Introduction
Patients with unilateral vocal fold paralysis typically experience a hoarse, weak and easily tired voice. Quality of life is significantly reduced, and social and employment opportunities are compromised.Reference Fang, Li, Gliklich, Chen, Wang and Chuang1, Reference Smith, Gray, Verdolini and Lemke2 Therefore, maximal rehabilitation of the paralysed larynx is important for health and wellbeing and work prospects alike.
Rehabilitation of the paralysed larynx generally includes speech therapy during the first six months of the ‘watch and wait’ period. Where speech therapy alone is insufficient to improve the voice, surgical treatment is offered. The aim of surgical treatment for unilateral vocal fold paralysis is to achieve optimum glottic closure during voice production. Various surgical treatment options have been proposed, but, to date, there is insufficient evidence concerning the best surgical option to improve voice quality in patients with unilateral vocal fold paralysis. The treatment options include injection laryngoplasty, Isshiki type I thyroplasty, arytenoid adduction and laryngeal reinnervation.Reference Isshiki, Okamura and Ishikawa3–Reference Crumley and Izdebski6 Injection laryngoplasty using either ‘short-term’ or ‘long-term’ injectable materials can be performed under local or general anaesthesia, and repeat injections may be needed.Reference Mallur and Rosen7, Reference Carroll and Rosen8
Isshiki type I thyroplastyReference Isshiki, Okamura and Ishikawa3 is widely used to rehabilitate the permanently paralysed larynx.Reference McCulloch and Hoffman4, Reference McLean-Muse, Montgomery, Hillman, Varvares, Bunting and Doyle9–Reference Ryu, Nam, Han, Choi, Kim and Roh11 An implant is inserted through a window in the thyroid lamina cartilage of the larynx to medialise the paralysed vocal fold to the midline position. This allows the normal, non-paralysed vocal fold to make firm contact and produce a stronger voice during phonation. The procedure is commonly conducted under local anaesthesia as patients' co-operation is deemed necessary by most practitioners to fine-tune the voice according to implant size and placement.
Another approach is laryngeal reinnervation that restores the tone and bulk of the paralysed vocal fold,Reference Crumley, Izdebski and McMicken12 thus re-enabling pitch control and resulting in normal or near normal voice.Reference Lee, Milstein, Hicks, Akst and Esclamado13–Reference Wang, Chen, Chen, Li, Li and Xia15 Innervation of the larynx is re-established by anastomosing the injured recurrent laryngeal nerve to a donor nerve. A recent systematic review of studies on reinnervation revealed that there is a need for a prospective trial using standardised, internationally accepted outcomes.Reference Aynehchi, McCoul and Sundaram16 Such a trial, comparing reinnervation and thyroplasty in adult unilateral vocal fold paralysis patients, was attempted in the USA, but was suspended prematurely because of issues regarding obtaining informed consent and low accrual.Reference Paniello, Edgar, Kallogjeri and Piccirillo17 Within the small group of patients that did take part, the authors found no significant differences in voice quality between the two treatment groups. The experience highlights some of the commoner problems in surgical trials. The question of which surgical option delivers the most superior outcomes for patients with unilateral vocal fold paralysis remains unanswered because of the lack of strong evidence in the literature. Therefore, replication of the randomised, controlled trial (RCT) comparing reinnervation and Isshiki type I thyroplasty is necessary.
However, issues in terms of the recruitment of eligible patients in such RCTs require exploration. It is a problem inherent to RCTs in surgery because of factors such as patient preferences, the additional demand of the trial, the worry over uncertainty, and concern about information and consent.Reference Ross, Grant, Counsell, Gillespie, Russell and Prescott18 It has been recommended that patient recruitment be properly planned and piloted. Hence, a feasibility study that includes qualitative methods is necessary.Reference Lovato, Hill, Hertert, Hunninghake and Probstfield19
This qualitative study aimed to explore the views and beliefs of symptomatic unilateral vocal fold paralysis patients concerning the design of an RCT of laryngeal reinnervation versus thyroplasty. We also wanted to find out what issues concerned the patients most as regards to their voice.
Materials and methods
This study was approved by the local ethics committee. It was a prospective qualitative study that involved individual interviewing.
The study population comprised unilateral vocal fold paralysis patients who were eligible for the proposed randomised, controlled trial (RCT) of laryngeal reinnervation versus thyroplasty and who presented to the voice clinics of five London hospitals in the year 2011–2012.
Each eligible patient was given an information sheet. The principal investigator at the main site – the Royal National Throat, Nose and Ear Hospital – evaluated the patients further over a period of a month to confirm their eligibility. Subsequently, consent was sought for the interview session.
During the recruitment period, 69 unilateral vocal fold paralysis patients were identified, 17 of whom were eligible for the proposed RCT. Of these 17 patients, 10 (60 per cent) agreed to participate in the RCT and 40 per cent of them (4 of 10) were willing to be randomly allocated to a treatment group (Figure 1).
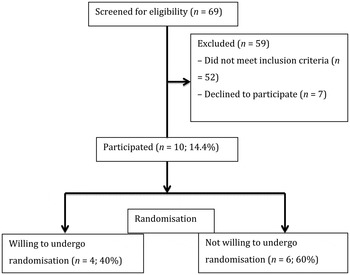
Fig. 1 Unilateral vocal fold paralysis patients identified in the clinics.
Eleven of the 17 patients (9 females and 2 males, with an age range of 18 to 65 years) agreed to be interviewed. Nine of these patients were English speakers, of various ethnicities. Their education level ranged from school leaver to degree holder. The causes of the unilateral vocal fold paralysis were thyroidectomy (five patients), thymectomy (one patient), vagal schwannoma excision (one patient), cervical spine procedure (one patient) and idiopathic origin (three patients). The duration of palsy was between 5 and 24 months. Of the 11 patients who were interviewed, 3 declined surgical intervention.
Information sheet
The information sheet explained the trial; it described the study design, the randomisation procedure, the thyroplasty and reinnervation procedures, the outcome measures, and the clinic visits required.
Interview sessions
Each individual interview was carried out in a dedicated room using a topic guide. The guide was a semi-structured questionnaire developed and based on discussions with ENT consultants and unilateral vocal fold paralysis patient representatives. It focused on the following topics: (1) the patients' voice complaints following unilateral vocal fold paralysis, (2) problems encountered as a result of the voice complaints, (3) patients' understanding of the surgical procedures, (4) patients' understanding of randomisation, (5) reasons for agreeing or disagreeing to take part in a research trial, and (6) reasons for agreeing or disagreeing to accept randomisation as part of this trial.
The interviews were conducted by the first author, a trained ENT surgeon. They were recorded digitally and saved as audio files.
Analysis
The audio files were anonymised and sent for transcription. The data were analysed using thematic analysis. The transcribed text was read repeatedly for familiarisation, and themes were subsequently extracted. Pen and paper were used to extract codes and identify the themes, and the data were managed using Microsoft Excel spreadsheet software.
Results
Voice complaints
The voice problems reported by the unilateral vocal fold paralysis patients during the interview are listed in Table I. The main complaint was that they lost the strength and volume of their voice, which affected their work and social life. Patients also complained of their voice being unpredictable, hoarse and tiring easily. Apart from voice issues, patients also reported reduced effort tolerance and mild aspiration.
Table I Voice complaints related to unilateral vocal fold paralysis

Associated problems
Problems encountered in the unilateral vocal fold paralysis patients' daily life are summarised in Table II. The unilateral vocal fold paralysis patients suffered decreased self-confidence at work as a result of the voice problems. They were unable to project their voice in meetings or express their opinion on the phone, as highlighted by the quotes below:
Table II Reported problems associated with voice issues

‘Even if I have an opinion, I kind of hold back’ (participant 4).
‘I would do other parts of my job and push another senior to do the phone calls’ (participant 4).
‘I do so much of my business over the telephone as well as being in large board room scenarios where people, unless they were sitting next to me, wouldn't be able to hear me. Even somebody sitting opposite me on the desk would have difficulty hearing me’ (participant 9).
Those who work outdoors or in a noisy environment found it hard to carry out their work, and one participant resorted to using a voice amplifier.
‘Hard to do with my job, especially outdoors, to raise the voice above a certain level’ (participant 3).
‘The kitchen is so noisy, the machines are on and things, so to scream or to get on top of your voice, you really need a quiet place’ (participant 6).
An actor who has stopped performing since the voice problem stated: ‘[I] haven't been able to work for maybe two years now, quite embarrassing sometimes’ (participant 1).
Patients isolated themselves from social gatherings, as they could not converse effectively with other people. The more they tried, the more their neck tensed up, which worsened and tired out the voice.
‘Socially, it bothers me if I couldn't go out and everyone's talking in a park when I just can't get involved in their conversation so I felt kind of isolated’ (participant 3).
‘I used to sing at church and I really enjoy my music. But with this problem now [I can't sing anymore] and as soon as I finished it [church], I go home. I don't stay back because there's no point seeing like, seeing people singing and you can't sing’ (participant 6).
Understanding of surgical procedures
Patients had read the information sheet and discussed the surgical procedures with ENT consultants prior to the interview. During the interview, the patients reported that they understood that thyroplasty is an old type of operation that involves an artificial implant which pushes the paralysed vocal fold and is technically easier than laryngeal reinnervation (Table III). They believed that it is temporary in nature and that it may need revision. With regard to laryngeal reinnervation, the patients perceived it to be a permanent and ‘natural’ type of operation that involves giving the paralysed vocal fold muscle a new nerve supply which makes it ‘alive again’ (Table III). However, the way that laryngeal reinnervation works was not properly understood. Some of the patients had thought that the procedure would re-establish the paralysed vocal fold movement.
Table III Patients' understanding of thyroplasty and laryngeal reinnervation

Understanding of randomisation
All patients said that the information sheet was clear and easily understood. Patients' understanding was further explored by asking them to describe the surgical techniques and randomisation procedure. Eight of 11 unilateral vocal fold paralysis patients understood the concept of randomisation (Table IV) and 3 of them agreed that randomisation was necessary. Only one patient did not really understand the meaning of randomisation, although they were still willing to be randomly allocated to a treatment group after a proper explanation had been given.
Table IV Patients' understanding of concept of randomisation

‘No guarantees as to which group you will be in’ (participant 2).
‘You get [a] 50-50 chance…. I think for out of 12 people, 6 people would have the injection, 6 people would have the rewiring…. But you don't have the choice. You would be … we would be chosen on an ad hoc basis…’ (participant 7).
‘Randomisation means that you are randomly selected for one or another treatment. So, it's the one … somebody will decide on your behalf as to how they're going to proceed with the treatment for you or how they are going to deal with it’ (participant 9).
Agreement to participate
Those unilateral vocal fold paralysis patients who agreed to participate were motivated by the desire to help other patients, as they believed the outcome of the research would improve the service and offer other patients a better treatment (altruism). Some patients felt that by participating they would get quicker and better treatment, and better treatment progress monitoring (self-interest) (Table V).
Table V Patients' reasons for agreeing or disagreeing to participate in trial

‘I am aware of studies needing to take place to allow progressive movement in research and, therefore, allow other people who may have my problem in the future [to] get the right and the best quality of care and treatment for their condition’ (participant 2).
Conversely, patients who declined to participate were worried about any further surgical interventions (anxiety). They did not want to undergo any surgery as they felt that such treatment was invasive and might cause unwanted complications. Although it was not stated by the patients themselves as reason for refusing to take part, it is important to note that many had negative experiences of surgery, as surgery was the cause of the unilateral vocal fold paralysis in these cases. Some patients said they were not ready to participate (personal reasons); such reasons may have been related to an inability to comply with the clinic visits requested because of busy schedules and the extra travelling required.
‘I understand the research, but at the moment, I don't think I want to go through it … too much going on in my life’ (participant 5).
‘I don't even like going to the dentist’ (participant 7).
Agreement to randomisation
Those unilateral vocal fold paralysis patients who agreed to the randomisation procedure perceived that both surgical options – reinnervation and thyroplasty – improved voice, although one of the patients was more interested in reinnervation than thyroplasty.
‘I was more intrigued by the nerve one, because in my head I had the feeling that that [reinnervation] would give me back more control; however, both [reinnervation and thyroplasty] have the same outcome’ (participant 1).
‘As you'd explained, both of them, all they do is put your vocal cord in the middle and set it so that the other cord makes it easier and you lose less breathe. So they both have the same outcome, you know’ (participant 1).
‘Because you're telling me both operations work’ (participant 4).
‘Both are good, aren't they?’ (participant 6).
The other factor that encouraged patients to agree on randomisation was that they still could have the other surgical option should the first one be unsuccessful.
‘Whichever group I end [up in], it's not contraindicated to having further treatment in the future…. They do both work and it's quicker than waiting…. Because you're telling me both operations work…. Whichever operation I have, my voice will improve’ (participant 4).
Those who did not agree to randomisation had strong treatment preferences. All of the patients who did not want to be randomly allocated to treatment groups chose reinnervation instead of thyroplasty. This is because they believed that reinnervation was permanent and natural, whereas thyroplasty was temporary and involved insertion of a ‘foreign body’, ‘plastic’ or ‘silicone wedge’ that may dislodge during vigorous exercise or athletic activity.
‘Nerve graft would've been a once, one-off operation if it's successful…. Better long-term option for my quality of life…. Seem[s] to be the best option to start with because we could always go back to the thyroplasty if the nerve graft failed…. The other operation, the alternative one, may not have been permanent…. Laryngeal reinnervation [is] more of [a] natural thing rather than having an implant… I think it's a lot to do [with] confidence as well’ (participant 3).
‘I'd prefer the nerve rewiring because I just don't like the idea of having just this … an extra wedge inside; I thought it'd be a bit more … natural…. I'd rather prefer to choose…. I don't want to do the old-fashioned way…. Personal preference – mainly based on talking to the speech therapist initially. He recommended it … silicone wedge over sort of boosting the nerves. I am still quite athletic…. If I had a silicone wedge, I think if I had a knock or a kick to the head…. Because I do boxing and rugby… it might get dislodged. If it didn't work, I would go with…. The wedge is plan-B to me…. From what I have read’ (participant 10).
‘I don't like a plastic going to … I don't like the thyroplasty idea … the side effects…. It's more natural – nerve rewiring. I've been researching with myself as well’ (participant 11).
The decision to undergo reinnervation instead of thyroplasty was influenced by patients' own research, by speaking to other patients who had undergone reinnervation, and by the ENT surgeons or speech therapists who saw them in the clinics.
‘I was not prepared to settle … for second best. It was clear to me that the best option and the only option for me would be reinnervation but the other two options are far too temporary. I thoroughly researched all of the options available. I suppose PB [ENT consultant] had given me some fairly clear indication just by being frank that the fact the other types of medialisation, the thyroplasty, the fact that it wasn't something that at this stage was expected to last longer than about 10 years, I believe MR [another ENT consultant] indicated that it was, you know, that both of those again were more shorter term options’ (participant 9).
Although these patients were aware that they could still undergo reinnervation if the thyroplasty did not work, they worried that they may not be eligible anymore because of a palsy cut-off duration for the trial and because of age, as reinnervation is thought to become less effective with age.
‘I wouldn't be able to have the reinnervation after three years, after my initial injury, which would be October 13…. I am 62 and my voice will probably change as I get older, I suppose I want to feel I have done everything I can to preserve my voice so that it won't actually deteriorate too much’ (participant 8).
Discussion
Randomised, controlled trials (RCTs) are widely proposed as the best method to evaluate the efficacy of certain treatments or surgical interventions. However, RCTs in surgery encounter methodological and practical challenges, greater than those of drug trials, because of factors including variations in surgeons' and patients' equipoise wherein one surgical option is preferred over the other. These challenges can lead to poor patient recruitment.Reference Ross, Grant, Counsell, Gillespie, Russell and Prescott18, Reference McCulloch, Taylor, Sasako, Lovett and Griffin20–Reference Abraham, Young and Solomon22 Some authors have recommended that a feasibility study which employs qualitative research methods is carried out so that patient recruitment can be properly planned.Reference Ross, Grant, Counsell, Gillespie, Russell and Prescott18, Reference Lovato, Hill, Hertert, Hunninghake and Probstfield19, Reference Murtagh, Thomson, May, Rapley, Heaven and Graham23, Reference Lewin, Glenton and Oxman24 Good qualitative studies can be major contributors to the success of RCTs in surgery. Therefore, we performed this qualitative study before embarking on the proposed RCT, in order to explore problems concerning patient recruitment and identify patients' main voice concerns.
Recruitment process
We explored the patients' views and beliefs after they had read an information sheet about the proposed study. Ethical committees require that information sheets are used to ensure shared treatment decision-making between clinicians and patients.Reference Charles, Whelan, Gafni, Reyno and Redko25 It is recommended that such sheets are clear but concise in explaining the study design, details of the procedure, and the advantages and side effects.Reference Mills, Donovan, Smith, Jacoby, Neal and Hamdy26, Reference Ellis, Butow and Tattersall27 The sheets can, however, influence patients' perception and reasoning, and ultimately affect recruitment to a trial.Reference Mills, Donovan, Smith, Jacoby, Neal and Hamdy26, Reference Edwards, Braunholtz, Lilford and Stevens28–Reference Donovan, Lane, Peters, Brindle, Salter and Gillatt30 Recruiters may use terminology that subconsciously encourages potential patients to prefer one treatment over another.Reference Mills, Donovan, Smith, Jacoby, Neal and Hamdy26, Reference Donovan29 Donovan et al. showed that the rate of patients agreeing to undergo randomisation was boosted after terminologies were changed in the written informed consent form.Reference Donovan29, Reference Donovan, Lane, Peters, Brindle, Salter and Gillatt30
In the present study, patients were given a minimum of two weeks to read through the study information sheet, prior to the interview. All patients were satisfied with the clarity of the content. The patients tended to describe reinnervation as a ‘natural’ and ‘permanent’ type of operation that makes the vocal fold ‘alive’ again. In contrast, the patients tended to explain thyroplasty as a ‘temporary’, ‘old-fashioned’ type of operation that involves using a ‘wedge’ or ‘plastic’ which is inserted into the neck to make the voice stronger, and considered it an operation that may need revision at some point. The presentation of the options in the literature, also provided verbally by recruiters, led to the patient perception that reinnervation might be a more ‘attractive’ option than thyroplasty; this represents a clear source of bias and lack of equipoise. The fact that the reinnervation cannot presently re-establish normal vocal fold movement, but rather aims to improve the tone and bulk of the vocal fold muscles should be conveyed effectively. The information sheets and recruiters should also emphasise that both types of operation have been shown repeatedly to be successful in strengthening the voices of unilateral vocal fold paralysis patients. However, we simply do not know which operation is better at addressing those concerns most important to the patients themselves.
Factors that motivated the patients to participate in the present study, such as altruism and self-benefit, were similar to those reasons reported by other studies.Reference Daugherty, Ratain, Grochowski, Stocking, Kodish and Mick31, Reference Featherstone and Donovan32 Conversely, patients who refused to participate considered the operation as invasive, had strong treatment preferences and regarded participation as time-consuming. Similar reasons have also been mentioned in previous studies.Reference Bevan, Chee, McGhee and McInnes33–Reference Alderson35 Eighty per cent of unilateral vocal fold paralysis patients in this study understood about randomisation and the importance of it, but could not accept the concept of equipoise or had a strong treatment preference. They wanted to be in control in making decisions as to which surgical option they would receive. Unilateral vocal fold paralysis patients who accepted that both treatments work to improve the voice, and hence had clinical equipoise, tended to accept randomisation.
Voice concerns
McCulloch et al. suggested that surgical researchers should run a feasibility study to identify suitable primary outcome measures.Reference McCulloch, Taylor, Sasako, Lovett and Griffin20 There has been no consensus to date on the primary outcome measures for trials evaluating the efficacy of treatments for unilateral vocal fold paralysis. Each of the three RCTs published to date used different primary outcome measures; these included a self-reported visual analogue scale of voice quality,Reference Hertegård, Hallén, Laurent, Lindström, Olofsson and Testad36 the well-validated voice handicap indexReference Jacobson, Johnson, Grywalski, Silbergleit, Jacobson and Benninger37, Reference Lau, Lee, Wong, Lim, Chan and Tan38 and perceptual evaluation of the voice by untrained listeners.Reference Paniello, Edgar, Kallogjeri and Piccirillo17 However, crucially, surgeons' choice of outcome measure might not truly represent patients' main concerns.Reference Ergina, Cook, Blazeby, Boutron, Clavien and Reeves21
• Randomised, controlled trials (RCTs) in surgery face many challenges, particularly patient recruitment issues
• A pre-RCT feasibility study is recommended to aid recruitment planning and identify patients' main concerns
• For an RCT of laryngeal reinnervation versus thyroplasty in unilateral vocal fold paralysis, certain phraseology used during recruitment needs to be changed or avoided
• Such changes may improve patients' willingness to be randomised
• The main concerns of unilateral vocal fold paralysis patients related to reduced voice strength and the subsequent effects on work and social life
• We propose using the voice handicap index 10 as the primary outcome measure
Here, we explored unilateral vocal fold paralysis patients' concerns about their voice to determine the primary outcome measure that is most likely to be meaningful to patients in a full trial. Their main concerns were found to be reduced voice strength and volume, and the resulting effects of this issue on work and social life. Therefore, we propose that the short and fully validated self-reported outcome tool, the voice handicap index 10,Reference Rosen, Lee, Osborne, Zullo and Murry39 should be used in future trials. Specifically, the tool incorporates items that measure the ability of the voice to compete against background noise and project. The voice handicap index 10 has been used in other retrospective and prospective trials involving unilateral vocal fold paralysis patients, and was able to demonstrate treatment effects before and after the operations.Reference Rosen, Murry, Zinn, Zullo and Sonbolian40–Reference Misono and Merati43 However, its sensitivity in detecting differences between reinnervation and thyroplasty in terms of outcomes is unknown. The interpretation of results using the voice handicap index must be done with caution in the proposed RCT, as the blinding of patients is not possible.
Conclusion
The study data were used to evaluate patient focus and optimisation of the trial protocol, and recruitment and consent processes. We identified phraseology that needed to be changed or avoided during the recruitment process. These changes may in turn improve the willingness of potential patients to be randomly allocated to treatment groups. We also propose using the voice handicap index 10 as the primary outcome measure in the proposed randomised, controlled trial.
Acknowledgement
The authors would like to thank all the patients for their participation in the study.








