Introduction
Endoscopic ear surgery has gained immense popularity among otologists over the past few decades. The domain of transcanal endoscopic ear surgery has been expanding ever since, with surgeries addressing diseases involving external ear to as far as the lateral skull base.Reference Tarabichi1–Reference Kojima, Tanaka, Yaguchi, Miyazaki, Murakami and Moriyama3 The main reasons behind this are the technical advantages that endoscopes offer in comparison to conventional microscopes, such as a wider field of vision, higher magnification to see finer structural details and the ability to look around corners without disrupting normal tissues for the sake of access.Reference Bennett, Zhang, Labadie and Noble4
Although endoscopes have established a firm ground in otological surgery, there are legitimate concerns regarding their safety. A number of studies performed in cadaveric and experimental models have shown a significant increase in temperature within the confined space of the middle ear.Reference Kozin, Lehmann, Carter, Hight, Cohen and Nakajima5–Reference Bottrill, Perrault and Poe6 The heat generated could potentially disrupt the homeostasis of inner ear structures and fluids. This could lead to adverse post-exposure outcomes. Such an estimation is only possible in vivo. We have attempted to make an objective estimation of intra-operative middle ear temperature change for different light sources used in endoscopic ear surgery and note the post-operative outcomes in terms of clinical and audiological parameters.
Materials and methods
Patient selection and randomisation
A total of 64 patients diagnosed with chronic otitis media with central perforation (mucosal disease) with pure conductive type hearing loss underwent endoscopic type 1 tympanoplasty. Patients who were aged between 18–60 years, without any active infection or known systemic disease, such as diabetes mellitus, thyroid or neurological disease, and who were not on chronic medication were included in this study.
The patients were randomised into two groups based on the light source of the endoscopic unit, either xenon or light-emitting diode (LED). The randomisation sequence was generated by a table of random numbers, and allocation was concealed using sealed opaque envelopes. Both the patients and the surgeons were blinded from the light source used. A study investigator, who was excluded from further data collection and analysis, oversaw the randomisation process, preparation and set-up of the respective surgical procedures. All patients underwent routine pre-operative investigations including pure tone audiometry, impedance audiometry and high-resolution tomography scans of temporal bone. Written informed consent and institutional ethics committee approval were obtained. All operations were performed by authors A Das and S Mitra.
Temperature measurement
The ambient room temperature was recorded before the start of surgery. For the blinding process, the endoscopy unit was kept covered by an opaque sheet before the beginning of the surgery. The intensity of both light sources was kept at 50 per cent. A Stryker® 1288 HD camera system with either an X8000 xenon light source or L9000 LED light source was used. Karl Storz (Tuttlingen, Germany) rigid endoscopes (4 mm diameter, 18 cm length; 0 degree) were used for all cases. Endoscopic trans-canal type 1 tympanoplasty was done in both groups. A separate incision in the postero-superior aspect behind the pinna, well hidden behind the hairline, was made for harvesting the graft. The margins of perforation were freshened. The canal incision was made 5 mm behind the annulus extending upwards anterior to the lateral process of the malleus and inferiorly up to the five o'clock position in the right ear and seven o'clock position in the left ear. The tympanomeatal flap was elevated. Ossicular mobility and round window reflex were checked. Temperature measurement was performed using a K type thermocouple at standard operating room temperature (24.5°C/76.1°F), and the thermocouple was calibrated before each operation. The thermocouple was inserted into the thermocouple jack, and the switch was shifted towards the Fahrenheit scale. The ball point probe of the thermocouple was then placed in contact with the promontory and round window niche (Figure 1). Three readings were taken at each interval of 0, 20, 40 and 60 minutes, depending on the duration of each surgery. The mean of each of these three readings as well as the mean for all readings at the two anatomical points (promontory and round window niche) were taken. Graft was placed using the underlay technique, and gelfoam was placed in the middle ear and external auditory canal.

Fig. 1. Thermocouple probe being used intra-operatively to measure temperature at: (a) the promontory and (b) the round window niche. Et = Eustachian tube; Mh = malleus handle; Tcp = thermocouple probe; Pr = promontory; Isj = incudo-stapedial joint; Rwn = round window niche
Study parameters and result analysis
The parameters studied were mean temperature change with respect to the time interval of surgery, mean audiometric change (air conduction threshold in decibels) with respect to each frequency (0.5, 1, 2, 4, 6 and 8 kHz), incidence of post-operative complications such as vomiting in the first 24 hours, vertigo and tinnitus at the end of first the week.
For statistical analysis, data were analysed by SPSS® statistical software (version 24) and GraphPad Prism statistical software (version 7). Change in temperature (°F) was compared with the time interval of the surgical procedure (in minutes) using the one-way analysis of variance (ANOVA) test followed by Dunn's multiple comparison test. Tests of normality were performed using Kolmogorov–Smirnov test. Normally distributed data were compared using the ANOVA test followed by Dunn's multiple comparison test. Fisher's exact test was used to determine the level of significance. A p-value less than 0.05 was considered to be statistically significant.
Results
The mean age of the patients in the xenon and LED light source groups was 32.85 ± 11.27 years and 32.68 ± 8.91 years, respectively. There was no statistically significant difference between the two groups (p = 0.9502).
In the xenon light source group, 64 per cent of patients were males and the rest were females. In the LED group, 60 per cent were males and the rest were females. There was no statistically significant difference between the two groups in this respect.
The mean body temperature of patients in the xenon group was 98.6°F (37°C) and the mean body temperature of patients in the LED group was 98.8°F (37.1°C). The results did not show any statistical significance (p = 0.825).
The mean temperature change (measurements taken at the promontory and round window niche as described previously) at Δ20–40 minutes when compared to that of Δ0–20 minutes with xenon as the light source, showed a statistically significant difference (p < 0.0001). Similar results were found when the temperature change was compared between Δ0–20 and Δ0–40 minutes for the xenon light source. When the same parameters were analysed for the LED light source, no statistically significant difference was found. A statistically significant difference was found between the two light sources when mean temperature change at a particular time interval was taken into account, at Δ0–40 and Δ20–40 (Figure 2).

Fig. 2. Mean temperature change (°F) with respect to time interval (minutes) of surgery. **** represents p value of <0.0001 obtained for Xenon light source when the temperature change at that point is compared with Δ0-20 for the same source ‡‡‡‡ represents p value of <0.0001 when temperature change is compared between two light sources at a particular time interval of surgery. LED = light-emitting diode
Mean audiometric change (pre-operative versus post-operative (in decibels)) was seen in relation to respective frequencies. It was found that when xenon was used as the light source, mean audiometric change started to show a downhill curve from 4 kHz with a statistically significant difference at 4, 6 and 8 kHz (p < 0.01 for 4 kHz and p < 0.001 for 6 and 8 kHz). Clinically, this was interpreted as a poor outcome because patients without pre-existing high frequency hearing loss (in the observed frequencies) showed post-operative change at the same frequencies, causing an increased audiometric change (with the use of that particular light source). With an LED as the light source, a statistically significant difference was found at 8 kHz only. When mean audiometric change was compared between xenon and LED light sources for a particular frequency, a statistically significant difference was found between the two at 4, 6 and 8 kHz (p < 0.0001 for all three frequencies; Figure 3).

Fig. 3. Mean audiometric change (pre-operative versus post-operative (in decibels)) was seen in relation to respective frequencies. **, *** and **** represent p-values <0.01, <0.001 and <0.0001, respectively, when that frequency was compared to 0.5 kHz. ‡‡‡‡ represent p value <0.0001 when audiometric change was seen at a particular frequency between the two sources.
A total of 56.2 per cent (18 of 32) of the patients belonging to the xenon group experienced post-operative vomiting, whereas in the LED group 28 per cent (9 of 32) experienced vomiting. This was found to be statistically significant (p = 0.042). Vertigo was reported by 40.6 per cent (13 of 32) of patients in the xenon group and 18.7 per cent (6 of 32) of patients in the LED group. Post-operative tinnitus was reported by 34.3 per cent (11 of 32) of patients in the xenon group and 15.6 per cent (5 of 32) of patients in the LED group. No statistical significance was found between the two groups in terms of vertigo and tinnitus (p = 0.099 and p = 0.147, respectively).
Discussion
Several studies have shown that there is a considerable increase in temperature within the limited space of the middle ear when performing endoscopicear surgery. However, these studies have been mostly performed on cadavers or in experimental models. In vivo assessment of middle-ear temperature change using different light sources and its impact on inner ear function has been attempted in our study, probably for the first time, to the best of the authors’ knowledge.
During any endoscopic ear surgery, the most prominent structure that is exposed to the light is the promontory, which is the lateral wall of the cochlea that harbours the delicate inner ear structures such as hair cells and inner ear fluids (Figure 4). Therefore, the thermocouple probe was placed over the most accessible area without damaging any important middle or inner ear structure. We agree that the temperature change would probably be more evident if measured over the round window membrane. However, as this was a blind procedure, there was a possibility of microtrauma to the round window membrane itself. Therefore, we chose the bony anatomical structure closest to the round window membrane, the round window niche, as our second anatomical landmark for recording the temperature. Ito et al. measured the middle-ear temperature in a simulated three-dimensional experimental model at three points: the promontory, facial nerve and lateral semi-circular canal. However, in a live surgery, such as endoscopic tympanoplasty, this may not always be possible as there remains a chance of ossicular injury.Reference Ito, Kubota, Takagi, Watanabe, Futai and Furukawa7
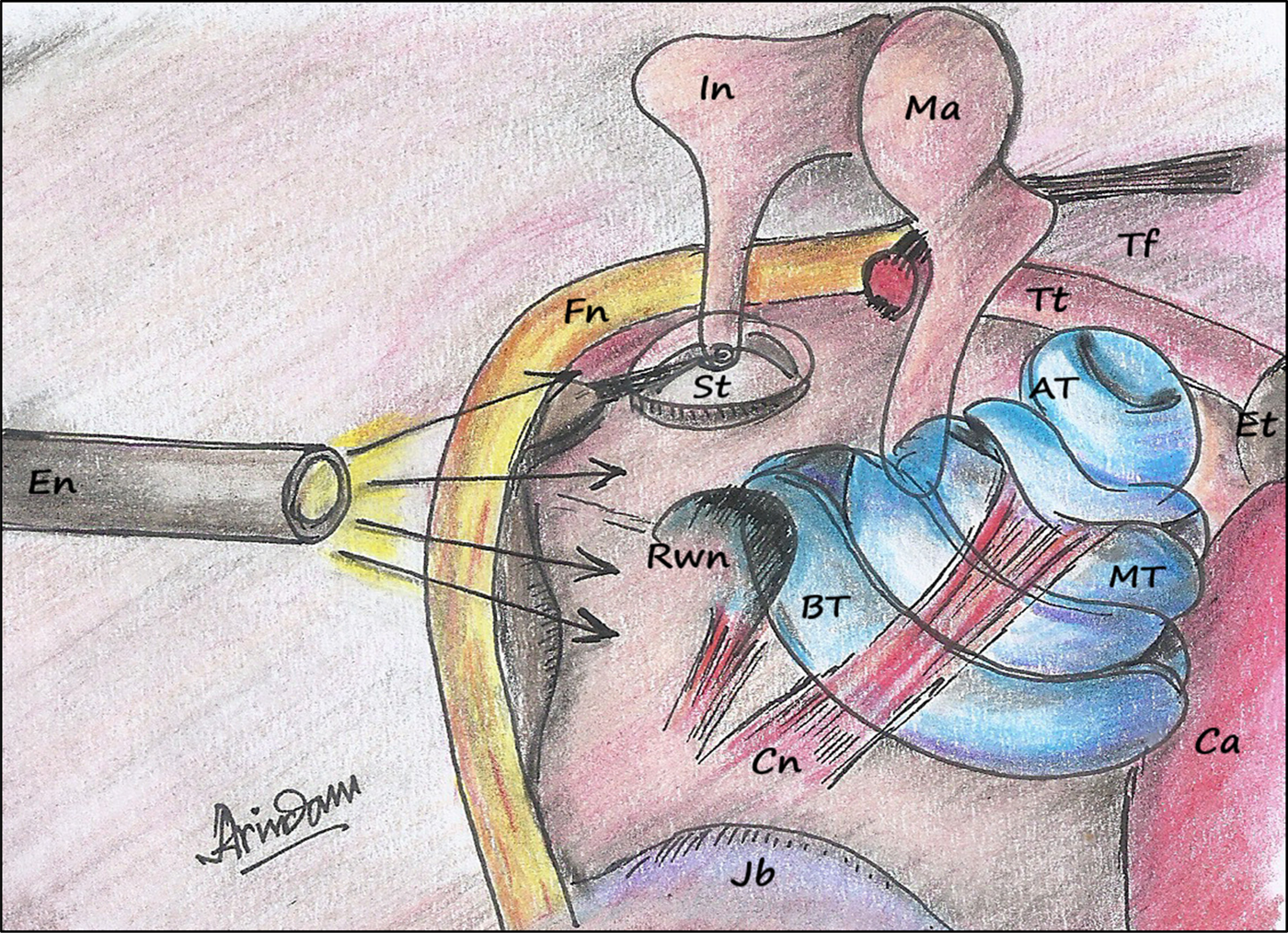
Fig. 4. Middle-ear and inner ear structures exposed to heat from a light source during endoscopic ear surgery. Note the relative proximity of the basal turn of cochlea to the light source. En = endoscope; In = incus; Ma = malleus; Fn = facial nerve; Tt = tensor tympani; Tf = tensor fold; St = stapes; AT = apical turn; Et = Eustachian tube; Rwn = round window niche; MT = middle turn; BT = basal turn; Cn = cochlear nerve Ca = carotid artery; Jb = jugular bulb
The cochlea, the sense organ of hearing, houses the auditory receptors. The outer hair cells are delicate structures that are susceptible to external stimuli such as temperature changes.Reference Lonsbury-Martin, Martin, Flint, Haughey, Lund, Niparko, Robbins, Thomas and Lesperance8 Aksoy et al. demonstrated a significant decrease in the distortion product otoacoustic emissions values and a significant increase in the auditory brainstem response thresholds in guinea pigs subjected to xenon light for 5 minutes.Reference Aksoy, Dogan, Ozturan, Eren, Veyseller and Gedik9 Changes in the latency, duration and amplitude of cochlear microphonics with a rise in temperature from 18°C to 39°C have been reported near the round window, in hamster cochlea with sound stimuli.Reference Kahana, Rosenblith and Galambos10 Bottrill et al. concluded that a temperature rise in middle-ear endoscopy can cause a rise in temperature in the lateral semi-circular canal, similar to a warm caloric stimulation, which is responsible for vestibular symptoms such as vertigo and vomiting.Reference Bottrill, Perrault and Poe6
Various light sources, such as halogen, xenon and LED lights, have been used in endoscopic ear surgery. Aksoy et al. compared halogen and xenon light sources in middle-ear endoscopy at 100 per cent intensity. They found a decline in auditory function with prolonged use of a xenon light source.Reference Aksoy, Dogan, Ozturan, Eren, Veyseller and Gedik9 Dundar et al. compared a xenon light source with LED at 100 per cent intensity. They found that the lowest temperatures were observed with the LED light source, which is in accordance with our results.Reference Dundar, Bulut, Yükkaldiran, Güler, Demirtaş and Iynen11 Tomazic et al. found that with the increase in intensity from 33 to 66 per cent up to 100 per cent, there was a concomitant rise in the maximum tip temperature, irrespective of the type of light source used.Reference Tomazic, Hammer, Gerstenberger, Koele and Stammberger12 A decrease in light intensity, which is protective for the inner ear, is not associated with a deterioration in the image quality.Reference McCallum, McColl and Iyer13,Reference Ozturan, Dogan, Eren and Aksoy14 An optimal balance between the intensity of the light used as well as the image quality can be achieved in most cases when the intensity is kept at 50 per cent.Reference Ryan, Wuesthoff and Patel15 Therefore, we used 50 per cent intensity in our study.
We performed the study under actual clinical settings in vivo and measured the tissue temperature directly. This is a better representative of the temperature change because the probe is kept directly over the middle-ear tissues rather than the endoscope tip. Moreover, temperature change may be overestimated in simulated anatomical or cadaveric models as the ‘heat sink’ contributed by blood and inner ear fluid circulation cannot be taken into account in such cases.Reference Bottrill, Perrault and Poe6,Reference Mitchell and Coulson16
We do acknowledge certain limitations of our study, such as a limited sample size and comparison between only two types of light source for one particular type of endoscopic ear surgery.
• Thermal damage to delicate inner ear structures in endoscopic ear surgery has long been contemplated
• Xenon and light-emitting diodes (LEDs) are two commonly used light sources for endoscopic ear surgery
• No objective documentation of the effects of various light sources used in endoscopic ear surgery has been done in vivo
• There was a statistically significant rise in the middle-ear temperature with time
• Poorer audiometric outcomes were noted in the higher frequency range (4–8 kHz) when xenon was used as a light source compared to LED despite operating surgeons and the assistant being constant in all cases
• Xenon light sources should be replaced with cooler light sources such as LEDs for all endoscopic ear surgical procedures
Conclusion
For endoscopic ear surgery, an LED light source is associated with less middle-ear temperature rise and audiometric changes at higher frequencies when compared to a xenon light source. Therefore, the use of a xenon light source must be thoroughly questioned in the realm of endoscopic ear surgery and should be replaced with cooler sources such as an LED light source.
Competing interests
None declared






