Introduction
In the head and neck, inverted papillomas most commonly originate from the mucosa of the lateral nasal wall. They can extend into the paranasal sinuses, orbits and anterior skull base. They have also been reported to occur in the pharynx, nasopharynx, lacrimal sac and, rarely, the temporal bone.Reference Wenig1
Primary temporal inverted papilloma with premalignant change is an extremely rare entity which has not previously been reported (as researched by an Ovid Medline search using the medical subject headings ‘inverted papilloma/Schneiderian papilloma’ and ‘middle ear/temporal bone’).
In this paper, we present a rare case of this tumour requiring resection via a Fisch type A infratemporal fossa approach. We also review the available data on temporal inverted papilloma, and we discuss its pathogenesis, diagnosis, management and prognosis.
Case report
A 52-year-old man presented with intermittent left-sided otorrhoea for 30 years and facial distortion for three years. One year prior to presentation, he had experienced ipsilateral headache and had developed a complete ipsilateral sensorineural hearing loss. He also complained of diplopia over the three months preceding presentation. He denied nasal obstruction, epistaxis and vertigo. His medical history was otherwise unremarkable.
Physical examination revealed a flesh-coloured, extremely friable mass protruding from the left middle ear and obstructing the deep external acoustic meatus. Right ear examination was normal.
Nasoendoscopy did not show any lesions in the nasal cavity or nasopharynx.
Biopsy of the mass revealed high grade squamous intraepithelial neoplasia.
Computed tomography (CT) revealed a large area of soft tissue opacification of the left middle ear, mastoid cavities and temporal bone, with severe sphenoid bone erosion (Figure 1). Magnetic resonance imaging (MRI) showed that the tumour was adjacent to the middle fossa dura and associated with focal oedema of the temporal lobe (Figure 2).
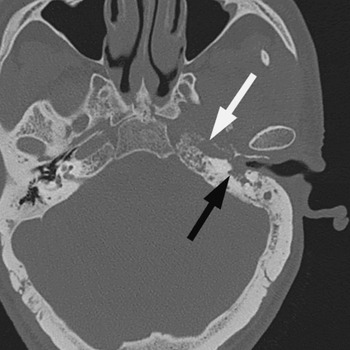
Fig. 1 Axial computed tomography scan showing a mass of soft tissue density in the left external auditory canal, middle ear and mastoid (black arrow), with extension into the inner ear and petrous apex. Destruction of the left bony eustachian tube and the petrous portion of the carotid artery canal is also evident (white arrow).

Fig. 2 Coronal, T1-weighted, fat-suppressed, postgadolinium contrast magnetic resonance image showing a moderately enhancing tumour adjacent to the middle fossa dura, associated with focal oedema of the left temporal lobe (arrow).
The patient underwent a Fisch type A infratemporal fossa approach to the petrous apex and infratemporal fossa. Initially, a canal wall down mastoidectomy was performed and the facial nerve was skeletonised from the stylomastoid foramen to the geniculate ganglion.
Intra-operatively, the tumour was seen to fill the middle ear and mastoid, with extension into the petrous apex, inner ear and left skull base. The horizontal segment of the facial nerve had been destroyed by tumour invasion. Several small, focal epidural abscesses and large areas of dural adhesion were also encountered. The tumour extended into the infratemporal fossa. There was complete destruction of the bony eustachian tube and circumferential encasement of the intratemporal carotid artery by the tumour.
A subtotal temporal bone resection was performed, and the tumour was dissected from the middle cranial base with preservation of the dura. The dissection was carried forward to the infratemporal fossa, deep into the petrous apex, and medially to the left nasopharynx. The tumour which encompassed the carotid artery was dissected free. The lateral skull base defect was repaired with a temporalis muscle flap.
Permanent histological examination confirmed the diagnosis of inverted papilloma with carcinoma in situ (Figures 3 and 4).

Fig. 3 Photomicrograph of middle-ear papilloma with inverted morphological features, demonstrating significant focal nuclear pleomorphism indicative of carcinoma in situ. (H&E; original magnification ×20)

Fig. 4 Photomicrograph of the same lesion as in Figure 3, shown to be composed of severely pleomorphic cells. (H&E; original magnification ×60)
Post-operatively, the patient received radiation therapy (6000 cGy) to the left temporal bone.
At the time of writing, he had been followed for eight months without evidence of recurrent disease.
Discussion
Inverted papilloma involving the temporal bone is extremely rare. We reviewed published reports of inverted papilloma involving the middle ear or temporal bone and found only 20 evaluable cases (19 plus the present case). Of these, 10 patients' neoplasms were localised exclusively in the temporal bone, while the others were located jointly in the temporal bone and nasal cavities.
Review of the literature showed that, in 90 per cent (nine of 10) of cases in which inverted papillomas involved the temporal bone and nasal cavities, the nasal tumour preceded the middle-ear tumour. The middle-ear and nasal tumours were also ipsilateral, with the exception of one case with bilateral middle-ear involvement. It may thus be inferred that inverted papilloma involving the temporal bone and nasal cavities is a unique type of sinonasal inverted papilloma. In such cases, we suspect that the tumour arises in the nasal cavity and secondarily involves the temporal bone. It is likely that this involvement is through direct transmission of prior sinonasal disease through the eustachian tube, due to the aggressive nature of the tumour. In some reported cases, CT and nasoendoscopy were unable to detect any continuity of lesion or any irregularities of the eustachian tube; therefore, we speculate that some other route of spread may play a role in the aetiology of sinonasal inverted papilloma involving the temporal bone, and we suggest the need for further research. Ferlito et al. have suggested that clinicians should distinguish primary sinonasal papilloma with secondary temporal bone involvement from true primary temporal papilloma.Reference Ferlito, Devaney and Rinaldo2 Therefore, we consider that a diagnosis of primary temporal inverted papilloma should be made only following clinical exclusion of sinonasal papilloma.
To date, only 10 cases of primary temporal inverted papilloma have been described (including the present case).Reference Wenig1, Reference Roberts, Dinges and Hanly3–Reference Marioni, Altavilla, Busatto, Blandamura, de Filippis and Staffieri7 Primary temporal inverted papilloma has been reported in six women and four men, with a mean age of 40.1 years (median age, 41.5 years; range, 19–77 years). These tumours were localised in the middle ear in seven patients (70 per cent), in the middle ear and mastoid in two patients (20 per cent), and in the temporal bone with infratemporal fossa invasion in one patient (10 per cent). None of these cases had a history of sinonasal inverting papilloma.
The aetiology of primary temporal inverted papilloma is poorly understood. One hypothesis suggests that during embryological development there may be ectopic migration of the ectodermally derived Schneiderian membrane to the endodermally derived mucosa of the upper aerodigestive tract, including the tubotympanic recess, which becomes the tympanic cavity and the eustachian tube.Reference Wenig1 This theory may explain the appearance of inverted papilloma in the temporal bone; however, the stimulus for development of temporal inverted papilloma is not well understood. Possible aetiological factors include viruses, chronic inflammation, allergy and carcinogen exposure (including occupational exposure).
Primary temporal inverted papilloma normally manifests with hearing loss, otorrhoea and/or otalgia. All the cases reported to date have involved decreased hearing in the affected ear. In 60 per cent of reported cases (six of 10), there has been a definite history of chronic otitis media which did not resolve following antibiotic treatment. Analysis of the lesion with biopsy is the key to accurate diagnosis of inverted papilloma. Temporal bone CT (and/or MRI) is essential in order to determine the degree of temporal bone extension of the lesion and the most appropriate surgical treatment.
The treatment of primary temporal inverted papilloma is mainly surgical. Nevertheless, any surgical treatment must guarantee a radical resection of the lesion in all cases, because of the possible association of this tumour with malignancy and the intrinsic local aggressiveness of the neoplasm itself. Radical tympanomastoidectomy or temporal bone resection should be considered as the initial treatment, because of the high recurrence rate if the tumour is not completely excised. The lesion may recur despite appropriate treatment, necessitating further surgical intervention. Because of the risk of malignant transformation of the papillomatous epithelium following radiotherapy, such treatment is recommended only in cases which are inoperable or associated with malignancy.
The recurrence rate for sinonasal inverted papilloma has been reported as 40–78 per cent with limited surgery and 0–14 per cent with more aggressive surgery.Reference Vrabec8 Despite the scarcity of reported cases, the recurrence rate seems to be higher for temporal inverted papilloma. After initial surgery, primary temporal inverted papilloma recurred in five of 10 patients (50 per cent) described in the literature.Reference Wenig1, Reference Roberts, Dinges and Hanly3–Reference Marioni, Altavilla, Busatto, Blandamura, de Filippis and Staffieri7 Recurrence was noted in three of six cases (50 per cent) treated with tympanomastoidectomy and in both cases (100 per cent) treated with myringotomy with simple excision. Although multicentricity of inverted papilloma has been suggested to explain the high rate of recurrence, inadequate tumour removal during the initial surgery seems to be the most important predictor of local recurrence. Compared with sinonasal inverted papilloma, we postulate that the more complex anatomical characteristics of the temporal bone, which may impede the complete elimination of disease, may explain the higher recurrence rate of primary temporal inverted papilloma.
• Primary temporal inverted papilloma is extremely rare; it should be diagnosed only after clinical exclusion of sinonasal papilloma
• A case of primary temporal inverted papilloma associated with premalignant change is reported
• Treatment comprises radical resection of the lesion
• The recurrence rate is higher for primary temporal inverted papilloma than for sinonasal inverted papilloma, and long-term post-operative follow up is mandatory
Limited information is available on the prognosis of primary temporal inverted papilloma, because of the small number of cases and (generally) short follow-up times reported. Of the reported cases, over follow-up periods ranging from three months to 20 years, two patients suffered a single recurrence while three suffered two or more recurrences.Reference Wenig1, Reference Roberts, Dinges and Hanly3–Reference Marioni, Altavilla, Busatto, Blandamura, de Filippis and Staffieri7 No carcinoma developed, and no patients died from their tumour.
To the best of our knowledge, the current case represents the first report of primary temporal inverted papilloma accompanied by premalignant change. Long-term post-operative follow up is mandatory for patients with this tumour, in order to detect recurrence and to monitor for malignant transformation. Magnetic resonance imaging may be useful in the detection of recurrences during post-operative follow up; it is considered very accurate in distinguishing papilloma from adjacent inflammatory tissue and scar tissue, but is unable to differentiate inverted papilloma from associated squamous cell carcinoma.Reference Savy, Lloyd, Lund and Howard9
Acknowledgement
This work was supported by a grant from Jiangsu (China) Health Administration to G Xing (grant number RC2007064).






