Introduction
A large selection of paediatric tracheostomy tubes is available and suits a variety of individual requirements. In recent years, a small range of tubes has remained in favour for the majority of tracheostomised patients at our centres, although some patients continue to require other varieties on account of particular tube characteristics.
As in previous articles,Reference Irving, Jones, Bailey and Melville1–Reference Tweedie, Skilbeck, Cooke and Wyatt3 we separate the tubes into silicone, polyvinyl chloride (PVC) and metal varieties. We discuss their features and uses, and include an updated sizing chart (Figure 1). This update also includes a number of important design changes to some of the existing tubes.
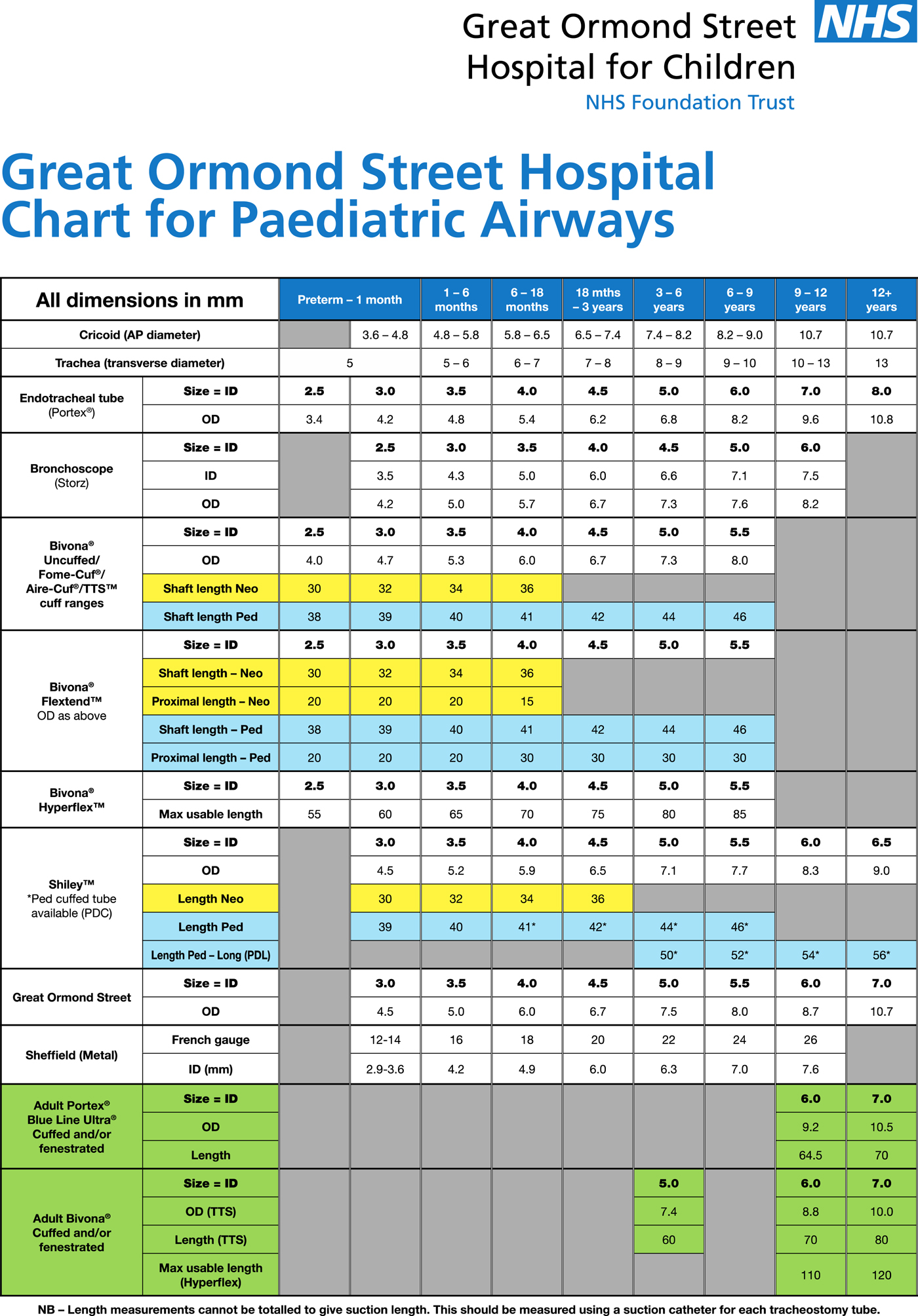
Fig. 1. Great Ormond Street Hospital sizing chart for paediatric airways (2016). AP = anteroposterior; ID = inner diameter; OD = outer diameter
Tracheostomy multidisciplinary team
The importance of a multidisciplinary approach to children with tracheostomies, at every stage, cannot be overstated, from pre-operative discussions to long-term care and, it is hoped, eventual decannulation. Patient safety and tolerance is central to these considerations. Aside from issues of safety, stoma care and ongoing management of airway pathology, many of these children have other physical, medical, developmental, communicational and psychological problems that must be addressed in parallel. Additionally, the long-term impact on their families and other carers should not be overlooked.
Our in-hospital teams comprise ward nurses, medical staff, play specialists, social workers, speech and language therapists, and dedicated clinical nurse specialists. It is also vital that close links are established with patients’ local hospitals, allied professionals in their communities and support groups, facilitating education, equipment provision and respite care, for example.
Silicone tracheostomy tubes
Portex Bivona tracheostomy tubes
The Portex Bivona silicone tracheostomy tube (Smiths Medical, Ashford, UK) continues to be the most commonly used tube at our centres, having largely replaced other varieties for reasons of comfort and versatility.
Figure 2 shows some examples of tracheostomy tubes. Other Portex tubes, and Shiley and Tracoe products, are occasionally used as alternatives to the Bivona. Tubes are classified as uncuffed or cuffed, and all varieties intended for paediatric use have a single lumen.

Fig. 2. Examples of paediatric tracheostomy tubes: (a) Bivona tracheostomy tube (straight neck flange); (b) Bivona FlexTend TTS (tight-to-shaft) cuffed tracheostomy tube (V neck flange); and (c) Bivona Hyperflex uncuffed tracheostomy tube (adjustable ‘V’ shaped neck flange).
The versatile Portex Bivona range includes a large variety of tube dimensions (both uncuffed and cuffed), with the additional option of integrated attachments to suit particular clinical circumstances. Additionally, Portex Bivona offers a tube customisation service to allow further modifications to these products.
The Portex Bivona range (now in its fourth series (‘T4’)) is based around a standard shaft manufactured from opaque siliconised PVC. The shaft is latex-free and hydrophobic. This hinders protein adhesion, and thereby limits secretion build-up and bacterial colonisation. This has particular advantages in small calibre, single lumen paediatric tubes, facilitating suction, reducing tube blockage risks and allowing more infrequent (monthly) tube changes. Additionally, in our experience, we have found that the incidence of external granulation may be significantly less with these siliconised tubes, in comparison to their simple PVC counterparts.
The silicone shaft is reinforced with a kink-resistant wire coil, producing a tube that is flexible and conforms to the shape of the trachea. The wire insert may render this range incompatible with magnetic resonance imaging (MRI), necessitating an alternative in these circumstances. A new range of tubes is now available, containing a reduced amount of ferromagnetic metal, and is ‘MRI-conditional’, suitable for scanners of 3 Tesla or less. Full compatibility details are available in the package insert. These tubes do, however, result in the appearance of artefacts in scanning, and are therefore not recommended for head and neck imaging. We recommend that the tracheostomy tube is always changed to a PVC alternative for scanning.
The current range includes new contoured flange designs, for improved comfort. These are the Neo and Ped ‘V’, the Ped Straight (with flanges of 60 mm from end to end), and a Neo Straight (46 mm flanges), with larger eyelets for easier threading of tracheostomy tapes. We would generally favour straight flanges in children under one year of age, as these tend to sit more comfortably in infants with short necks and overhanging chins. The ‘V’ type is generally suited to older children, although the overall neck shape, chin size and craniofacial dimensions are generally more pertinent considerations in flange selection than age alone.
The connector design has also changed. Instead of the former swivelling 15 mm connector, current tubes have a fixed connector moulded into the flange, reducing bulk and eliminating grooves between the components to facilitate cleaning. These tubes can also be customised to a swivel 15 mm connector.
The design of the tube cuffs and obturators in this range has also changed slightly since previous versions. The cuffs now have ridges at either end – ‘glue dams’ – to improve inflation and symmetry, and the obturators have been modified to have hemispherical tips that fit more snugly against the edges of the tube lumen, thereby reducing insertion-related trauma. Additionally, neonatal tubes now have their own specific obturators, rather than the previously used paediatric obturators with spacers.
Each tube is supplied with half-inch twill tape ties, although we prefer quarter-inch tapes for all children, as the thicker tapes will not pass easily through the eyelets of paediatric tube flanges and are more suited to adult use. A disconnection wedge is provided to facilitate separation of any connected appliances from the tube. The wedge slides between the two items; once a click sound is heard, the device will gently slide off the end of the tracheostomy tube.
The standard uncuffed tube is available in neonatal (‘Neo’) and paediatric (‘Ped’) lengths, with an unchanged range of inner diameters (2.5–4.0 mm and 2.5–5.5 mm, respectively).
In our experience, Bivona tubes can usually be left in situ for up to 28 days without the need for changing. Unlike most other silicone products, they are steam autoclaveable and paediatric tubes can be re-used up to five times, subject to the continued integrity of the tube (10 times in adults). This substantially reduces the costs of supply for individual patients. Guidelines have been drawn up for in-hospital sterilisation (with enzymatic cleaners and autoclaves) and at home (with baby bottle steam sterilisers). Additionally, sealed Bivona tubes that are found to be past their expiry date may be safely autoclaved and used.
Importantly, the adult versions of Bivona tracheostomy tubes offer similar features to the paediatric range. They also have the added advantage of being slightly shorter than some of the other adult tubes on the market. Together with their soft flanges and other innovative accessories, this shorter size may offer advantages in adolescent patients for whom paediatric tubes are no longer suitable. A smooth transition between child and adult tubes can also be achieved with both the cuffed and uncuffed ranges. Of note, the outer diameter and shaft length of the adult range are significantly greater than the paediatric range. Adult Bivona tubes also do not contain metal.
A Hyperflex™ version of the tube is available in paediatric sizes (2.5–5.5 mm inner diameter). The long shaft has an embedded stainless steel coil as an added safeguard against compression, and an adjustable flange. This permits alteration of the intra-tracheal tube length without the hazards of extubation. This is particularly useful for those children with unusual tracheal anatomy or pathology (such as distal tracheomalacia, granulations and abnormal tracheal length), who might eventually require a customised tube. Importantly, because of the potential risks of flange slippage, we recommend that Hyperflex tubes should not be used at home. Even when used in hospital, they should be replaced with a fixed-flange customised alternative as soon as possible.
The FlexTend™ Plus tube has a similar embedded coil, but has a fixed flange and a long, flexible external end, which increases the distance between the tube connections and the child's neck. This is an important consideration in babies and young children with poor head control and/or short necks, who are otherwise prone to tube obstruction by their chins. The extension also facilitates attachment and disconnection of ventilator tubing when long-term respiratory support is required. Importantly, the external and internal components of the tube are constructed as separate segments, reducing the risk of tube obstruction if the extension is pulled or twisted by the child or ventilator tubing. However, it is essential that a disconnection wedge is used to separate the tube from ventilator circuits and other attachments, rather than pulling them apart, as the extension is liable to be damaged, risking tube occlusion. The FlexTend is available with standard neonatal and paediatric shaft lengths and diameters, in uncuffed and now in TTS™ cuffed versions, as described below.
There are three types of cuffed Bivona tracheostomy tube: Aire-Cuf®, TTS and Fome-Cuf®. Of note, the Aire-Cuf has a blue pilot balloon, the TTS has a clear pilot balloon and the Fome-Cuf has a red pilot balloon.
The Aire-Cuf comprises a standard tube with an added air-filled cuff. This is useful for protection from aspiration and for minimising air leak during ventilation. The product is available in appropriate neonatal and paediatric dimensions. It is not commonly used for two main reasons. When inflated for long periods, the cuff may cause pressure necrosis of the tracheal mucosa. Cuff pressure may be best measured using an appropriate manometer. When fully deflated, the collapsed cuff drops around the shaft of the tube, limiting air leak.
The TTS (tight-to-shaft) tube is a useful alternative. It is our cuffed tube of choice. The TTS cuff has a low-volume, high-pressure design, and is inflated with water rather than air, which may diffuse through the cuff wall. The cuff may be inflated during meals and at night to protect the airway when aspiration is most likely, or during periods of ventilatory support (e.g. overnight). At other times, the cuff can be deflated completely to assume the profile of an uncuffed tube. This is useful at the time of insertion, minimising trauma to the stoma and trachea, and when weaning a child from a ventilator. This feature also allows air to leak around the shaft for periods of phonation, when a speaking valve may be attached safely (the cuff must be down).
Importantly, as the TTS cuff is filled with water, high pressure is exerted on the tracheal wall. Cuff pressures are more difficult to maintain reliably than with air-filled or foam-filled cuffs, such that we would not recommend the TTS for long-term use. A manometer cannot be used with a water-filled cuff, unlike an air-filled cuff. Regular cuff deflations must be performed in order to protect the tracheal lining from prolonged pressure injury and subsequent stenosis risk. The frequency of cuff deflations varies according to inflation volumes, which must be clearly recorded, and cuff-use duration. We typically recommend cuff deflation every 2 hours for 5–10 minutes, if tolerated. With regard to the amount of air or water a cuff should be inflated with, an air-filled cuff should be monitored with an appropriate manometer. For the TTS tube, the amount of water should be slowly titrated to a level that minimises an air leak in the artificially ventilated patient.
A Fome-Cuf version is also available. This is a self-inflating foam rubber filled cuff that can be inflated permanently. It is useful in those children with chronic severe aspiration, when long-term protection of the airway is required. The foam is self-inflating, conforming to the dimensions of the trachea. It adjusts to changes in pressure during the ventilation cycle, while maintaining a low cuff-to-wall sealing pressure. A syringe and three-way tap should be available in the event of any tube change. It is essential to appreciate that, owing to the self-expanding nature of the foam, the cuff may be deflated somewhat using a syringe, but will not fully collapse. This means that removal and/or reinsertion of this tube, particularly in a small child or in the context of a new stoma, may be difficult. A TTS tube should be available as a back-up; this would be the first-line response during an emergency tube change. The tubes can be fitted with a ‘talk attachment’. This is a finger-controlled valve that allows airflow above the cuff to aid speech. In our children, we primarily use this to facilitate removal of secretions that accumulate above the cuff, thereby avoiding the risks of conventional cuff deflation, to allow suction from below.
Portex Bivona customised tracheostomy tube service
This option is available to address specific difficulties. Individual requirements of the patient (shaft style, curvature, length, diameter and flange position) are submitted. The company aims to provide a non-sterile tube within one week, which can be autoclaved before use.
Polyvinyl chloride tubes
Shiley tracheostomy tubes
The Shiley product range (Covidien, Dublin, Ireland) is manufactured from opaque, thermosensitive PVC (latex-free), with a thin-walled shaft, tapered tip and universal fixed 15 mm connector. Uncuffed tubes are available in neonatal (‘Neo’), standard paediatric (‘Ped’) and paediatric long (‘PDL’) varieties, with the latter being 10–15 per cent longer than their standard counterparts. Air-filled, cylindrical, low-pressure cuffed tubes are produced in standard paediatric (‘PDC’) and paediatric long (‘PLC’) versions. All Shiley tubes feature a recessed area behind the connector for increased comfort, and the neonatal tubes also have a lower flange for improved fit. Customisation services are also available.
Unlike the Bivona range, Shiley tubes are not re-useable, but may remain in situ for up to 29 days. However, we recommend weekly changes, as the tubes may become coated and blocked by secretions, which in our experience is more likely than with siliconised tubes.
Although the Bivona range is now more commonly used at our centres, an ‘off the shelf’ long paediatric tube (size 5.0–6.5 mm) is manufactured only by Shiley, offering a unique option for a limited number of children who require a tube that is midway between typical paediatric and adult lengths. Similarly, a 4.5 mm neonatal length tube is available in a Shiley version, but not as a Bivona. The Hyperflex and customised tubes may offer alternatives in the Portex Bivona range.
Given that the Shiley tubes contain no metallic components, they are MRI-compatible. We also favour them for use in our tracheostomy emergency boxes, provided in a half-size smaller than the child's typical tube. The Shiley shaft, made of PVC, is typically stiffer than the siliconised Bivona equivalent, and is therefore more suited to being ‘railroaded’ into the stoma over a suction catheter in an emergency.
Table 1 compares the principal features of the Portex Bivona and Shiley paediatric tracheostomy tube ranges.
Table 1. Comparison of Portex Bivona and Shiley tracheostomy tube features
Information correct at time of publication. For full information, refer to detailed product-specific information. *Maximum recommended routine tube change frequency. PVC = polyvinyl chloride; MRI = magnetic resonance imaging
Tracoe mini tracheostomy tubes
Tracoe tubes (Tracoe Medical, Nieder-Olm, Germany) are manufactured from white, radio-opaque PVC, and include a built-in 15 mm universal connector. The wall of the shaft is particularly thin, but flexible and kink-resistant. An obturator is included, featuring a ‘ring-pull’ type handle. The tubes are intended for single use only; as for the Shiley, we recommend a weekly tube change.
Neonatal length tubes (the ‘350’ series) are available in a variety of sizes, from 2.5 to 4.0 mm internal diameter. Standard paediatric-length tubes (the ‘355’ series) range from 2.5 to 6.0 mm. Importantly, the Tracoe mini range includes the only 6.0 mm paediatric-length tube; this is useful for a number of patients (particularly small adolescents) who cannot tolerate an adult-length product.
Portex ‘555’ series paediatric tracheostomy tubes
This tube is rarely used in our practice; however, use varies worldwide. The ‘555’ tube is made from blue opaque PVC that is thermosensitive. It is therefore quite stiff and easy to handle, with an obturator for the time of insertion. It soon softens at body temperature, allowing it to conform to the shape of the child's trachea. This improves comfort and reduces the risk of mucosal damage. Like the Bivona, the ‘555’ has a contoured flange to secure the tube comfortably and with minimal movement. A 15 mm (universally compatible) clear plastic connector allows easy visualisation of any secretions and, like the FlexTend, makes occlusion by the chin less probable. Also supplied are a disconnection wedge and a double-swivel connector, which can reduce torque from a ventilator circuit. As with a Shiley tube, these tubes are single use only and may require weekly changes because of the adherence of secretions.
Portex Blue Line® paediatric tracheostomy tubes
This range is also manufactured from clear, thermosensitive PVC, as for the ‘555’ series, allowing easy insertion and conformation to the trachea. The ‘Blue Line’ refers to the blue radio-opaque strip running along the tube, facilitating radiological assessment of its position. The product is available in a full range of paediatric and adult sizes, with or without connectors and/or fenestrations. It is designed for single use only.
Great Ormond Street tracheostomy tube
Rarely used in recent years, this tube is now no longer manufactured. Importantly, in the unlikely event of a child presenting with such a tube in situ, it is not compatible with standard ventilator tubing or resuscitation equipment. A Portex male/female adaptor of appropriate size will be required in emergency situations.
Metal tracheostomy tubes
A number of silver metal tubes have been developed. Their designs and general principles have remained unchanged since previous articles.Reference Irving, Jones, Bailey and Melville1–Reference Tweedie, Skilbeck, Cooke and Wyatt3 While seldom used by children in our departments, silver tubes have some important qualities that confer advantages over non-metal varieties in certain circumstances. Most significantly, the tubes can be manufactured with very thin walls, permitting the use of an inner tube without compromising airflow. This can be removed and cleaned without taking out the whole tube. Silver tubes may remain in situ for up to 29 days. Additionally, some older children who are more image-conscious prefer the appearance of the silver tubes to their plastic counterparts.
However, silver tubes have certain disadvantages. For example, they are rigid and do not conform to the trachea, which some children find uncomfortable. Additionally, each tube is unique: the unit cost is high (although far fewer tubes are required in the long term) and the components are not interchangeable, creating compatibility problems. As a consequence, particular emergency equipment should be provided with these tubes, including a male-to-female adaptor to allow connection to ventilator circuits. Sizes are measured in the French gauge (Fr) and are not comparable to the metric measurements of the plastic tubes. They are not compatible with MRI scanning, and they may distort computed tomography images of the head and neck. A change to a PVC tube is recommended in these circumstances.
The Sheffield tube is currently the only silver product used at our centres, although the other tubes are described for reference purposes.
Sheffield tracheostomy tube
This is the newest variety of silver tube. The range of included accessories addresses the major disadvantages of previous types, and it is therefore our silver tube of choice. It is supplied in six parts, each of which may also be ordered individually, as required: a fenestrated outer tube with slim flanges and a retaining safety clip, three inner cannulae (two plain and unvalved, one fenestrated and valved), an introducer, and a full-length obturator. One plain inner tube may be kept in situ while the other is cleaned, with the further option of a valved tube for certain children. Additionally, the full-length obturator is invaluable during decannulation to prevent crust aggregation near the tip. When the tube is in situ, it lies flush to the skin. In addition, the flanges are rather less bulky than those of other tubes, suiting most paediatric neck dimensions.
Negus tracheostomy tube
This tube is supplied in four parts: a plain outer tube, a choice of two inner tubes (plain or with a speaking valve) and an introducer. In addition to the general disadvantages of the silver varieties, the outer tube of the Negus lacks a safety catch, allowing the inner tube to be coughed out inadvertently. Another consideration is the limited selection of supplied inner tubes: if the plain inner cannula is removed for cleaning, its valved counterpart is the only replacement supplied with the tube. This can create problems for those children who cannot tolerate the valve; during cleaning periods, the outer tube alone may have to be used.
Chevalier-Jackson tracheostomy tube
This tube is similar to the Negus, but is supplied in three parts: a plain outer tube, a plain inner tube and an introducer. Additionally, it is longer than the Negus and has a safety catch to secure the inner cannula. The added length makes it particularly useful for bypassing areas of tracheal stenosis or tracheomalacia. Unfortunately, a speaking-valved version of the tube is not available, thereby limiting its applications.
Alder-Hey tracheostomy tube
This tube comprises five parts: a fenestrated outer tube, valved and unvalved fenestrated inner tubes, an introducer, and an obturator. The neck plate of the outer tube is adjustable, enabling the position of the fenestrations to be altered, although the plate itself is rather large, precluding its use in most infants.
Montgomery Safe-T-Tube
The Montgomery Safe-T-Tube (Boston Medical Products, Shrewsbury, Massachusetts, USA) is unlike conventional tracheostomy tubes, but it is suited to certain limited paediatric applications. It is a T-shaped silicone stent (‘T-tube’) comprising a long principal lumen, and a shorter lumen projecting from its side at 75 or 90 degrees. Such stents have been used successfully to support adult airways, for tracheal stenosis and tracheomalacia, and following reconstructive surgery.Reference Phillips, Kubba, Hartley and Albert4, Reference Stern, Willging and Cotton5 The limbs of the principal lumen can be trimmed: the lower limb of the stent can extend as far as necessary down the trachea towards the carina, while the upper limb can sit either below or above the glottis, depending on the clinical situation. The short limb is brought out through a tracheostomy and trimmed to a convenient length. The use and tailoring of a T-tube is complex and typically individualised.
The T-tube is particularly useful as an alternative to a typical tracheostomy tube in those complex cases where stenting around the level of the larynx is required. It is generally well tolerated and can be left in situ for months at a time. Although not associated with excessive peri-stomal granulation tissue formation, tenacious crusts may accumulate within the tube, putting the airway at risk. It is important that parents and medical staff are aware of the atypical nature of the T-tube, which may have to be pulled out and replaced with a conventional tube in the unusual event of complete obstruction. Limitations of tube size (smallest outer diameter is 6 mm) and associated significant risk of blockage prohibit T-tube use in younger children.
Tracheostomy tapes
For safety reasons, all tracheostomy tubes of children managed at the Great Ormond Street Hospital for Children are currently secured with Marpac tracheostomy tube holder tapes (Albuquerque, New Mexico, USA), as opposed to Velcro®-based alternatives. Marpac ties provide a comfortable, latex-free holder to secure the tracheostomy tube. They are made of soft, breathable foam, with twill tie adjustments.
We favour Trachi-Dress stoma dressings (Kapitex Healthcare, Wetherby, UK) for routine use. They are composed of three layers of polyethylene and viscose, which are non-adherent and absorb secretions effectively.
Appropriate tracheostomy tape-tying technique is of utmost importance. Tapes should be secure and prevent accidental decannulation, but should not be overly tight so as to result in breakdown and excoriation of the underlying skin. Tension should be checked by comfortably placing only one finger between the neck and the tapes. Knots should be tied at the front of the neck.
Tracheostomy emergency box
All tracheostomised children are provided with an emergency box that remains with them at all times. This contains a spare tracheostomy tube (same size and type as is worn), a Shiley tube that is a half-size smaller (regardless of the child's normal tube type, for easier insertion in an emergency), water-based lubricant jelly, round-ended scissors, spare tapes and a spare suction catheter (the same size as the child's typical catheters). In an emergency, the suction catheter may be inserted into the stoma, allowing the tube to be ‘railroaded’ over it. Children are discharged with three additional items: Velcro tapes (to facilitate tube changes by one carer working alone), a disconnection wedge and a valve pocket mask to aid emergency ventilation when basic life measures are required.
One-way (speaking) valves
A number of one-way valves are currently used at Great Ormond Street Hospital for Children, particularly the Rüsch and Passy-Muir varieties. All have similar components (a body and flap), but vary in design. The Rüsch and most other valves are bias-open, closing only on expiration, and are open at all other times. However, the Passy-Muir valve is bias-closed and opens only for inspiration. As well as diverting airflow through the glottis for potential vocalisation, valves offer a useful means of assessing a child's ability to adapt to oral breathing when decannulation is considered. Use of a one-way valve is dictated by the laryngotracheal anatomy and the relative size of the tracheostomy tube cannula to the airway lumen.
Rüsch speaking valve
The Rüsch valve (Teleflex Medical Europe, Athlone, Ireland), is preferred for initial assessment, being easily available and relatively inexpensive. In addition, it is bias-open and allows some air leakage during exhalation, which is of particular value in those patients with limited peak expiratory flow and/or supra-stomal obstruction.
Passy-Muir valve
The Passy-Muir valve (Kapitex Healthcare) comprises a plastic body and a clear one-way valve flap, and is universally compatible with 15 mm tubes and connectors. It requires daily cleaning with soapy water. The Passy-Muir valve is bias-closed, with no leak around the valve. This creates a closed system that maintains a column of air in the trachea, thereby mimicking normal laryngopharyngeal physiology and allowing the development of positive supraglottic pressure. This optimises voice production, aids coughing and improves swallowing. Full closure of the system during expiration has the added advantage of limiting the accumulation of airway secretions within the tube and valve.
The Passy-Muir valve is the valve of choice for long-term use, but its bias-closed, no-leak design creates a number of potential limitations. The valve cannot be used in conjunction with an inflated cuffed tube, a particular consideration in children at risk of aspiration. Some children struggle with the Passy-Muir valve during expiration, but may still tolerate the Rüsch or other bias-open valve types.
Shiley speaking valve
The Shiley valve is no longer in routine use at Great Ormond Street Hospital for Children, although it is occasionally used by children transferred from other centres. It comprises a white 15 mm diameter plastic body (universally compatible) with a flip cap to allow access to the tube for cleaning. The flap is clear and delicate, with low resistance during respiration. The valve is therefore quiet, lightweight and well tolerated.
Heat and moisture exchangers
Maintenance of the humidity and warmth of inspired air is an essential part of tracheostomy management, as the normal functions of the upper respiratory tract have been bypassed by the tracheostomy. Inspiration of cool and dry air may create many problems for the tracheostomised child. Impairment and destruction of cilia reduce the proximal transportation of mucus. Secretions become increasingly thick and tenacious, making their expulsion difficult, which may lead to blockage of the tube. Additionally, cold inspired air increases heat loss from the respiratory tract, a particular danger for the small infant.
Such problems may be overcome in the hospital environment by nebulisers and humidifiers for ventilation circuits. Heat and moisture exchangers are more suitable for definitive and long-term use. These consist of multiple layers of water-repellent paper or foam membranes, which trap heat and moisture during exhalation. Cold inhaled air is then warmed and moisturised, thus maintaining the optimum respiratory tract environment.
Several varieties of heat and moisture exchanger may be used, but a number of important aspects should be considered. Firstly, the selected heat and moisture exchanger must be appropriate to the particular child's tidal volume (6–8 ml/kg), in order to limit resistance to airflow and prevent carbon dioxide retention. The heat and moisture exchanger must also be lightweight to avoid traction to the tracheostomy tube, which might cause skin irritation or even accidental decannulation. Additionally, the internal volume of the heat and moisture exchanger will add to respiratory dead space (already 2–2.5 ml/kg), increasing the work of breathing. This may be further exacerbated by the accumulation of secretions within the device. Manufacturers therefore recommend changing the heat and moisture exchanger daily or whenever contaminated.
Figure 3 shows examples of heat and moisture exchangers. We currently routinely use four types of heat and moisture exchanger: the Gibeck Humid-Vent Mini, the Thermovent T, the TrachPhone and the ProTrach DualCare, which are described below.

Fig. 3. Examples of heat and moisture exchangers. Left to right: Thermovent T, Gibeck Humid-Vent Mini and TrachPhone.
Gibeck Humid-Vent Mini
The Gibeck Humid-Vent Mini (Teleflex Medical Europe), or ‘mini vent’, is designed specifically for neonatal patients. The device protrudes from the tracheostomy, preventing occlusion of the tube by the neck. It has a standard 15 mm internal diameter and 15 mm outer diameter connector. It provides a moisture output of over 30 mg H2O/l at 20 ml tidal volume, with only 2.4 ml of added dead space. It is not possible to deliver oxygen through this device.
Thermovent T
The Thermovent T (Smiths Medical) is suitable for spontaneously breathing patients with a tracheostomy tube. It has a low profile design, and is designed to ensure maximum comfort with minimal protrusion. The high performance, double paper element makes it an efficient heat and moisture exchanger, with minimal resistance to flow. Consideration should be given to the tidal volume of the child; it is our recommendation that this heat and moisture exchanger is used for children over 10 kg in weight. Moisture output is 25 mg H2O/l at 500 ml tidal volume.
TrachPhone
The TrachPhone (Atos Medical, Colwick, UK) is a lightweight 2.9 g standard, 15 mm heat and moisture exchanger, intended for spontaneously breathing patients. It also has a valve for forced inspiration and expiration or suctioning, and a built-in oxygen port. It has a spring lid that can easily be occluded by a finger to facilitate speech. After releasing the finger, the lid falls forward automatically.
ProTrach DualCare
The ProTrach DualCare (Atos Medical) combines a speaking valve with a heat and moisture exchanger. The switch between the speaking mode and heat and moisture exchanger mode is achieved by twisting the lid of the speaking valve. On exhalation, the air is guided through the vocal folds and out through the mouth. When the ProTrach DualCare is in speaking mode, there is no heat and moisture exchanger effect.
Conclusion
Choosing between varieties of tracheostomy tubes, speaking valves, and heat and moisture exchange devices is often difficult, although the decision will be guided by individual requirements. The child's progress and safety will depend on careful follow up and interaction between the child, parents, and a multidisciplinary team, including speech and language therapists and a tracheostomy nurse specialist.
Competing interests
None declared