Introduction
Background and rationale
The efficacy of endoscopic ear surgery has been validated in an increasing number of studies within the past 10 years.Reference Yawn, Hunter, O'Connell, Wanna, Killeen and Wick1 Endoscopes offer minimally invasive approaches for various procedures, including tympanoplasty, stapedotomy, cochlear implantation and skull base surgery; similar or even better surgical outcomes have been reported with such endoscopic techniques.Reference Yawn, Hunter, O'Connell, Wanna, Killeen and Wick1–Reference Hsu, Kuo and Huang8
Endoscopic ossicular chain reconstruction has recently become a topic of interest as well.Reference Yawn, Hunter, O'Connell, Wanna, Killeen and Wick1,Reference Cox, Page, Trinidade and Dornhoffer7,Reference Wu, Chen, Yang, Lin, Lee and Liu9,Reference Fisher, Youngs, Hussain and Fishman10 Because endoscopes can better visualise the middle-ear structures,Reference Bennett, Zhang, Labadie and Noble11 it can be hypothesised that endoscopic ear surgery may improve the post-operative outcomes of patients with conductive hearing loss due to ossicular chain disruption.Reference Yawn, Hunter, O'Connell, Wanna, Killeen and Wick1
Objective
This study aimed to compare the outcomes of endoscopic and microscopic ossicular chain reconstruction.
Materials and methods
Study design
This was a retrospective case–control study.
Setting and ethical considerations
After approval by the institutional review board (protocol number: GOA-3552), a retrospective chart review was conducted of patients who underwent ossicular chain reconstruction between January 2012 and June 2017 in the Department of Otorhinolaryngology, Dokuz Eylul University Medical School.
Participants and eligibility criteria
Patients with ossicular chain disruption due to chronic otitis media only were included. Cases with a minimum of two years’ follow up were selected, considering their most recent post-operative audiometric data. Patients with any of the following were excluded from the analyses: age of less than 18 years; cholesteatoma; history of head trauma; revision and/or staged surgical procedures and/or mastoidectomy; surgically confirmed otosclerosis; and congenital aural atresia. Patients who underwent a transcanal approach were not included. Moreover, patients who had undergone surgical procedures that started endoscopically but finished microscopically were also excluded.
Sample size, variables and data sources
A total of 65 patients were included, comprising 31 endoscopic and 34 microscopic ossicular chain reconstructions. All surgical procedures were performed under general anaesthesia by the senior author (EAG) (Figures 1–4) using retroauricular and/or endaural approaches; no special instruments were used for the endoscopic surgical procedures. Microscopic ossicular chain reconstruction was generally performed via a retroauricular incision, in contrast to endoscopic ossicular chain reconstruction which was mostly performed with an endaural incision.

Fig. 1. (a) Peri-operative endoscopic view of the discontinuity between the incus (‘i’) and stapes (‘s’). (b) Touching the malleus (‘m’) to confirm the integrity and mobility after the application of bone cement between the incus and stapes.
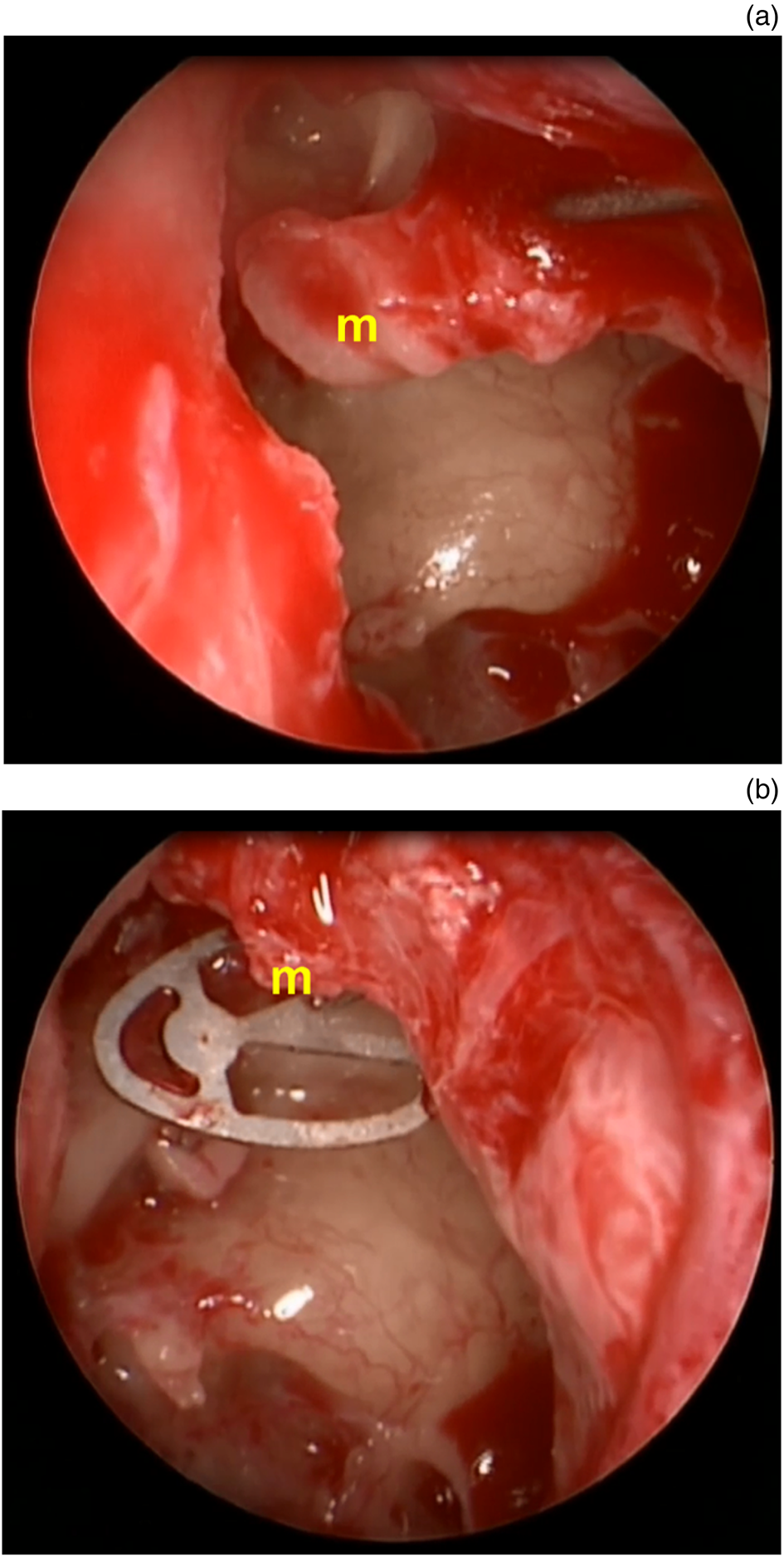
Fig. 2. (a) Peri-operative endoscopic view of the posteriorly relocated malleus (‘m’). (b) Repair using a titanium total ossicular replacement prosthesis (Grace Medical) with a cartilage footplate shoe.

Fig. 3. (a) Peri-operative endoscopic view of the discontinuity between the incus (‘i’) and stapes (‘s’). (b) Bone cement was applied between the incus, stapes and malleus (‘m’).
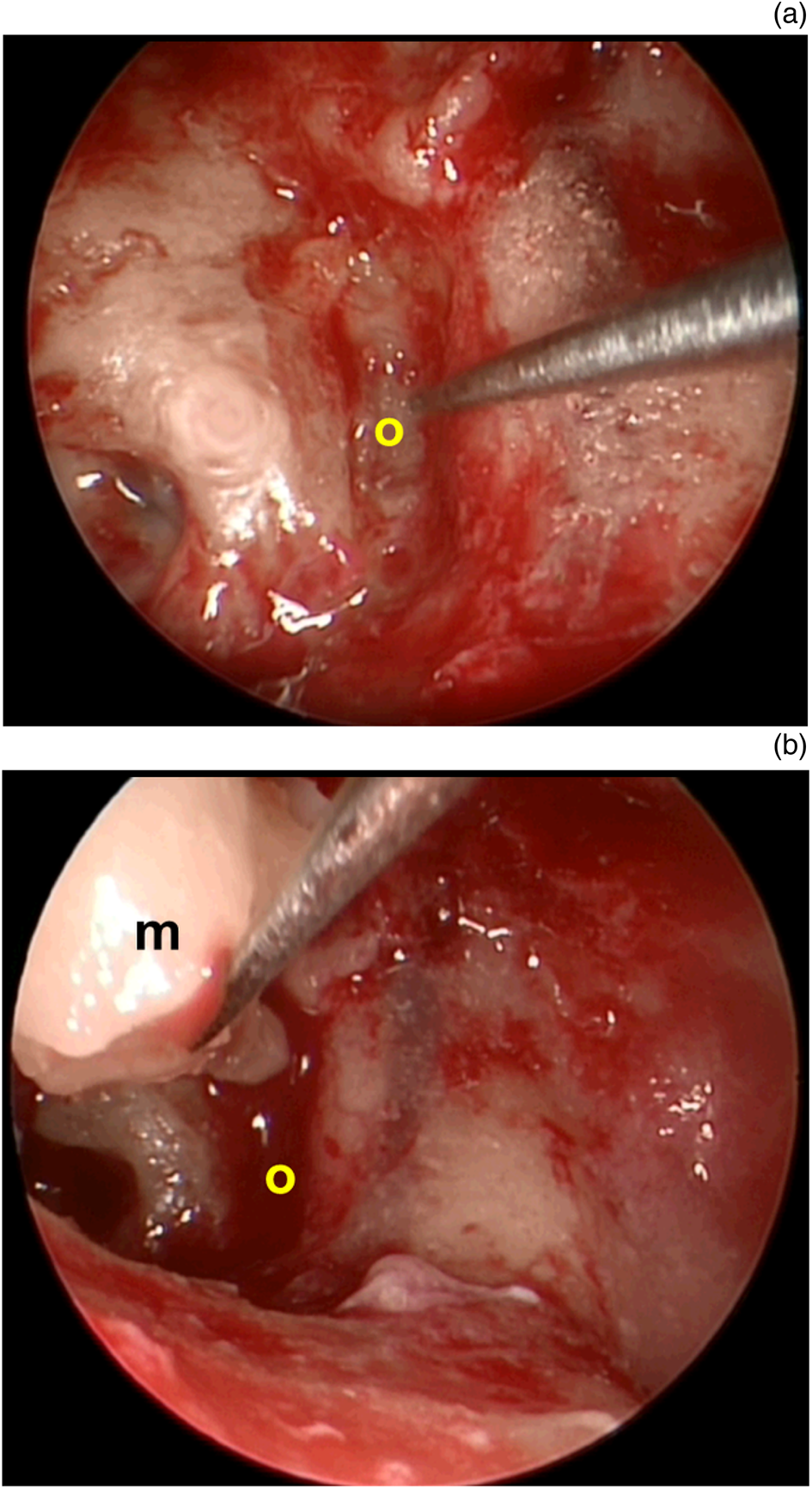
Fig. 4. (a) Peri-operative endoscopic view of the absence of stapes in the oval window (‘o’). (b) Placement of autologous malleus graft (‘m’) onto the oval window.
The study was designed to compare endoscopic and microscopic ossicular chain reconstruction techniques by evaluating variables such as: the age and sex of the patients; otorrhoea status; presence and location of the tympanic membrane perforation; smoking status; presence of middle-ear granulations or effusion; ossicular chain defect type (based on the Austin–Kartush classification);Reference Austin12,Reference Kartush13 presence of the malleus handle and stapes superstructure; Middle Ear Risk Index;Reference Dornhoffer and Gardner14 incision type; tympanic membrane grafting material; ossicular chain reconstruction material (bone cement to repair the discontinuity between the incus and stapes); use of a titanium total ossicular replacement prosthesis (Grace Medical, Memphis, Tennessee, USA) with a cartilage footplate shoe, titanium partial ossicular replacement prosthesis (Grace Medical) or autologous ossicle graft; pre- and post-operative second-year pure tone audiogram resultsReference Gurgel, Jackler, Dobie and Popelka15 (obtained using a Madsen Astera2 audiometer; GN Otometrics, Taastrup, Denmark), including mean air conduction thresholds, air–bone gap, air–bone gap gain and word recognition score; mean operation duration; and mean post-operative follow-up duration.
Bias
To prevent any potential bias, data collection and statistical analysis were cross-checked by a colleague who was not an author of this study and who was blinded to the procedure.
Statistical analysis
Statistical analyses were performed using SPSS software (version 15.0; IBM, Armonk, New York). Results were expressed as numbers and percentages for categorical variables, mean ± standard deviation for parametric variables, and median and range (minimum, maximum) for non-parametric quantitative variables. The assumption of normality was assessed using the Kolmogorov–Smirnov test for the endoscopic and microscopic ossicular chain reconstruction groups. The independent-samples t-test was used to assess the normally distributed quantitative variables, whereas the Mann–Whitney U test was used for non-parametric quantitative variables. Pearson's chi-square and Fisher's exact tests were used to compare the categorical data. Hearing status before and after surgery was compared using the general linear model of repeated-measures analysis of variance to control for within and between subject effects. The ‘within-subject effect’ refers to the difference between pre- and post-operative measurements, whereas the ‘between-subject effect’ represents the difference between the two groups. A p-value of less than 0.05 was considered statistically significant.
Results and analysis
Participants and descriptive data
The two groups were similar in all aspects except for incision type, which was found to be significantly different (Table 1). Both groups were also similar regarding pre-operative air conduction, air–bone gap, air–bone gap gain and word recognition score data (Table 2).
Table 1. Patient characteristics and clinical data

*n = 31; †n = 34. ‡Independent-samples t-test; **Pearson chi-square test; §Fisher's exact test. SD = standard deviation; MERI = Middle Ear Risk Index; TORP = total ossicular replacement prosthesis; PORP = partial ossicular replacement prosthesis
Table 2. Pre-operative air conduction threshold, ABG and WRS, for both groups

*n = 31; †n = 34. ‡Independent-samples t-test. ABG = air–bone gap; WRS = word recognition score; pre-op = pre-operative; SD = standard deviation
Outcome data
Audiological outcome
At the two-year follow-up assessment, post-operative air conduction, air–bone gap and word recognition score had improved significantly in both groups (within-subject p < 0.001 for both air conduction and air–bone gap, and 0.026 for word recognition score, in both groups), and no significant differences were found between them (between-subject p = 0.192 for air conduction, 0.102 for air–bone gap and 0.709 for word recognition score) (Table 3). When the covariates, such as age, sex, Middle Ear Risk Index category, and ossicular chain reconstruction material, were controlled, air conduction and air–bone gap results were also not significantly different (between-subject p > 0.05, and within-subject p < 0.001). There were no differences in follow-up duration or air–bone gap gain between the groups. In addition, the rate of unfavourable hearing outcome, which was considered to be an air–bone gap gain of less than 10 dB, was also similar between the groups (Table 4).
Table 3. General linear model of repeated-measures ANOVA

Controlled for between- and within-subject effects regarding pre- and second-year post-operative air conduction threshold, air–bone gap and word recognition score results. *n = 31; †n = 34. ‡Effect between pre- and post-operative repeated measurements; **effect between endoscopic and microscopic groups. ANOVA = analysis of variance; SD = standard deviation; pre-op = pre-operative; post-op = post-operative; ABG = air–bone gap; WRS = word recognition score
Table 4. ABG gain, ABG closure, and operation and follow-up duration, for both groups

*n = 31; †n = 34. ‡Mann–Whitney U test; **Fisher's exact test; §independent-samples t-test. ABG = air–bone gap; SD = standard deviation
Other analyses
The mean operation duration was significantly shorter for the endoscopic ossicular chain reconstruction group (p < 0.05), and incision type was found to be significantly different between the endoscopic and microscopic groups (p < 0.05) (Tables 1 and 4). The mean operation duration was further examined by considering the type of incision among the endoscopic endaural, microscopic endaural and microscopic retroauricular cases. It was found that the mean duration both for microscopic retroauricular and microscopic endaural surgical procedures was significantly longer than for endoscopic endaural cases (p < 0.05) (Table 5).
Table 5. Operation duration according to incision type

*n = 31; †n = 18; ‡n = 16. **One-way analysis of variance test; §post-hoc Bonferroni test. SD = standard deviation
Discussion
Key results
In this study, air conduction threshold, air–bone gap and word recognition score were significantly improved after surgery in both the endoscopic and microscopic ossicular chain reconstruction groups. The general linear model revealed no differences between the two groups regarding air conduction, air–bone gap and word recognition score outcomes (Table 3). The general linear model was also used to determine the effect of covariates such as age, sex, Middle Ear Risk Index category and ossicular chain reconstruction material on the outcomes; the results showed significant post-operative improvements in both groups, with an insignificant difference between them. The rate of an unfavourable post-operative hearing outcome was also similar between the two groups (Table 4). However, the mean operation duration was significantly shorter in the endoscopic group (Tables 4 and 5).
Interpretation and generalisability
Previous studies have shown similar audiological outcomes after endoscopic and microscopic ossicular chain reconstruction.Reference Kuo and Wu4,Reference Wu, Chen, Yang, Lin, Lee and Liu9,Reference Choi, Noh, Park, Lee, Yook and Choi16–Reference Kaya, Sezgin, Sergin, Ozturk, Eraslan and Gode19 However, the representation of post-operative audiometric data was heterogeneous,Reference Lailach, Zahnert and Neudert20 and some studies have reported only the gain in the air conduction thresholds or closure of the air–bone gap.Reference Zhu, Kou, Lee, Kutz and Isaacson3,Reference Wu, Chen, Yang, Lin, Lee and Liu9 In our study, we used the general linear model of repeated-measures analysis of variance to independently assess the effects of two different ossicular chain reconstruction techniques (Table 3).
A previous study reported that the post-operative hearing outcomes were better in the endoscopic ossicular chain reconstruction group than in the microscopic ossicular chain reconstruction group; however, this result was attributed to the better pre-operative hearing levels of the endoscopic ossicular chain reconstruction cases.Reference Yawn, Hunter, O'Connell, Wanna, Killeen and Wick1 In order to eliminate such confounding factors, we compared the pre-operative hearing characteristics of patients who underwent endoscopic and microscopic ossicular chain reconstruction, and did not find any differences between the groups (Table 2). Because post-operative hearing outcomes after ossicular chain reconstruction may be influenced by the type of the ossicular chain reconstruction material or technique,Reference Govil, Kaffenberger, Shaffer and Chi21 as well as the status of the middle-ear mucosa and Middle Ear Risk Index category,Reference Demir, Karaca, Ozmen, Kasapoglu, Coskun and Basut22 we attempted to exclude the potential effects of these factors on post-operative hearing results by ensuring that the endoscopic and microscopic groups were matched in terms of their peri-operative features (Table 1).
Endoscopic ear surgery provides a greater field of view and ease of access to hidden areas, which may increase the detection rate of the underlying cause of ossicular chain disruption.Reference Kozin, Gulati, Kaplan, Lehmann, Remenschneider and Landegger2,Reference Zhu, Kou, Lee, Kutz and Isaacson3,Reference Huang, Ho, Wang, Chien and Wang18,Reference Tarabichi, Ayache, Nogueira, Al Qahtani and Pothier23 However, the endoscopic technique may be challenging because of the lack of depth perception and inability to use both hands during surgery.Reference Tarabichi, Ayache, Nogueira, Al Qahtani and Pothier23,Reference Marchioni, Mattioli, Alicandri-Ciufelli and Presutti24 In addition, basic principles should be followed to avoid potential thermal risks.Reference Fisher, Youngs, Hussain and Fishman10,Reference Mitchell and Coulson25 A recent study reported that endoscopic ear surgery was associated with better ossicular chain reconstruction outcomes,Reference Yawn, Hunter, O'Connell, Wanna, Killeen and Wick1 but we did not find a similar result in our cohort. However, we think that better visualisation, inherent in the endoscopic technique, may help in performing less invasive surgical procedures with endaural or transcanal approaches instead of retroauricular incisions (Table 1).
• This study compared the results of endoscopic and microscopic ossicular chain reconstruction surgery
• It investigated parameters that could affect post-operative outcomes, including demographic data, middle-ear characteristics and pre-operative audiological status
• Results revealed that the endoscopic and microscopic groups were similar in terms of these parameters
• Statistical analysis of pre- and post-operative hearing status in a single model avoided potential biases
• A minimum follow-up duration of two years contributed to the results’ reliability
• Endoscopic ossicular chain reconstruction surgery may be performed faster and with similar post-operative outcomes to the microscopic technique
A systematic review comparing endoscopic and microscopic tympanoplasty techniques reported similar rates of tympanic membrane closure; however, the duration of surgery and length of hospitalisation were shorter, and cosmetic results were more favourable, in the endoscopic group.Reference Tseng, Lai, Wu, Yuan and Ding26 A recent paper has also shown that the cost-effectiveness of endoscopic and microscopic surgical procedures for chronic otitis media is comparable.Reference Tseng, Lai, Wu, Yuan and Ding27 A smaller incision,Reference Kuo and Wu4 less post-operative pain,Reference Choi, Noh, Park, Lee, Yook and Choi16,Reference Kaya, Sezgin, Sergin, Ozturk, Eraslan and Gode19 reduced medical expenditureReference Kuo and Wu4 and shorter operation durationReference Dundar, Kulduk, Soy, Aslan, Hanci and Muluk17–Reference Kaya, Sezgin, Sergin, Ozturk, Eraslan and Gode19 may be considered as the advantages of all kinds of endoscopic ear surgery.
According to our results, the mean operation duration was significantly shorter in endoscopic ossicular chain reconstruction cases (Table 4), and an endaural incision was more likely to be used (Table 1). The shorter operation duration was probably a result of the reduced need for curettage and/or drilling of the posterior superior wall of the external auditory canal, and the lack of microscope positioning during surgery. However, we believe that an additional issue could have affected the operation duration, because both groups were similar except for the incision type (Table 1). Therefore, we further analysed the type of incision for each case. Post-hoc analyses showed that the operation duration was significantly shorter for endoscopic endaural surgical procedures than for matched microscopic procedures. However, there was no significant difference in the duration of microscopic endaural and microscopic retroauricular surgical procedures (Table 5). We postulate that a shorter operation duration in the endoscopic group may not be solely an effect of the incision type; the heterogeneity of the endoscopic endaural, microscopic endaural and microscopic retroauricular subgroups with regard to the reconstructive materials used may also have had an influence.
In conclusion, we suggest that endoscopic ossicular chain reconstruction may be performed in a significantly shorter time and that it provides post-operative audiometric outcomes that are similar to those of the microscopic technique.
Limitations
The limitations of our study are: the retrospective design and thus the lack of randomisation, the relatively small sample size, and the heterogeneity of the incision types.
Acknowledgements
The authors would like to acknowledge Professor Pembe Keskinoğlu, an esteemed academic member of the Department of Biostatistics and Medical Information, Dokuz Eylul University Medical School, for her professional contribution to the statistical analysis. The authors would also like to thank Enago (www.enago.com) for the English language review.
Competing interests
None declared











