Introduction
Sensorineural hearing loss is commonly encountered in patients with uncomplicated chronic otitis media. Even though the patients have no history of labyrinthitis, the bone conduction threshold is elevated. However, the mechanism of bone conduction threshold elevation in cases of chronic otitis media is not completely understood. Such an elevation has been reported to be caused by either cochlear involvement, as a result of an extension of inflammation into the inner ear,Reference Cureoglu, Schachern, Paparella and Lindgren1, Reference Paparella, Morizono, Le, Mancini, Sipila and Choo2 or disruption of the middle-ear conductive mechanism of hearing.Reference Walby, Barrera and Schuknecht3 According to Paparella et al.,Reference Paparella, Morizono, Le, Mancini, Sipila and Choo2 sensorineural hearing loss in chronic otitis media is the result of toxic substances passing from the middle ear into the inner ear via the round window membrane. Morphological changes in the cochlea have also been demonstrated in patients with chronic otitis media.Reference Cureoglu, Schachern, Paparella and Lindgren1 An elevation in the bone conduction threshold in chronic otitis media is associated with prolonged disease durationReference Cusimano, Cocita and D'Amico4–Reference Redaelli, Zinis, Campovecchi, Parrinello and Antonelli7 and the presence of cholesteatoma,Reference El-Sayed5, Reference Levine, Shelton, Berliner and Sheehy8, Reference Noordzij, Dodson, Ruth, Arts and Lambert9 which supports the view that toxic inflammatory substances could be the main reason for the elevation in bone conduction threshold seen in chronic otitis media.
On the other hand, an elevation in the bone conduction threshold could be caused by a disruption of the middle-ear mechanism of hearing. The bone conduction response is not always induced by sound conduction from the skull directly to the cochlea.Reference Tonndorf10 The ossicular chain is also involved in the bone conduction response.Reference Tsai, Ostroff, Korman and Chen11 The Carhart effect refers to a depression of bone conduction in the presence of a conductive hearing loss, particularly otosclerosis. Chronic middle-ear inflammation usually causes perforation of the tympanic membrane and ossicular chain discontinuity. In addition, middle-ear granulations can restrict the motion of the ossicular chain. Browning and Gatehouse suggested that elevated bone conduction thresholds in chronic otitis media were likely to reflect the Carhart effect rather than damage to the inner ear due to disease.Reference Browning and Gatehouse12 In addition, Walby et al. reported that there was no evidence that chronic otitis media caused the destruction of hair cells or cochlear neurons.Reference Walby, Barrera and Schuknecht3
The aim of this study was to determine the mechanism of bone conduction change in chronic otitis media. Bone conduction threshold can be restored after ossicular reconstructive surgery if the ossicular chain disruption is the main cause of bone conduction threshold elevation. Therefore, this study compared bone conduction thresholds before and after ossicular reconstruction.
Materials and methods
One hundred and six patients with unilateral, chronic otitis media who had undergone tympanomastoidectomy between 1999 and 2003 were reviewed retrospectively. Subjects with a history of labyrinthitis, previous otological surgery, meningitis, head trauma, labyrinthine fistula and ototoxicity that could cause permanent sensorineural hearing loss were excluded. Patients' ages ranged from 10 to 63 years (mean, 40.1 years). The contralateral, unaffected ear was used as the control.
The air conduction and bone conduction thresholds were measured using a clinical audiometer (GSI 61, Grason-Stadler, Milford, NH, USA), which had been calibrated according to International Organization for Standardization (ISO) standards. Bone conduction threshold measurement was performed with appropriate masking of the opposite ear. The differences between the bone conduction thresholds of the diseased and contralateral normal sides were calculated, and these differences were compared according to the presence of cholesteatoma and the disease duration. Audiograms were obtained pre-operatively and six months after surgery in order to compare the level of post-operative hearing.
The role of ossicular continuity in bone conduction response was investigated by dividing the patients into two groups according to surgery type. The first group comprised subjects who had undergone tympanomastoidectomy with ossicular reconstruction (n = 76). The second group comprised subjects who had undergone tympanomastoidectomy without ossicular reconstruction for a staged operation (n = 30). The post-operative air and bone conduction thresholds were measured in both groups. The patients in the first group were subdivided into successful (n = 37) and unsuccessful (n = 39) groups, according to the presence or absence, respectively, of a post-operative air conduction improvement of 15 dB or more at the four-frequency (500, 1000, 2000 and 4000 Hz) average. The post-operative changes in bone conduction threshold for these subgroups were compared.
Statistical analysis
A paired t-test was used to compare the pre-operative bone conduction threshold for the normal and diseased ears, and to compare the pre- and post-operative bone conduction thresholds in each group. Comparisons between the groups were performed using an independent samples t-test. Linear regression was used to analyse the association between the disease duration and the difference in bone conduction. All statistical analyses were performed using the Statistical Package for the Social Sciences version 11.5 software (SPSS, Chicago, Illinois, USA).
Results and analysis
Pre-operative bone conduction threshold
The differences in the bone conduction threshold ranged from 3.3 to 11.6 dB across the frequency range, and were greatest at 2000 Hz (Figure 1).

Fig. 1 Mean differences in pre-operative bone conduction thresholds according to frequency, for normal and diseased ears (n = 106). These differences ranged from 3.3 to 11.6 dB across the frequency range, with a maximum value at 2000 Hz. (*p<0.05)
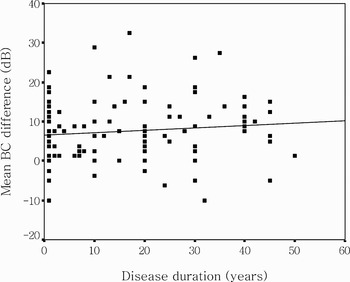
The presence of cholesteatoma and the disease duration did not affect these differences in bone conduction threshold (Table I, Figure 2).

Fig. 2 Correlation between mean pre-operative bone conduction (BC) threshold difference and disease duration. No significant correlation was demonstrated (p = 0.266).
Table I Pre-operative bone conduction threshold differences, by presence of cholesteatoma

* n = 52; †n = 54; ‡p = 0.890. BC = bone conduction; SD = standard deviation
Post-operative bone conduction change
In patients who had undergone ossicular reconstruction, the post-operative air–bone gap (ABG) improved by an average of 10.0 ± 10.4 dB. However, in those who had not undergone ossicular reconstruction, the post-operative ABG did not significantly improve (range, −1.46 ± 10.2 dB). After ossicular reconstruction (n = 76), the mean post-operative bone conduction threshold showed a significant improvement at all frequencies, ranging from 2.3 to 3.9 dB, with the greatest improvement being observed at 2000 Hz (Figure 3a). However, in those who had not undergone ossicular reconstruction (n = 30), the mean post-operative bone conduction threshold did not improve (Figure 3b).

Fig. 3 Mean post-operative bone conduction thresholds according to type of surgery. (a) Tympanomastoidectomy plus ossicular reconstruction (n = 76); significant bone conduction threshold improvement at all frequencies (2.3–3.9 dB), greatest at 2000 Hz (*p < 0.05). (b) Tympanomastoidectomy without ossicular reconstruction (n = 30); no significant bone conduction threshold improvement.
Of those who had successfully undergone ossicular reconstruction (i.e. >15 dB improvement in air conduction threshold; n = 37), a significant improvement in post-operative bone conduction threshold was observed at 500, 2000 and 4000 Hz, ranging from 3.1 to 6.0 dB, with the greatest improvement being observed at 2000 Hz (Figure 4a). In the unsuccessful group (n = 39), the mean post-operative bone conduction changes were smaller and significant only at 1000 Hz (Figure 4b). Post-operative bone conduction change at 2000 Hz was significantly greater in the successful group compared with the unsuccessful group (Figure 4c).

Fig. 4 Mean post-operative bone conduction thresholds in patients undergoing ossicular reconstruction, according to success of surgery (i.e. improvement in air pure tone average of >15 dB). (a) Successful group (n = 37); significant bone conduction threshold improvement at 500, 2000 and 4000 Hz (3.1–6.0 dB), greatest at 2000 Hz (*p < 0.05). (b) Unsuccessful group (n = 39); smaller bone conduction changes, significant only at 1000 Hz (*p < 0.05). (c) Mean post-operative bone conduction threshold changes, comparing successful and unsuccessful groups; bone conduction change at 2000 Hz was significantly greater in the successful group (*p < 0.05).
Discussion
In this study, chronic otitis media was observed to elevate the bone conduction threshold significantly at all frequencies (i.e. 500, 1000, 2000 and 4000 Hz). However, disease duration and presence of cholesteatoma were not related to the degree of the bone conduction changes. The bone conduction threshold improved significantly after ossicular reconstruction. In particular, post-operative change of bone conduction threshold was significantly greater in those who showed a hearing gain after the ossicular reconstruction, compared with those who did not. This suggests that disturbances in the middle-ear mechanism as a result of chronic inflammation can increase the bone conduction threshold, an effect which can be reversed by surgery.
The causes of sensorineural hearing loss in chronic otitis media are controversial. In chronic otitis media, an increase in bone conduction threshold has been reported to be caused by either cochlear involvement, as a result of extension of the inflammation into the inner ear,Reference Cureoglu, Schachern, Paparella and Lindgren1, Reference Paparella, Morizono, Le, Mancini, Sipila and Choo2 or disruption of the middle-ear hearing mechanism.Reference Walby, Barrera and Schuknecht3 In order to exclude the involvement of inflammatory toxins in the inner ear, the correlations between bone conduction threshold and disease duration or presence of cholesteatoma were examined. A longer duration of inflammation might produce a greater elevation of bone conduction threshold. Chronic otitis media with cholesteatoma also has a prolonged pathological process,Reference Cureoglu, Schachern, Paparella and Lindgren1, Reference Eisenman and Parisier13 and several inflammatory mediators might be produced that could lead to inner-ear disease during the active process. However, in this study, the observed bone conduction threshold elevation was not associated with disease duration or presence of cholesteatoma, which is consistent with the results of other studies.Reference Noordzij, Dodson, Ruth, Arts and Lambert9, Reference MacAndie and O'Reilly14 These findings suggest that an extension of inflammation into the inner ear is not the main reason for sensorineural hearing loss in chronic otitis media.
The contribution of the middle-ear mechanism to the bone conduction response in patients with chronic otitis media was examined. The bone conduction response employs three different modes: the compressional, inertial and osseotympanic modes. In the compressional mode, skull vibration caused by sound directly causes vibration of the otic capsule. The ossicular chain is not involved in this mode. However, both inertial and osseotympanic motion employ the ossicular chain. The ossicular chain is loosely connected to the skull and otic capsule. Because of inertia in the ossicular chain, skull vibration due to sound causes movement in the ossicular chain. In osseotympanic motion, sound energy is transmitted from the external auditory canal to the tympanic membrane via the vibration of the skull and para-auditory structures (i.e. jaw and soft tissue).Reference Tsai, Ostroff, Korman and Chen11 If the ossicular chain is ankylosed or disrupted, the inertial and osseotympanic motion contributing to the bone conduction response may be hindered. This can cause an increase in the bone conduction threshold.
This effect has been demonstrated by the Carhart notch observed in cases of otosclerosis. Carhart observed a maximal bone conduction threshold elevation at 2000 Hz in patients with stapes ankylosis, a pattern termed the Carhart notch. This effect can also influence patients with chronic otitis media, via mechanical occlusion of the oval window or the round window by granulations, cholesteatoma or exudate, or by ossicular fixation. In our study, in patients with chronic otitis media, bone conduction thresholds were elevated compared with the contralateral, normal ear. The mean bone conduction threshold difference was greatest at 2000 Hz. This result is similar to those of other studiesReference El-Sayed5, Reference Levine, Shelton, Berliner and Sheehy8 which showed that Carhart effects are also effective in chronic otitis media.
Mean bone conduction thresholds were significantly improved in the ossicular reconstruction group. However, in those cases where the ossicular reconstructions were not performed for a staged opertion, the post-operative bone conduction thresholds were similar to the preoperative values. In the ossicular reconstruction group, the mean average post-operative bone conduction threshold change was less than 5 dB (2.3 to 3.9 dB) over the frequencies. However, 23 of 76 patients (30.3 per cent) showed a >5 dB improvement in bone conduction average (500, 1000, 2000 and 4000 Hz), and seven of 76 patients (9.2 per cent) showed a >10 dB improvement (data not shown).
Individual variations in pre-operative bone conduction threshold and post-operative bone conduction change suggest that the severity of middle-ear pathology might influence the ossicular chain mobility and the bone conduction threshold. In addition, patients undergoing successful ossicular reconstruction (i.e. post-operative air conduction improvement >15 dB) showed better bone conduction improvement than those undergoing the same procedure unsuccessfully. In the unsuccessful group, even though ossicular chain continuity was restored, there may have been middle-ear granulation or other factors which limited the ossicular chain mobility and sound conduction mechanism. These persistent middle-ear problems prevented satisfactory hearing gain or bone conduction improvement.
These results appear similar to those reported by Linstrom et al.,Reference Linstrom, Silverman, Rosen and Meiteles15 who reported bone conduction threshold improvements from 4.0 to 9.3 dB across the frequencies in patients undergoing ossicular reconstruction, with the largest mean improvement being observed at 2000 Hz. Tuz et al. reported improved bone conduction thresholds in six of 12 cases following tympanoplasty.Reference Tuz, Dogru, Uygur and Gedikli16
• In patients with chronic otitis media who have no history of labyrinthitis, bone conduction threshold is elevated. However, the mechanism of bone conduction threshold elevation by chronic otitis media is not completely understood
• In this study, no significant relationship was found between an increase in bone conduction threshold and the disease duration or the presence of cholesteatoma. The mean pre-operative bone conduction thresholds were significantly elevated on the diseased side across frequencies with greatest at 2000 Hz. In addition, Mean post-operative bone conduction thresholds were significantly improved at all frequencies in ossicular reconstruction grop, especially in successful group.
• This study suggests that the elevation in bone conduction threshold seen in chronic otitis media is mainly caused by a change in the conductive mechanism of the middle ear
In contrast, Vartiainen and Seppa reported that nine out of 181 cases showed an improvement in bone conduction threshold after surgery, but this change was not clinically significant.Reference Vartiainen and Seppa17 Similarly, El-Sayed noted that post-operative improvement in bone conduction threshold was significant in only nine out of 93 patients.Reference El-Sayed5
Our finding of post-operative improvement in bone conduction threshold in those who had undergone ossicular reconstruction, particularly in the successful group, may also support the hypothesis that an elevated bone conduction threshold in chronic otitis media is caused by a loss of the middle-ear mechanism of hearing.
Conclusion
This study demonstrated statistically significant elevations in bone conduction threshold in patients with chronic otitis media. No significant relationship was found between an increase in the bone conduction threshold and the disease duration or the presence of cholesteatoma. The mean difference in the pre-operative bone conduction between the diseased and normal ears, and the improvement in the post-operative bone conduction, were greatest at 2000 Hz. These results suggest that the elevation in bone conduction threshold observed in chronic otitis media is caused mainly by a change in the conductive mechanism of the middle ear.