Introduction
Stapes surgery is the established surgical treatment for otosclerosis. The techniques and prostheses have evolved since the 1950s.Reference Causse, Causse, Wiet and Yoo 1 However, risks of sensorineural hearing loss, labyrinthitis, meningitis and facial paralysis still exist.Reference Causse, Causse, Wiet and Yoo 1 , Reference Glasscock, Storper, Haynes and Bohrer 2 Granuloma is a comparatively rare complication, first described in 1962,Reference Harris and Weiss 3 affecting 0.07 per centReference Seicshnaydre, Sismanis and Hughes 4 to 1.8 per cent of patients.Reference Burtner and Goodman 5 An excessive inflammatory reaction occurs, leading to granulomatous tissue formation around the prosthesis and oval window.Reference Fenton, Turner, Shirazi and Fagan 6
Symptoms typically manifest one to six weeks post-operativelyReference Mahadevaiah, Parikh and Kumaraswamy 7 as sensorineural dysacusis (70–100 per cent), vertigo (20–35 per cent), otalgia or tinnitus.Reference Seicshnaydre, Sismanis and Hughes 4 , Reference Wiet, Harvey and Bauer 8 – Reference Gacek 10 The precise aetiology is not fully understood.Reference Seicshnaydre, Sismanis and Hughes 4 Whilst a foreign body reaction remains the most probable explanation,Reference Burtner and Goodman 5 , Reference Kaufman and Schuknecht 9 , Reference Dawes, Cameron, Curry and Rannie 11 pyogenic inflammation, autoimmune responses, allergic reactions and excessive healing are alternative theories.Reference Mahadevaiah, Parikh and Kumaraswamy 7
We report three cases of severe post-stapedectomy granuloma, emphasising the variable presentation of this devastating complication and the challenges of its management.
Case report
Case one
A 40-year-old male developed intrusive tinnitus, dizziness, vomiting and diminished hearing 2 days after surgery involving left-sided stapedectomy with a fluoroplastic piston, performed in February 2010. Exploratory tympanotomy revealed a perilymph leak, and the oval window niche was packed with fat. Some clinical improvement transpired, although hearing failed to improve.
In April, the patient re-presented with left-sided House–Brackmann grade III facial weakness, otalgia and post-auricular pain, and severe sensorineural hearing loss. Otoscopically, the left drumhead appeared dull with a superior reddish hue; hence, systemic antibiotics and steroids were trialled. Magnetic resonance imaging (MRI) demonstrated a high signal in the middle ear and mastoid, implying granulomatous inflammation. A combined tympanomastoid approach revealed granulation tissue filling the aditus, epitympanum and mesotympanum, eroding the lateral semi-circular canal and extending into the inner ear. Granulations were cleared piecemeal and the prosthesis was left in situ at the patient's request. Gelfoam impregnated with dexamethasone was placed over remaining granulations adjacent to the dehiscent facial canal. Histopathology showed cuboidal epithelium, with an active chronic lymphoplasmacytic inflammatory infiltrate, and no aerobic or anaerobic growth. Post-operatively, facial function gradually recovered fully, although left otalgia persisted.
Follow-up MRI (conducted in July 2010) showed enhancing soft tissue in the mesotympanum, mastoid cavity, membranous labyrinth, external auditory canal and the lateral third of the internal auditory canal. Computed tomography (CT) showed extensive bony erosion of the otic capsule, advocating petrosectomy. Extensive, polypoidal granulomatous tissue was removed from the petromastoid. The lateral semi-circular canal was eroded and grossly involved, but the patient had pre-operatively refused labyrinthectomy because of concern about worsening imbalance. The facial canal was preserved and the granulomatous tissue was followed medially as permissible. The prosthesis was removed and the drumhead grafted where the granuloma had caused perforation.
Steady clinical improvement and reduced enhancement on serial MRI scans precluded further surgical intervention. Of note, the patient required admission in April 2015 for Pseudomonas aeruginosa meningitis, potentially related to previous ENT operations. He continues to be monitored annually.
Case two
In September 2011, a 55-year-old female underwent right-sided stapes surgery involving potassium titanyl phosphate laser stapedotomy and a SMart® Nitinol piston. Immediately post-operatively, profound vertigo persisted for 4 days, associated with vomiting and postural instability. She had a dead ear when the packs were removed two weeks later. Five months post-operatively, she presented with right-sided otalgia that failed to improve with oral antibiotics and steroids. Magnetic resonance imaging demonstrated inflammation throughout the middle ear and otic capsule, with extension into the internal auditory canal (Figures 1 and 2). This prompted exploratory tympanotomy in May 2012, whereby the bent prosthesis and surrounding inflammatory tissue filling the mesotympanum were removed.

Fig. 1 Post-contrast axial, T1-weighted magnetic resonance imaging scan of case two, from April 2012, demonstrating abnormal soft tissue enhancement in the vestibule and fundus of the right internal auditory canal.

Fig. 2 Coronal, T2-weighted magnetic resonance imaging scan of case two, showing a normal high-intensity signal for the inner-ear structures on the left, and an intermediate signal replacing the vestibule and membranous labyrinth on the right.
Despite radiological improvement, tinnitus, vertigo, imbalance and pain persisted, prompting tertiary referral. A tympanomastoidectomy and osseous labyrinthectomy were performed in June 2013. Extensive granulations were found throughout the petrous bone. All air cells containing disease were exenterated, and the incus and head of the malleus were removed. The semi-circular canals had been obliterated by fibrosis and ossification. Soft tissue was removed from the vestibule, oval window niche and the facial recess via a posterior tympanotomy; histopathology confirmed this as granulomatous tissue. Marginal symptomatic improvement was noted three months later, with reduced pain and vertigo.
At follow up in February 2014, the patient had deep otalgia radiating to the post-auricular area and neck. Subsequent MRI revealed mixed-signal material within the petrous cavity, indicative of recurrent granuloma formation. A right subtotal petrosectomy, fallopian bridge and blind end closure of the external auditory canal with abdominal fat graft was carried out in July following intensification of the otalgia and recent-onset facial numbness. The cavity was revised and all disease excised.
Post-operatively, the patient had grade IV, right-sided facial nerve palsy. Six months later, the facial weakness had resolved, but otalgia persisted, albeit less intensely. She is now reviewed annually with serial MRI.
Case three
A 63-year-old female underwent left-sided stapes surgery in June 2011. Two years later, she presented to her local hospital with left-sided pulsatile tinnitus, which was temporarily relieved by oral steroids. She subsequently developed otalgia and imbalance. An MRI scan demonstrated excessive inflammatory tissue in the left middle-ear cleft. Exploratory tympanotomy, performed in March 2013, instigated debulking of the granuloma and prosthesis removal.
In January 2015, tertiary referral was prompted by persistent tinnitus, vertigo and a three-week history of approximately twice-daily left-sided hemi-facial spasm, despite a course of oral prednisolone. Pure tone audiometry showed severe mixed hearing loss on that side. The left external auditory canal skin was erythematous, with narrowing of the deep meatus and scant pulsatile discharge. Urgent CT and MRI with contrast confirmed extensive reparative granuloma of the middle ear and otic capsule. Figures 3 and 4 show the extent of the inflammatory process.
Intra-operatively, a massive granuloma of the medial external auditory canal, middle ear, cochlea and vestibule involving the cochlear nerve and labyrinthine segment of the facial nerve was found and confirmed with histopathology. A left lateral petrosectomy, labyrinthectomy and blind sac closure of the external auditory canal was carried out. The majority of the petrous disease was removed, but some disease remained around the facial nerve and the fundus of the internal auditory canal. Steroids and ciprofloxacin were used to bathe the cavity.
Post-operatively, there were no surgical complications and the facial spasms fully resolved, although the pulsatile tinnitus remained.

Fig. 3 Axial, T2-weighted magnetic resonance imaging scan of case three, demonstrating loss of the normal inner-ear fluid signal on the left and oedema in the region of the brainstem cochlear nucleus.
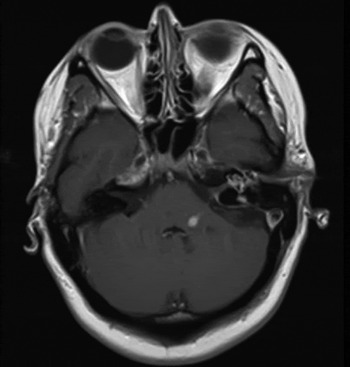
Fig. 4 Axial, T1-weighted, gadolinium-enhanced magnetic resonance imaging scan of case three, demonstrating enhancement of the middle ear, cochlea and internal auditory meatus on the left. Spread of enhancement is also seen along the VIIIth cranial nerve into the brainstem cochlear nucleus. A 6 mm, well-defined, oval-shaped enhancing lesion can be seen in the left middle cerebellar peduncle, around the level of the inferior aspect of the fourth ventricle.
Discussion
Granuloma should be suspected in any patient presenting with severe otological symptoms after stapes surgery. Typical otoscopic findings range from a slight reddening of the tympanic membrane to prominent granulations involving the external auditory canal.
Dual modality imaging is paramount to assess the extent of disease, plan surgery and assist in diagnosis. The CT and MRI findings correlated well with our intra-operative observations.
Case three presented two years after initial surgery, emphasising the variable presentation of this complication. In this case, we strongly suspect the granulomatous reaction spread along the VIIth and VIIIth cranial nerves to reach the cochlear nucleus. To the authors’ knowledge, this is the only reported case where the granuloma had tracked to the brainstem.
Histological examination classically reveals a localised collection of epithelioid histiocytes surrounded by lymphocytes. Histological assessment in all three cases revealed non-specific granulation tissue consistent with other literature reports.Reference Fenton, Turner, Shirazi and Fagan 6 , Reference Kaufman and Schuknecht 9 , Reference Gacek 10
Previously referred to as ‘reparative granuloma’, such terminology was often confused with ‘giant cell reparative granuloma’, which involves osteoclastic giant cells of the jaw and temporal bone. ‘Post-stapedectomy granuloma’ or ‘stapes surgery-induced granulation tissue’ are now the preferred terminologies.Reference Fenton, Turner, Shirazi and Fagan 6
Whilst foreign body reaction is widely believed the most likely aetiology, pathogenesis remains unclear. Fat, venous blood or GelfoamReference Seicshnaydre, Sismanis and Hughes 4 are commonly used during stapes surgery to surround the piston in the oval window, in order to minimise the risk of perilymphatic fistulaReference Shea 12 when a vein graft has not been used. Some evidence suggests that prosthetic material (for example Teflon, stainless steel or gold) does not influence granuloma formation.Reference Mahadevaiah, Parikh and Kumaraswamy 7 , Reference Kaufman and Schuknecht 9 , Reference Dawes, Cameron, Curry and Rannie 11 , Reference Tange, Schimanski, van Lange, Grolman and Zuur 13 Accidental foreign bodies, including cotton wool fibres and dust particles, have all been suspected to trigger this excess inflammatory reaction.Reference Dawes, Cameron, Curry and Rannie 11 Conversely, other studies demonstrate no such association.Reference Burtner and Goodman 5 , Reference Kaufman and Schuknecht 9 In case one, a perilymph leak following severe vomiting may have precipitated the post-operative granuloma.
Optimal management of post-stapedectomy granuloma remains contentious. A conservative approach with high-dose oral steroid and antibiotic treatment, as recommended by Seicshnaydre et al.,Reference Seicshnaydre, Sismanis and Hughes 4 was unsuccessfully trialled prior to surgery in all three of our cases. Some advocate immediate surgical exploration and prosthesis replacement;Reference Kaufman and Schuknecht 9 , Reference Gacek 10 others discourage surgery.Reference Hough and Dyer 14 Fenton et al. operated within a week of symptom onset in an attempt to preserve hearing.Reference Fenton, Turner, Shirazi and Fagan 6 Ideally, to reduce the risk of recurrence and minimise the potential for further foreign body reaction, total exenteration of granuloma with prosthesis removal would be followed by timely second-stage revision surgery and/or ossiculoplasty (if possible). In all our cases, profound sensorineural hearing loss had already been sustained prior to attempted definitive surgery.
-
• Granuloma is a rare complication of stapes surgery, with an extremely variable clinical presentation
-
• To the authors’ knowledge, this paper reports the only case of post-stapedectomy granuloma tracking to the brainstem
-
• Otalgia was a dominant feature in all cases
-
• Otalgia may be considered a potential red flag symptom of progressive, bony destruction and otic capsule involvement
-
• Optimal management of post-stapedectomy granuloma remains contentious
Hearing rehabilitation is a key consideration once the granuloma has been treated. In cases of dead ear, this may involve contralateral routing of stimulation, bone conducting solutions or cochlear implantation, depending on contralateral thresholds. Otalgia was a dominant feature in all our cases. We suggest this is a potential red flag symptom of progressive bony destruction and otic capsule involvement.
Conclusion
Whilst granuloma is a rare complication of stapes surgery, its occurrence remains unpredictable and the consequences devastating. Further multi-centre collaboration is crucial to better appreciate pathophysiology, devise optimum management strategies and ultimately improve patient outcomes.






