle is straightened until a very slight curve remains at the tip. Their technique of suturing involves starting the sutures in an anterior to posterior direction, and then continuing in a semicircular fashion along the dorsal part of the septum to join the anterior end, where a knot is tied. The method described by SessionsReference Sessions1 is similar in that a continuous suturing technique is used. This author used a 4.0 plain catgut suture on a small, straight needle and started the suture in a posterior to anterior direction. The difference in our technique, compared with Sessions' method, is that we use a curved needle, which reduces trauma to the mucosa of the turbinates. Also, placing the final knot in the vestibular skin reduces the risk of sutures cutting through the mucosa and also reduces granulation formation. The other advantage of this technique is the opportunity that it affords to incorporate the middle turbinates into the continuous suture, thereby medialising them during the healing process and in so doing preventing adhesions from forming due to lateralisation of an unstable middle turbinate.