Introduction
Granular myringitis is a chronic and difficult-to-treat condition of the tympanic membrane and often deep part of the ear canal. It is characterised by ulceration and de-epithelialisation of the stratified squamous layer of the drum, with variable amounts of granulation of the tympanic membrane. It presents with otorrhoea and subsequent recurrent infection, itching, otalgia, hearing loss, and aural fullness. Predisposing events causing granular myringitis include infection (mainly otitis externa), or local trauma including otological interventions and surgery.Reference Chung, Lee and Kim1,Reference Devaraja2 A previous study found that 80 per cent of patients had a prior history of myringotomy with or without ventilatory tube insertion, and revealed the condition is rare in children.Reference Levi, Ames, Gitman, Morlet and O'Reilly3 Bullous myringitis is an acute tympanic membrane inflammatory disease with vesicles, not discussed in this article.
There is no consensus regarding descriptions of granular myringitis and there have been several classification attempts. In 2000, El-Seifi and Fouad described focal, segmental and diffuse categories.Reference El-Seifi and Fouad4 In 2006, Wolf et al. classified granular myringitis into four grades: grade 1 is ulceration without polypoidal tissue, grade 2 is focal polypoidal tissue, grade 3 is diffuse polypoidal tissue and grade 4 is diffuse polypoidal tissue involving the external auditory canal.Reference Wolf, Primov-Fever, Barshack, Polack-Charcon and Kronenberg5 Grades 3 and 4 can be very difficult to treat, and have a high chance of progressing to fundal stenosis. In 2011, Kim described granular myringitis as being marginal or non-marginal, and subsequently divided it into ulcerative or non-ulcerative.Reference Kim6 Bansal, in 2017, proposed a classification system based on whether the condition is primary or secondary.Reference Bansal7 The variation in classification and grading systems highlights the wide variety of clinical appearances of granular myringitis. Long-standing granular myringitis can lead to stenosis or atresia of the external auditory canal.Reference Wolf, Primov-Fever, Barshack, Polack-Charcon and Kronenberg5,Reference Blevins and Karmody8
First-line treatment targets the inflammatory process, and involves aural toileting and topical medications such as steroids and antimicrobials. In a proportion of cases, this treatment will be successful and may lead to resolution. However, recurrence is common. Second-line treatment is variable and targets removing the granulation tissue itself. Published techniques include the use of chemical cautery with silver nitrate, carbon dioxide (CO2) laser causing vapourisation, or surgery to excise the abnormal tissue. Surgical options include curettage and tympanoplasty. Unconventional methods of treatment include diluted vinegar, Castellani solution (4.5g phenol, 10g resorcinol, 0.3g basic fuchsin, 5ml acetone, 9.4ml of 80 per cent ethanol and 85.6ml of distilled water) and 5-fluorouracil.Reference Kim6,Reference Jung, Cho, Yoo, Lim and Chae9,Reference Atef, Hamouda, Mohamed and Fattah10 Treatment must be administered with caution to prevent both tympanic membrane perforation and extension of the inflammatory process. There is no current consensus on treatment either.
We present a minimally invasive technique using the potassium titanyl phosphate (KTP) laser. The KTP laser emits green light (532 nm) that is avidly absorbed by red targets, especially melanin and oxyhaemoglobin. Conversely, it is not well absorbed by water and white lesions. The KTP laser can be delivered by a hand-held wand, which allows it to be used like other otological instruments. This technique has not been described in the literature before.
Materials and methods
This manuscript has been written with reference to the ‘CARE’ (case report) reporting guidelines.
Procedural technique
We use the Litechnica Lightlas™ 532 nm laser with its fibre-optic wand (Figure 1). All procedures are performed in an operating theatre with an operating microscope, under a general or local anaesthetic according to surgeon and patient preference. The ear is prepared with surgical cleaning using aqueous povidone-iodine disinfectant solution, which is then suctioned out. Topical adrenaline is applied to the drum. The laser is set to a power setting of 500–600 mW and is used in continuous mode. Under high magnification, the granulation tissue or ulcer is blanched with the KTP laser to create a thin layer of char, ideally over the middle fibrous layer of the drum (Figure 2). The wand should not touch the target area. We have then variably used either bismuth iodoform paraffin paste soaked ribbon gauze, Otocomb Otic© corticosteroid cream or a steroid ointment, depending on the associated inflammation or infection.
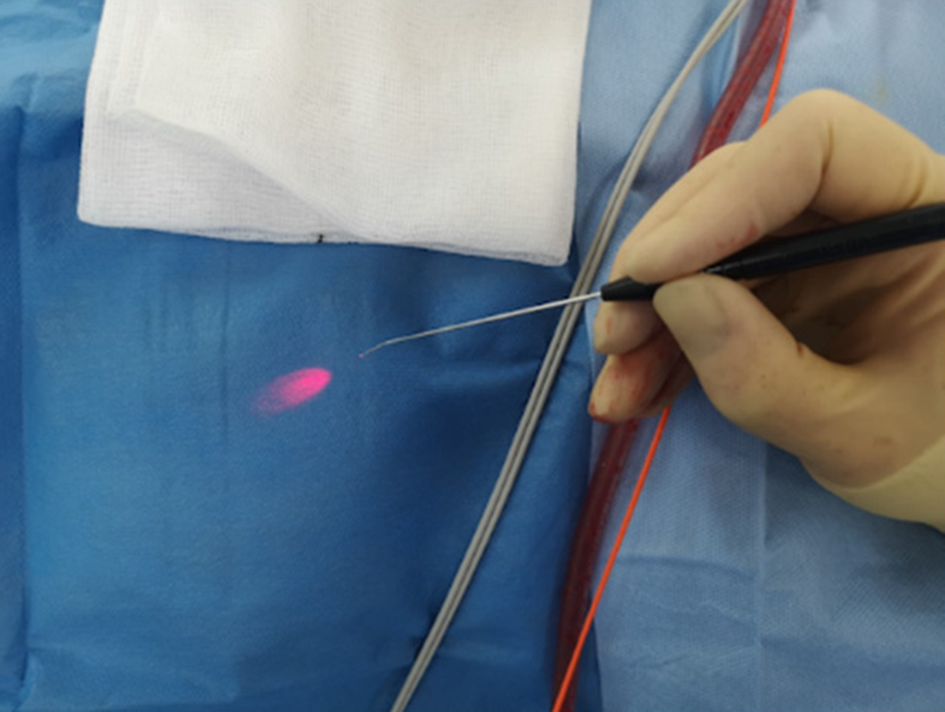
Fig. 1. Hand-held potassium titanyl phosphate wand with aiming beam.
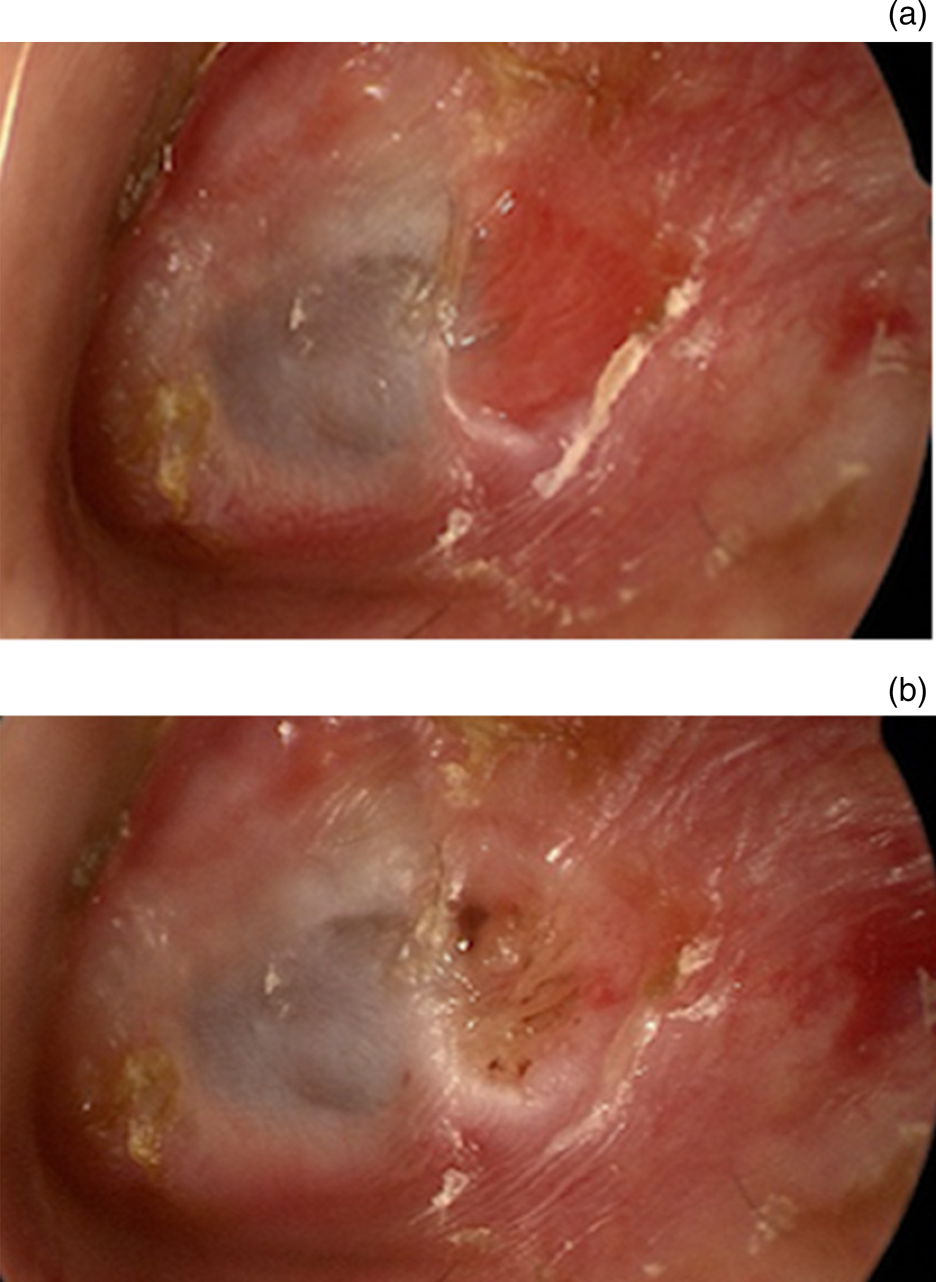
Fig. 2. (a) Endoscopic appearance of a posterior superior marginal area of myringitis of the left ear. (b) Appearance of myringitic area with a layer of char after the potassium titanyl phosphate laser has been used.
All patients were routinely followed up at two months post-operatively for examination of the tympanic membrane and audiological assessment with pure tone audiometry. In addition, those patients with surgical packing were seen at three weeks post-operatively for pack removal.
Main outcome measures
The primary aim was to assess whether the KTP laser technique can provide successful treatment for myringitis. Secondary measures included: identifying features and risk factors for chronic granular myringitis, reviewing the procedure's safety by assessing complications, and examining the impact on hearing.
Study setting and design
We performed a retrospective case review of patients who had undergone KTP laser treatment for myringitis. Patients were identified by reviewing our departmental scheduling database for relevant cases between the years 2015 and 2020, and the information obtained was cross-referenced with the operating theatre scheduling database to ensure complete data capture. We included patients of all ages with a diagnosis of myringitis who had undergone KTP laser surface tympanoplasty. We excluded patients who had any simultaneous pathology requiring additional surgery such as a tympanoplasty for a tympanic membrane perforation (n = 1). Case notes were obtained to enable review of the clinical documentation, including operation notes and audiograms.
We identified the time from the diagnosis of myringitis to the KTP laser treatment. We reviewed the operation notes for information on the appearance of the drum and the technical details of the procedure. Intra-operative pictures were reviewed by two independent clinicians. Involvement of the drum was classified into four categories according to whether 1–25 per cent, 26–50 per cent, 51–75 per cent or 76–100 per cent of the drum was involved. The position of the myringitis was categorised into four quadrants (posterior superior, posterior inferior, anterior superior, anterior inferior) or considered central. We also examined whether the granular myringitis was marginal or not.
Post-operatively, we categorised the appearance of the ear drum as worse, the same, improved or resolved. Pure tone averages were calculated (from frequencies 0.5, 1, 2 and 4 kHz) for the affected ear pre- and post-intervention. Time to discharge from the clinic was also noted. All patients underwent a final telephone follow up in 2020 to ascertain whether they had any chronic ear symptoms (specifically pain, recurrent discharge, hearing loss, aural fullness, vertigo or tinnitus), and all were offered face-to-face follow up to examine the tympanic membrane.
Categorical analysis
Myringitis involvement, otological history and post-procedure treatment were assessed with categorical analysis using chi-square tests.
Ethical considerations
This retrospective case review was registered with the local clinical effectiveness unit and subsequently approved (approval code: 10838). The Health Research Authority decision tool determined no ethical approval was required.11
Funding
This review received no specific grant from any funding agency, commercial or not-for-profit sectors
Results
Patient demographics
We identified 14 patients who underwent treatment with the KTP laser for their myringitis. Two patients had required two treatments with the KTP laser. One of these (patient four) had a KTP laser tympanoplasty in July 2016 and re-presented needing further lasering on the same side in November 2019. We felt that this represented two episodes of myringitis for the following reasons: the ear was seen to be dry before his first discharge, the position of the myringitis was different, and there was a significant period of time between the two cases. This was therefore defined as a recurrent case. A second patient (patient eight) had 80 per cent of the drum involved. They had an initial procedure in April 2017 and required a second procedure in July 2018. We felt this was a single extensive myringitis episode that proved more difficult to treat, and the patient was not seen with a dry ear before proceeding with the second procedure. This case was therefore defined as residual disease. One patient had treatment on both ears. In total, we had 17 cases of laser treatment for 16 discrete episodes of myringitis in 15 ears and 14 patients (Table 1).
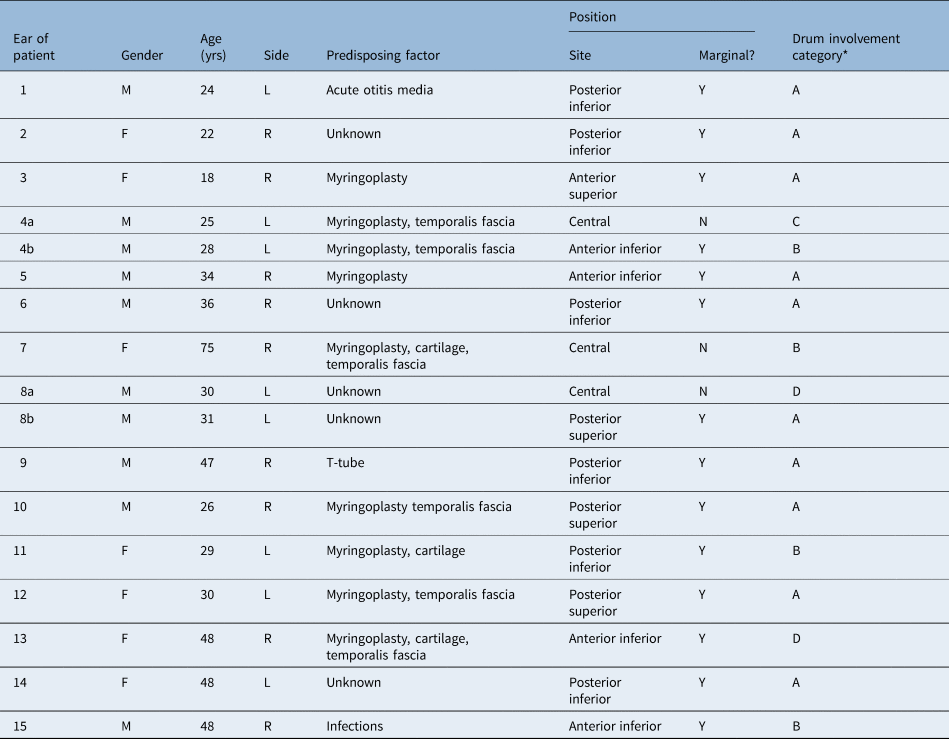
Table 1. Patient demographics, and site and size of myringitis
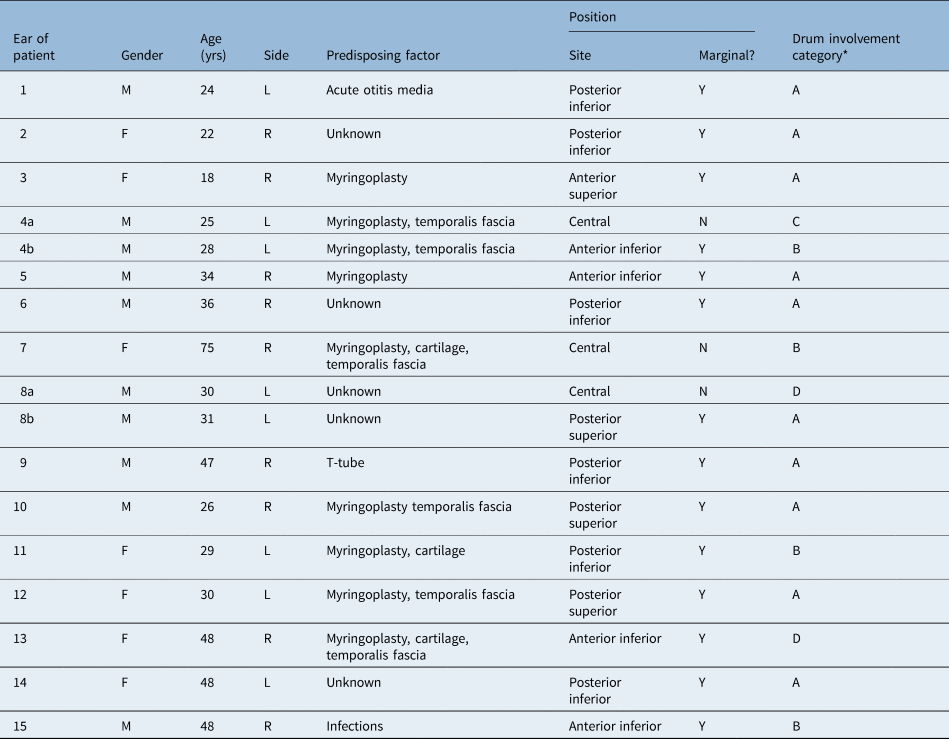
The ears of patient four (4a and 4b) represent the recurrent case. The ears of patient eight (8a and 8b) represent the residual disease requiring further treatment. *Involvement of the drum was classified into categories A–D according to whether 1–25 per cent, 26–50 per cent, 51–75 per cent or 76–100 per cent of the drum was involved, respectively. yrs = years; M = male; L = left; Y = yes; F = female; R = right; N = no
Mean patient age was 32 years (range, 18–75 years). There were six females and eight males. The left side was affected for six ears and the right side for nine ears.
Myringitic features
Nine out of 15 ears had a history of otological intervention: 8 myringoplasties and 1 previous T-tube insertion (p = 0.4386) (Table 1). Of the eight ears that had a myringoplasty, five had reconstruction with temporalis fascia and three used cartilage.
The ear drum was divided into four quadrants or was considered central, when categorising the position of myringitis. The posterior inferior quadrant was involved in 6 out of 17 cases, the posterior superior quadrant was affected in 3 out of 17 cases, the anterior inferior quadrant was involved in 4 out of 17 cases, the anterior superior quadrant was affected in 1 out of 17 cases, and the myringitis was considered central in 3 out of 17 cases. The myringitis was marginal in 14 of the 17 times that the procedure was performed (76 per cent). The involvement of the drum was 1–25 per cent in 10 out of 17 treatments, 26–50 per cent in 4 treatments, 51–75 per cent in 1 treatment and 76–100 per cent in 2 treatments (Table 1).
Nearly all patients complained of otorrhoea from the affected ears (12 out of 15 ears) (Table 2).
Table 2. Symptoms reported in myringitic ears

Post-operative findings
At the first post-operative review, the appearance of the drum had improved in 10 out of 17 treatments (59 per cent). There was complete resolution at the first review in 7 out of 17 treatments (41 per cent). No ear was the same or worse than before (Table 3).
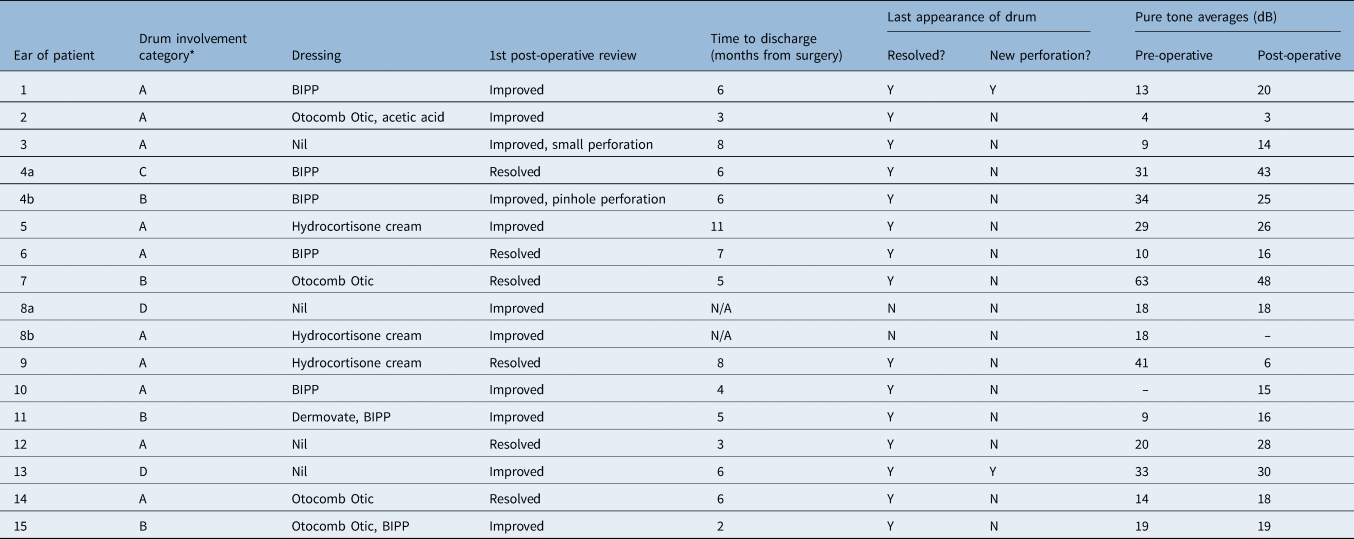
Table 3. Surgical procedure, post-operative findings, and pre- and post-operative pure tone averages

*Involvement of the drum was classified into categories A–D according to whether 1–25 per cent, 26–50 per cent, 51–75 per cent or 76–100 per cent of the drum was involved, respectively. Y = yes; N = no; BIPP = bismuth iodoform paraffin paste; N/A = not applicable
Fifteen of the 16 myringitis cases (94 per cent) had resolved after a single procedure with the KTP laser, as evident on subsequent follow up, and were discharged.
Regarding the extent of drum involvement, two patients were in the 76–100 per cent category. One of these cases failed to resolve even after two procedures, but the size of the involved area decreased each time. The other patient was completely free of myringitis at two months, but further follow up is needed. As there was only one case that did not resolve after one treatment, categorical analysis of size was not significant (p = 0.9242).
Patients could be discharged from 2 to 11 months after their procedure. The mean time to discharge or the documentation of a dry ear following surgery was 5.69 months (n = 13).
Procedural technique
We did not use standardised post-KTP laser treatment or packing; we varied what was placed in the ear depending upon the appearance of the deep canal, although bismuth iodoform paraffin paste was used most frequently, in 7 out of 17 cases. Otocomb Otic was used in four cases, steroid cream was used in four cases and nothing was used in four cases (Table 3). We found that the use of bismuth iodoform paraffin paste and steroid cream did not have a statistically significant impact on success (p = 0.6268 and p = 0.9248 respectively).
Complications
There was a new perforation noted in two patients at their first follow up. These perforations had resolved at the latest follow-up appointments (Table 4). Of the 17 cases, there was 1 other case of a permanent perforation, seen many months later (5.9 per cent).
Table 4. Follow up in 2020
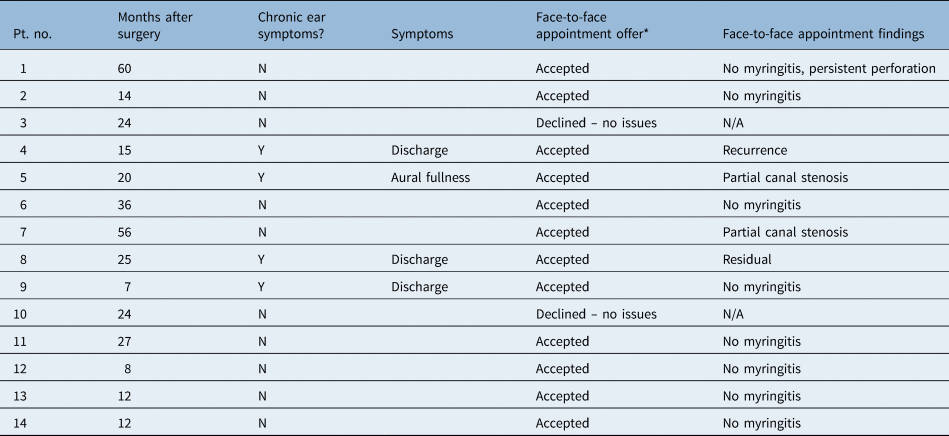
*Offered during telephone appointment. Pt. no. = patient number; N = no; Y = yes; N/A = not applicable
Of the 14 ears successfully treated, there was 1 later recurrence (7 per cent). Of the 15 ears treated, 1 patient received 2 procedures and experienced residual myringitis each time (7 per cent).
Two patients had a partial canal stenosis but no obvious granular myringitis. This was noticed after one year for one patient, and after two years for the other patient (Table 4).
Audiological outcomes
Pre- and post-intervention audiograms were reviewed for 12 patients (Table 2). Only one patient had a significant hearing loss (over 10 dB) after their first procedure, but this was shown to have improved after their second procedure (Table 3).
Follow up in 2020
All patients underwent telephone follow up in 2020 to assess for chronic ear symptoms. This resulted in a mean follow-up duration of 24 months (range, 7–60 months). All patients were also offered face-to-face follow up for examination. Four patients (28.6 per cent) reported chronic ear symptoms. Twelve patients attended a face-to-face follow-up appointment, of which eight had no evidence of myringitis (Table 4).
Discussion
Patient demographics
We did not identify any children that needed treatment; this supports previous findings indicating that myringitis is rare in children.Reference Levi, Ames, Gitman, Morlet and O'Reilly3
Myringitic features
Despite anecdotal views that previous otological intervention may predispose to myringitis, which may then be more recalcitrant to medical treatment and therefore require laser treatment, we found that this was not statistically significant.Reference Levi, Ames, Gitman, Morlet and O'Reilly3 We did not have enough patients to deduce whether particular graft material results in an increased risk of myringitis, although – again anecdotally – the presence of cartilage lying lateral to the drum's surface may be more likely to show persistent granulation. In those without a history of intervention, trauma to the epithelial layer of the tympanic membrane is likely to be the result of an infection, as the symptoms of the initial infection and subsequent myringitis may be difficult to differentiate. However, trauma and infection causing inflammation of the ear drum is common. For myringitis to become chronic, there must be inhibition of tympanic membrane re-epithelialisation.
The area that myringitis involved was variable and there did not seem to be a predisposition to a particular quadrant of the drum. We did, however, find that myringitis was more likely to involve the margin. This supports the findings of a study by Kim, in which 87.5 per cent of cases were marginal.Reference Kim6
Surgical outcomes
Cheung and Shiao showed that 22 out of 30 cases (73 per cent) had complete resolution after one procedure using a CO2 laser.Reference Cheng and Shiao12 Comparatively, Jung et al. found that 18 of the 21 patients (85 per cent) were cured after a single treatment.Reference Jung, Cho, Yoo, Lim and Chae9 In children, Fechner et al. showed resolution using the CO2 laser in 12 out of 15 ears (80 per cent).Reference Fechner, Cunningham and Eavey13 Our study demonstrates a similar success rate, of 94 per cent (15 out of 16), after a primary single treatment using the KTP laser.
Medical treatment depends on meticulous aural toileting, which may be restricted by clinic availability. Therefore, a single treatment rather than repeated clinic visits may be preferable for both the patient and healthcare provider.
Surgery is more complex than laser therapy, with inherently increased risk. Zhang et al. reported a 100 per cent resolution rate in 21 ears, achieved via excision of the fibrous layer and an overlay temporal fascia graft, with no reports of perforation after two years of follow up.Reference Zhang, Liu, Chen and Zheng14 El-Seifi and Fouad showed that only 2 out of the 48 patients treated surgically had recurrence, although the follow-up duration was short.Reference El-Seifi and Fouad4 One patient in that study had a new tympanic membrane perforation secondary to surgery. Surgery is more complex, and we feel it is best reserved for cases in which both medical and laser therapies have failed.
Other considerations
Although not statistically significant given the small number of patients, theoretically it makes sense that the size of the myringitis is more of a determinant of whether KTP laser tympanoplasty would be successful than its position. A larger myringitic area means a larger surface area that needs to be successfully treated with laser, with less of a relative leading edge of healthy epithelium available to migrate over this. This is what makes diffuse granular myringitis so difficult to treat, as there may be either no epithelium or just very inflamed epithelium present.
We did not find that post-operative treatment with steroid or bismuth iodoform paraffin paste had an effect on the success of treatment.
At the 2020 follow up, the same patients had recurrence and residual disease, suggesting that they have difficult-to-treat disease.
Complications
Only 1 patient out of 17 had a new permanent tympanic membrane perforation after laser treatment. Comparable alternatives to the KTP laser include silver nitrate cautery and CO2 laser. The issue with silver nitrate cautery is that it is relatively uncontrolled, with variable penetration, and therefore results in an unpredictable pattern of burning on a wet tympanic membrane. This can lead to perforations, which can then cause further issues. In a small study of 15 patients by van der Meer, 20 per cent of those who received treatment with silver nitrate cautery went on to have perforations.Reference van der Meer15 Laser treatment, however, is more precise and controllable. The KTP laser does have a variable penetration depth depending upon how it is used, and can be moderated both in terms of mode and power. There is a learning curve regarding achieving the correct distance needed to blanch and char the surface, whilst avoiding burning a hole through the drum.
In 2020, two patients were identified with partial canal stenosis. This could represent continuation of the underlying inflammatory process and is a recognised final stage of myringitis, as documented by Wolf et al.Reference Wolf, Primov-Fever, Barshack, Polack-Charcon and Kronenberg5 Alternatively, it could be a complication of the laser surgery, although it was not noted immediately following the operation. Interestingly, both patients no longer complained of otorrhoea.
Audiological outcomes
Hearing was not negatively impacted by our technique. The surface KTP laser technique appears to be safe, with a minimal impact on hearing, although risk is obviously present in terms of a perforation or blunting of the anterior tympanomeatal angle.
Patient discharge
Myringitis, if treated medically, requires many follow-up appointments, which is a burden both for the patient and the out-patient department. Definitive treatment that avoids this is therefore desirable, and we feel KTP laser treatment achieves this goal. We argue that this treatment should not be reserved only for patients who fail medical treatment, but could be offered at the time of myringitis diagnosis for timely resolution of the disease.
• Granular myringitis is a chronic and difficult-to-treat disease of the tympanic membrane
• There is no consensus regarding treatment
• Potassium titanyl phosphate (KTP) laser tympanoplasty is a minimally invasive option for treating granular myringitis
• There is a low rate of permanent perforation
• Hearing is not negatively affected by KTP laser tympanoplasty
Limitations
This study is limited by its retrospective nature and the lack of a control group. There are inconsistencies in long-term follow up given its retrospective nature. We have attempted to ameliorate this by completing an additional final telephone follow up with all 14 patients and face-to-face follow up in 12 patients. Statistical analysis has not been possible for non-categorical data given the small sample size and the lack of a control group. Statistically significant results have not been possible because of the small sample. Future research should address these limitations.
Conclusion
Potassium titanyl phosphate laser surface tympanoplasty is a useful tool in the armamentarium of ENT surgeons; it can provide safe, quick and effective resolution of granular myringitis. Secondary benefits include its greater efficiency, compared with the multiple out-patient appointments needed for aural toileting, and it reduces the burden to both the patient and out-patient clinic.
Data availability statement
The raw data collected are available from the corresponding author on request.
Competing interests
None declared