Introduction
Osseous fixation of the malleus and/or incus is an uncommon but significant cause of conductive hearing loss. It occurs when a bony bridge forms between the malleus and/or incus and the walls of the middle ear, preventing proper mobilisation of the ossicles. The bony bridge most commonly fixates in the lateral epitympanic wall,Reference Subotic, Mladina and Risavi1 but other sites include the anterior, superior and lateral malleolar ligaments. Fixation can be congenital, or acquired as a result of infection, trauma or previous middle-ear surgery.Reference Vincent, Lopez and Sperling2 It also commonly occurs concurrently with otosclerosis.
Isolated malleus and/or incus fixation is currently treated surgically by one of two techniques: ossicular chain mobilisation or ossicular chain reconstruction. Ossicular chain mobilisation involves lysing the bony fixations with a drill or laser, but leaving the architecture of the ossicular chain intact. Ossicular chain reconstruction involves removing the malleus head and the incus, and reconstructing the ossicular chain. The earlier method of reconstruction, ‘interposition’ or ‘autograft’, was achieved by reshaping one of the removed ossicles, either the incus or the malleus head, and reinserting it between the manubrium and the capitulum of the stapes. Over time, different synthetic prostheses were developed to reconstruct the ossicular chain.
Both ossicular chain mobilisation and ossicular chain reconstruction are used today, but there is no general consensus as to which technique produces better outcomes. In this study, we examined post-operative audiometric outcomes in patients with isolated malleus and/or incus fixation who underwent either ossicular chain mobilisation or ossicular chain reconstruction, in an attempt to detect a difference between the two techniques. We hypothesised that surgical techniques which preserve the ossicular chain will result in better hearing results because they more closely approximate normal physiological function.
Materials and methods
Search strategy
A systematic search of PubMed, Scopus, and the Cumulative Index to Nursing and Allied Health Literature (‘CINAHL’) was conducted in December 2016 to identify articles studying the surgical treatment of malleus and/or incus fixation. Scopus is a comprehensive database of peer-reviewed literature that includes scientific journals, books and conference proceedings. It draws directly from Medline, Embase and numerous other sources. The Cumulative Index to Nursing and Allied Health Literature is a database of nursing allied health literature. This database, used to supplement our search, was chosen for its unique search interface, subject headings and journal coverage.
The search strategy comprised the keywords: ‘malleus’, ‘malleal’, ‘incus’ or ‘incudal’, and ‘fixation’, ‘ankylosis’ or ‘sclerosis’. Articles were limited to those written in the English language and published in the last 50 years. We re-ran the search for any new articles published through December 2016. The references of our selected studies were also reviewed for any missed titles. The removal of duplicates and storage of articles was accomplished using RefWorks.
The titles and abstracts of articles were screened to identify those presenting surgical outcomes for malleus and/or incus fixation. The full text of relevant articles was reviewed to identify those satisfying the inclusion criteria outlined in Table 1. Two authors (WLC and SP) conducted independent searches; any discrepancies were resolved at each screening stage.
Table 1. Study inclusion criteria

ABG = air–bone gap
Data extraction
We established a list of inclusion and exclusion criteria for the selection of articles (Table 1). All included studies presented clinical hearing outcomes on patients undergoing surgery for isolated malleus and/or incus fixation, presented original data, and included at least five patients. Data were reported in the form of either a mean post-operative air–bone gap (recorded in decibels), or as a percentage of patients with a post-operative air–bone gap of 10 dB or less. Studies were excluded if multiple techniques were used to address malleus fixation, but hearing outcomes were not separated based on a specific surgical technique. Any patients within these studies who did not have a mobile and intact stapes were also excluded from analysis.
Classification of studies
We developed a three-tier classification system, ranking the selected studies by directness of evidence and risk of bias (Table 2). Tier III includes papers that reported outcomes on the surgical management of isolated malleus and/or incus fixation, but only studied one surgical technique or the other. Tier II studies include those that directly compared different techniques for the surgical management of isolated malleus fixation. Tier I studies include those that directly compared different surgical techniques and that also presented individual patient data, allowing for meta-analysis and statistical comparison.
Table 2. Selected studies, arranged according to tier system

In our tier system, we prioritised studies that directly compared the two surgical techniques, over quality and transparency of data. While the latter is valuable because raw data are more amenable to statistical analysis, the former is more in line with the central question of this paper. For instance, Seidman and Babu presented raw data, as in the tier I studies, but only reported on ossicular chain mobilisation; thus, the study is relegated to tier III.Reference Seidman and Babu3
A risk of bias assessment was performed on the selected studies to evaluate them for information bias (Table 3). The categories for this evaluation included: standardisation of treatment, standardisation of outcomes reported and completeness of data. For standardisation of treatment, a ‘good’ rating was given to studies where all patients underwent the same procedure, an ‘OK’ rating indicates that there were different procedures amongst patients but the outcomes were reported separately, and a ‘poor’ rating was reserved for studies with heterogeneous techniques that were not differentiated in the outcomes reported. For standardisation of outcomes, ‘good’ indicates consistent follow-up times, while ‘poor’ indicates inconsistent follow up, and ‘unclear’ reflects no mention of follow-up times in the article. A ‘good’ rating for completeness of data was given to studies where less than 10 per cent of patients were lost to follow up, ‘poor’ was for greater than 10 per cent lost to follow up, and ‘unclear’ indicates that the follow-up data were obscured by other non-contributory data.
Table 3. Assessment of studies

Standardisation of treatment: ‘good’ = all patients within each treatment group underwent the same procedure; ‘OK’ = different procedures but data presented individually; ‘poor’ = variety of treatments given to patients within a treatment group. Standardisation of outcome: ‘good’ = consistent follow-up times; ‘poor’ = inconsistent follow-up times; ‘unclear’ = follow-up times not specified. Completeness of data: ‘good’ = 90 per cent or more original patients completed follow up; ‘unclear’ = follow-up data obscured by other non-contributory data; ‘poor’ = more than 10 per cent of original patients lost to follow up.
Standardisation of treatment was chosen as a parameter to evaluate the consistency of surgical techniques between patients within a study, which could easily represent an influential factor in audiometric outcomes. We looked at the consistency of follow-up times because potential bias exists if outcomes are not recorded at set intervals. Finally, we wanted to highlight any studies that lost large numbers of patients to follow up, as those patients may have had poorer or better outcomes which could have influenced the outcome data.
Studies were considered to have a low risk of bias if they satisfied all three criteria, moderate risk of bias if they satisfied two criteria, and high risk of bias if they satisfied one or fewer.
Data analysis
We extracted and compiled the data from each study in order to compare the ossicular chain mobilisation and ossicular chain reconstruction techniques, and to assess for statistical significance. The primary outcome measures evaluated in this review were: mean post-operative air–bone gap, and the percentage of patients with an air–bone gap of 10 dB or less. The tier I studies presented raw data, reporting the post-operative air–bone gap for each individual patient, so we were able to extract these data and calculate both measures. Most of the tier II and tier III studies, on the other hand, only presented either the mean air–bone gap or the percentage of patients with an air–bone gap of 10 dB or less, and omitted the raw individual data. Thus, we were only able to use the data they published and were unable to calculate the missing measure ourselves. Secondary outcomes included incidence of complications, such as sensorineural hearing loss.
Meta-analysis took place by two complementary but distinct methods. First, pooled rates of surgical success were compared between the ossicular chain mobilisation and ossicular chain reconstruction groups. Surgical success was defined as a post-operative air–bone gap of 10 dB or less. Rates of surgical success using any surgical method were extracted from published reports; these rates could be assessed from all 14 papers where ossicular chain reconstruction, ossicular chain mobilisation or both were used as surgical approaches. Pooled surgical success rates were compared by chi-square test, with significance at p < 0.05. Data analysis was performed using R software (R Foundation, Vienna, Austria).
Next, studies directly comparing ossicular chain mobilisation to ossicular chain reconstruction were considered. This allowed us to use 6 published reports, totalling 147 patients who underwent either ossicular chain mobilisation or ossicular chain reconstruction.Reference Katzke and Plester4–Reference Guilford and Anson9 These include the three tier I papers, and three of the five tier II papers. The other two tier II papers were omitted from this analysis because they did not report outcomes in the form of percentage of air–bone gap outcomes of 10 dB or less.Reference Martin, Oletski and Prades10, Reference Albu, Babighian and Trabalzini11 Again, surgical success was defined as an air–bone gap of 10 dB or less.
Odds ratios using surgical success as a binary outcome were calculated from reported data by logistical regression, as described by Tierney et al.Reference Tierney, Stewart, Ghersi, Burdett and Sydes12 Ossicular chain mobilisation was considered the control group and ossicular chain reconstruction the intervention group for purposes of statistical analysis. Standard error of the mean was calculated from 95 per cent confidence intervals (CIs) by the equation: standard error of the mean = (ln (upper CI limit) – ln (lower CI limit)) / 3.92.Reference Higgins and Green13 Generic inverse variance, fixed effect, hazard ratio forest plots were generated using RevMan 5 software.14 Power calculations for the meta-analysis were conducted as described by Kirkwood and Sterne.Reference Kirkwood and Sterne15 The level of heterogeneity across studies was evaluated using an I2 statistic, with substantial heterogeneity for any I2 value greater than 50 per cent.Reference Higgins and Green16 The presence of publication bias was assessed using funnel plots generated by RevMan software.
Results
Search results
A total of 390 studies were retrieved by the initial search, excluding duplicates (Figure 1). After careful screening, we found that 14 of these studies met the criteria for this review. Searching the references of all included titles did not reveal any further relevant articles. The 14 papers included in the review were published between 1967 and 2015. These 14 studies were then subdivided into 3 tiers based on directness of evidence, and were evaluated for risk of bias.
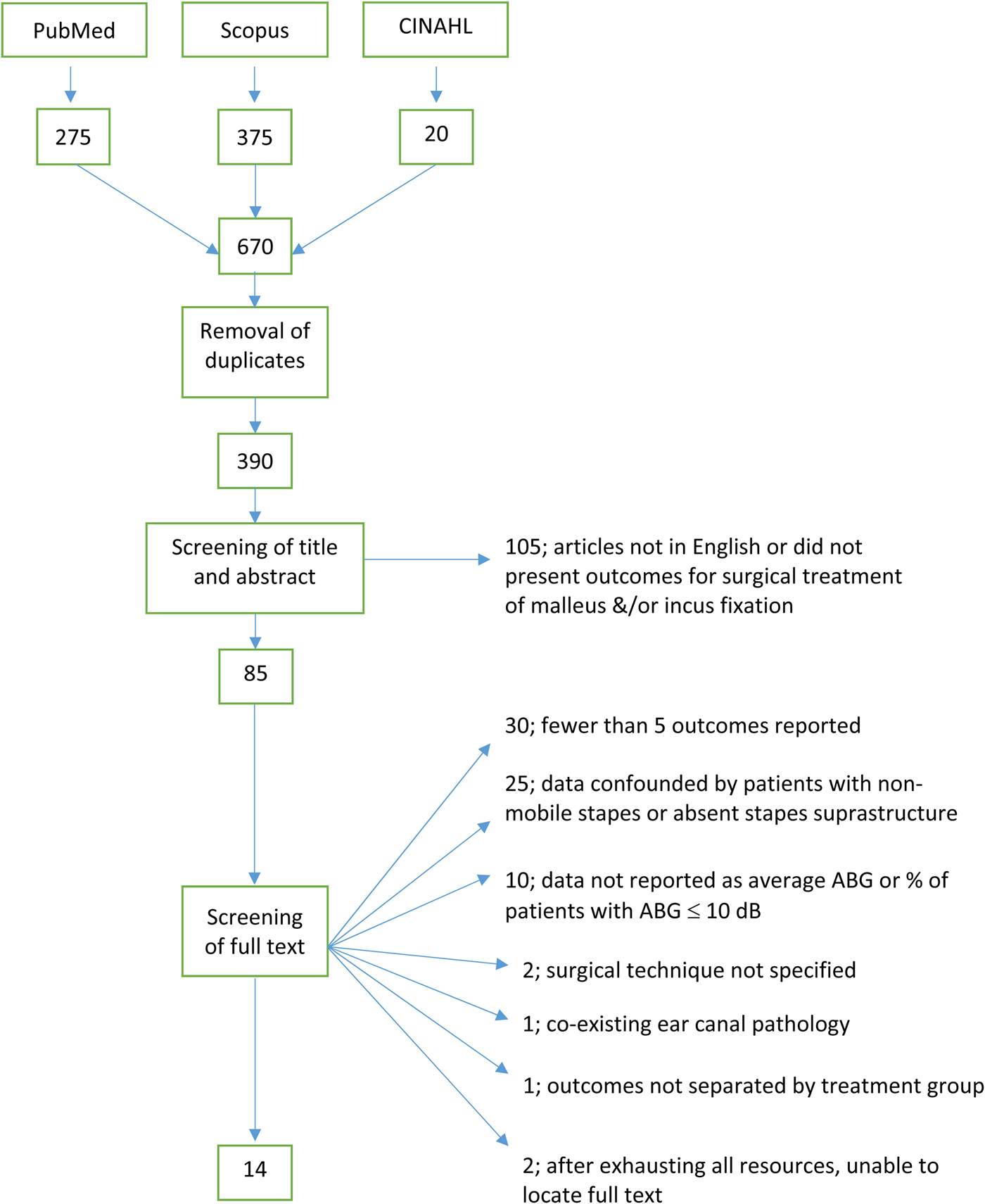
Fig. 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (‘PRISMA’) flowchart of search strategy for study selection. CINAHL = Cumulative Index to Nursing and Allied Health Literature; ABG = air–bone gap
Study assessment findings
Six studies met the criteria for tier III, while five of them met the criteria for tier II; only three studies met the criteria for tier I studies. Amongst the 14 studies, 4 were found to have a low risk of bias, 6 had a moderate risk of bias and 4 had a high risk of bias. Eight studies had ‘good’ standardisation of treatment, while four were rated ‘poor’ and two were rated ‘OK’. Six studies had ‘good’ standardisation of outcomes, while four were ‘unclear’ and four were ‘poor’. Lastly, 11 of the studies had ‘good’ completeness of data, while 2 were ‘poor’ and 1 was ‘unclear’.
Outcome data
The 14 studies included in this review reported clinical outcomes for a total of 391 patients, 165 (42 per cent) of whom underwent ossicular chain mobilisation and 226 (58 per cent) underwent ossicular chain reconstruction.
The outcome data extracted from each study were the average air–bone gap and the percentage of patients with an air–bone gap of 10 dB or less. The standard deviations were also either extracted or calculated from raw data in all studies except for one. The Seidman and Babu study did not report a standard deviation to accompany the average air–bone gap outcomes, and it did not report its raw data, so there was no way for us to extrapolate the standard deviation.Reference Seidman and Babu3
Outcomes for the ossicular chain mobilisation and ossicular chain reconstruction groups are reported in Tables 4 and 5 respectively, and the combined outcomes are summarised by tier in Table 6. Tiers II and III support our hypothesis that preserving the ossicular chain (ossicular chain mobilisation) yields superior results compared to reconstruction, but, interestingly, tier I supports the opposite. Statistical significance was not calculated for these comparisons as they were pooled for meta-analysis.
Table 4. Audiological outcomes for ossicular chain mobilisation

ABG = air–bone gap; NR = not reported
Table 5. Audiological outcomes for ossicular chain reconstruction

ABG = air–bone gap; NR = not reported
Table 6. Combined audiological outcomes based on tier system

*Indicates the approach with the better outcome. OCR = ossicular chain reconstruction; OCM = ossicular chain mobilisation; ABG = air–bone gap; pts = patients
Meta-analysis
Amongst 97 patients undergoing ossicular chain mobilisation for ossicular fixation, the surgical success rate (defined as an air–bone gap of 10 dB or less) was 46.4 per cent. Amongst 197 patients undergoing ossicular chain reconstruction for ossicular fixation, the surgical success rate was 37.6 per cent (Figure 2). On the chi-square test, there was no statistically significant difference between these two groups (p = 0.15).

Fig. 2. Comparison of the post-operative hearing outcomes in the ossicular chain mobilisation (OCM) and ossicular chain reconstruction (OCR) groups (p = 0.15): percentage of patients with post-operative air–bone gaps (ABGs) of 10 dB or less, used here as a marker of surgical success.
A meta-analysis of odds ratios was conducted using data for 147 patients from 6 published studies. Forty-seven patients underwent ossicular chain mobilisation and 100 underwent ossicular chain reconstruction. Using 147 patients, this analysis had a power of 90 per cent to detect an odds ratio of 2.2. An odds ratio of greater than 1.0 would represent a higher likelihood of success in ossicular chain reconstruction patients, and an odds ratio of less than 1.0 would represent a higher likelihood of success in ossicular chain mobilisation patients. A forest plot for the meta-analysis is shown in Figure 3a. The cumulative odds ratio was 0.74 (95 per cent CI = 0.34–1.62, p = 0.45), representing a higher likelihood of surgical success in ossicular chain mobilisation patients; this difference, however, was not statistically significant. This analysis had low heterogeneity, with I2 = 12 per cent, as seen in the funnel plot (Figure 3b).

Fig. 3. (a) Odds ratios comparing the surgical outcomes of ossicular chain mobilisation (OCM) and ossicular chain reconstruction (OCR), as reported by six studies that investigated both surgical methods. (b) Funnel plot demonstrating the heterogeneity of this analysis. SE = standard error; IV = inverse variance; CI = confidence interval; df = degrees of freedom
Discussion
This systematic review and meta-analysis aimed to examine the literature and determine whether there was a significant difference in audiometric outcomes between the two surgical techniques used to treat isolated malleus and/or incus fixation. Our results favour the hypothesis that ossicular chain mobilisation is superior, with the exception of tier I studies (Table 6). However, after statistical comparison, there is no statistically significant difference in outcomes between the two different surgical techniques. Additionally, the strength of the papers directly comparing these two techniques is low; therefore, the overall power of the meta-analysis is low. The comparisons described in Table 6 were not submitted to statistical analysis as they would be unlikely to produce significant results given the small number of patients in each tier, especially in tier I. Therefore, we felt it would be best to pool the surgical results, as was done in the meta-analysis. Any prospective study would be ethical in randomising patients to one of these two groups, but it would need to be a large study conducted across several institutions given that malleus and/or incus fixation is a relatively rare problem.
There are several decades of literature on both types of surgery, but no accepted consensus exists on which is superior. Katzke and Plester, and others in favour of ossicular chain mobilisation, believe that preserving the continuity of the ossicular chain will best approximate normal physiological function and restore hearing.Reference Katzke and Plester4 The traditional ossicular chain mobilisation technique involves using a bone drill or diamond burr to drill away the bony fixations contributing to the conductive hearing loss, and then introducing a physical barrier between the ossicles and the epitympanum, such as Silastic® sheetingReference Seidman and Babu3–Reference Armstrong5, Reference Martin, Oletski and Prades10, Reference Albu, Babighian and Trabalzini11 or a fascia graft,Reference Sakalli, Celikyurt, Guler, Biskin, Tansuker and Erdurak17 to prevent refixation. More recent advances in this technique include the use of lasers for fixation release. Martin et al. used an erbium-doped yttrium aluminium garnet (‘Er:YAG’) laserReference Martin, Oletski and Prades10 in some of their operations. Seidman and Babu used a potassium titanyl phosphate laser for initial fixation release, but still used a burr for atticotomy and creating adequate space around the ossicles.Reference Seidman and Babu3 Three papers comment on the importance of creating 2 mm of space around the previously fixed ossicle in order to adequately prevent refixation.Reference Seidman and Babu3, Reference Katzke and Plester4, Reference Sakalli, Celikyurt, Guler, Biskin, Tansuker and Erdurak17
Ossicular chain reconstruction techniques have seen significant modification over time and are still the subject of research. The earlier techniques of malleus head and incus interposition have largely given way to use of the partial ossicular reconstruction prosthesis (PORP), invented in 1976 by Shea.Reference Shea18 This trend is largely a result of the belief that synthetic prostheses are more stable over time, whereas the living tissue used in autografts is susceptible to remodelling and reabsorption. Both autografts and synthetic prostheses are at risk of displacement. Other concerns with the PORP are high cost and availability.Reference Goldenberg and Emmet19 Most recently, Sennaroglu et al. published a study in 2015 describing the new technique of manubrio-stapedioplasty, which uses glass ionomer bone cement to build a connection between the manubrium and the capitulum of the stapes, after removal of the incus and malleus head.Reference Sennaroglu, Gungor, Atay and Ozer20 Proponents of this technique cite reduced cost and elimination of the risk of prosthesis displacement.
Few studies have reported long-term data with either ossicular chain reconstruction or ossicular chain mobilisation techniques in patients with isolated malleus and/or incus fixation. Armstrong reported on two patients who underwent ossicular chain reconstruction and experienced refixation of the ossicular autograft about one year after surgery.Reference Armstrong5 Martin et al. reported on two separate instances of PORP slippage at three and five years after surgery, respectively.Reference Martin, Oletski and Prades10 Stankovic presented both short- and long-term outcomes of malleus fixation surgery.Reference Stankovic21 The follow-up rate for the short-term outcomes (assessed three to six months after surgery) was 100 per cent, while the hearing improvement preservation rate in the short term (assessed five years after surgery) was 82 per cent.Reference Stankovic21 Studies that collect additional data on the long-term stability of audiometric outcomes with either ossicular chain reconstruction or ossicular chain mobilisation in this population could help determine whether one approach is superior to the other.
Potential complications inherent to middle-ear surgery exist for both ossicular chain reconstruction and ossicular chain mobilisation. Emmett and Shea outlined possible complications specific to the use of a prosthesis for ossicular chain reconstruction, including pressure necrosis of the tympanic membrane from the placement of a prosthesis that is too long.Reference Emmett and Shea22 No papers in this series reported prosthesis extrusion with ossicular chain reconstruction. The use of bone cement, as in manubrio-stapedioplasty, presents potential complications such as aluminium toxicity if the cement contacts the facial nerve or the oval window, although Sennaroglu et al. reported no such complications.Reference Sennaroglu, Gungor, Atay and Ozer20 Regarding ossicular chain mobilisation related complications, Seidman and Babu described one tympanic membrane perforation and one patient with a 20 dB sensorineural hearing loss, presumably from mechanical vibration of the ossicles by the otological drill intra-operatively.Reference Seidman and Babu3 The remaining studies either had no complications or made no comment of complications.
It is unclear as to whether the aetiology of isolated malleus and/or incus fixation has an influence on the preferred repair technique. Most papers in this review did not directly compare outcomes based upon congenital versus acquired causes of fixation. Five studies included only patients with tympanosclerosis.Reference Tos6, Reference Albu, Babighian and Trabalzini11, Reference Sakalli, Celikyurt, Guler, Biskin, Tansuker and Erdurak17, Reference Stankovic21, Reference Emmett and Shea22 The average air–bone gap amongst those studies was 15.84 dB for ossicular chain mobilisation, with 28.9 per cent having an air–bone gap of 10 dB or less, whereas the average air–bone gap for ossicular chain reconstruction was 17.61 dB, with 21.5 per cent having an air–bone gap of 10 dB or less. Outcomes for patients with congenital isolated malleus and/or incus fixation were reported by Teunissen and Cremers; the average air–bone gap was 19.5 dB for ossicular chain mobilisation, with 33 per cent of patients having an air–bone gap of 10 dB or less, while for ossicular chain reconstruction the average air–bone gap was 15.69 dB, with 38.4 per cent having an air–bone gap of 10 dB or less.Reference Teunissen and Cremers7 Martin et al. studied patients with idiopathic malleus and/or incus fixation, and the average air–bone gap was 9.1 dB for ossicular chain mobilisation and 8.2 dB for ossicular chain reconstruction.Reference Martin, Oletski and Prades10 Finally, Harris et al. reported outcomes in patients with a variety of aetiologies, and showed a higher rate of air–bone gap closure of 10 dB or less in patients with idiopathic versus congenital fixation for the ossicular chain reconstruction technique, although the small sample size (n = 8) does not allow for extrapolation to larger patient populations.Reference Harris, Mehta and Nadol8
Other limitations exist that present confounding factors to the data presented in this review. For the most part, patient outcome data were extracted from a diverse set of studies, and many of these studies describe outcomes in only a small number of patients. A couple of exceptions are the studies by StankovicReference Stankovic21 and Katzke and Plester,Reference Katzke and Plester4 which contained a large number of patients (72 and 68, respectively) relative to the other reports, with a resulting disproportionately larger impact on final data analysis.
The overall variety in techniques, both within and between studies, represents another potentially confounding factor in our data. Some studies had very standardised treatment, while others utilised different surgical methods throughout the study. For example, Sakalli et al.Reference Sakalli, Celikyurt, Guler, Biskin, Tansuker and Erdurak17 and StankovicReference Stankovic21 explicitly state that the same experienced surgeon performed all operations with the same technique throughout the study, but most studies did not exhibit the same degree of consistency. Emmett and Shea described three different ossicular chain reconstruction techniques utilised in their patient series, including malleus interposition, incus interposition and, later on, PORP placement.Reference Emmett and Shea22 Incus interposition was the most common ossicular chain reconstruction technique used in our review (10 studies), followed by PORP and malleus autograft (3 each). Regarding PORP placement, there was additional variability in that Guilford and Anson reconstructed one patient's ossicular chain with a polyethylene prosthesisReference Guilford and Anson9 and Harris et al. report the use of a fat wire prosthesis in one of their patients.Reference Harris, Mehta and Nadol8 Finally, manubrio-stapedioplasty was described as yet another method of ossicular chain reconstruction.Reference Sennaroglu, Gungor, Atay and Ozer20
It is difficult to evaluate the efficacy of ossicular chain reconstruction as a whole when the operations were performed so differently and at different times; three of the studies were published before the invention of the PORP.Reference Armstrong5, Reference Tos6, Reference Guilford and Anson9
There are potential confounders within the ossicular chain mobilisation group too. Mobilisation was achieved with bone drills or burrs in the majority of cases, but two of the newer studies utilised laser technology.Reference Seidman and Babu3, Reference Martin, Oletski and Prades10 The material used as a physical barrier to prevent refixation varied as well. Five authors described using Silastic sheeting,Reference Seidman and Babu3–Reference Armstrong5, Reference Martin, Oletski and Prades10, Reference Albu, Babighian and Trabalzini11 while Guilford and Anson used Teflon sheeting,Reference Guilford and Anson9 Sakalli et al. used a temporalis fascia graft,Reference Sakalli, Celikyurt, Guler, Biskin, Tansuker and Erdurak17 and five studies made no mention of a physical barrier at all.Reference Tos6–Reference Harris, Mehta and Nadol8, Reference Emmett and Shea22, Reference Çelik, Felek, Islam, Arslan, Demirci and Haberal Can23
Conclusion
The current literature describes the use both of ossicular chain mobilisation and ossicular chain reconstruction techniques for the surgical management of isolated malleus and/or incus fixation. This systematic review of retrospective studies found no significant differences in audiometric outcomes between the two techniques, but the overall power of this meta-analysis is low. A large prospective randomised controlled trial could help identify whether one of the techniques yields superior long-term hearing results.
Competing interests
None declared











