Introduction
Organised haematoma is a benign, non-neoplastic, haemorrhagic lesion which preferably arises in the maxillary sinus.Reference Suzuki, Inaba, Hiraki, Hashida, Wakasugi and Kadokawa1 Chronic renal failure (CRF) patients are at an increased risk of bleeding due to platelet dysfunction caused by uraemia and the use of anticoagulants during dialysis.Reference Hörl and Feehally2
Herein, we present two cases of organised haematoma of the maxillary sinus in patients with CRF.
This report was approved by the institutional review board of Chonnam National University Hospital.
Case reports
Case one
A 51-year-old woman presented with a history of right nasal obstruction and recurrent epistaxis for several months. She had previously been diagnosed with CRF, and had been receiving haemodialysis routinely three times a week for the previous six years. The patient denied facial trauma, diplopia, blurred vision or facial numbness.
The patient's complete haematology profile and coagulation tests were normal.
On endoscopic examination, the right lateral nasal wall was found to be medially displaced towards the nasal septum, blocking the nasal passage completely.
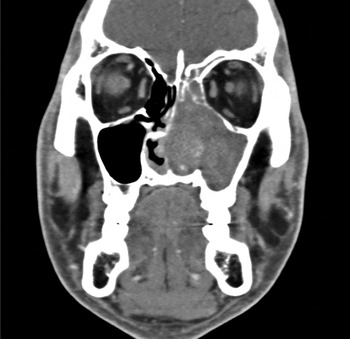
A computed tomography (CT) scan of the paranasal sinuses was performed to evaluate the right nasal cavity. The scan revealed an expansile lesion centred in the right maxillary sinus and elevating the posterior sinus wall, obstructing the right nasal cavity and extending to the ethmoid sinus. A contrast-enhanced scan showed heterogeneous enhancement in the centre of the lesion (Figure 1).
Fig. 1 Axial computed tomography head scan of case one, with contrast enhancement, showing an expansile lesion with heterogeneous enhancement, centred in the right maxillary sinus and elevating the posterior sinus wall, obstructing the right nasal cavity and extending to the ethmoid sinus.
A pre-operative diagnosis of vascular tumour of the right maxillary sinus was made. The patient underwent an angiography, which showed that the internal maxillary artery was the feeding artery. Pre-operative embolisation was performed.
We suspected a vascular tumour, based on the angiography result, and performed a Denker's operation. A dark-reddish, friable lump consisting of blood clots and fibrous tissues was found filling the maxillary sinus. Complete removal of the lesion was accomplished.
The pathological findings were haematoma, fibrosis and neovascularisation, with no evidence of malignancy. This case was diagnosed as an organised haematoma of the maxillary sinus.
The post-operative course was uneventful.
Case two
A 35-year-old man presented with a two-month history of left nasal obstruction and recurrent epistaxis. The patient had hypertension, diabetes and a one-year history of CRF. Since his diagnosis of CRF, he had been receiving haemodialysis. There was no history of facial trauma, bleeding tendency, allergy or sinus surgery.
All laboratory tests were within normal limits.
On endoscopic examination, a large, fleshy, polypoid mass was observed to be completely obstructing the left nasal cavity.
A CT scan of the paranasal sinuses was performed for evaluation of the left nasal cavity. The scan revealed a soft tissue mass filling the left maxillary sinus, with associated expansion of the sinus and partial destruction of the medial wall of the sinus (Figure 2).

Fig. 2 Coronal computed tomography head scan of case two, showing a soft tissue mass filling the left maxillary sinus with associated expansion of the sinus and partial destruction of the medial sinus wall.
Magnetic resonance imaging (MRI) revealed a large, lobulated mass. The central part of the lesion had a low signal intensity on T1-weighted images and a high signal intensity on T2-weighted images (Figure 3).

Fig. 3 Typical findings for a coronal magnetic resonance imaging head scan of case two: (a) T1-weighted image showing a slightly reduced signal intensity in the central region of the lesion (asterisk); and (b) T2-weighted image showing an increased signal intensity in the central region of the lesion (asterisk), with a dark peripheral rim (arrow).
The patient underwent endoscopic sinus surgery under general anaesthesia. The lesion was curetted piecemeal via endoscopy with the assistance of a microdebrider.
Microscopically, the lesions comprised haemorrhage and blood clots coexisting with neovascularisation and fibrosis, with no evidence of neoplasm. The histopathological examination was consistent with an organised haematoma of the maxillary sinus.
The post-operative course was uneventful.
Discussion
Organised haematoma is a non-neoplastic, haemorrhagic lesion which can develop in the paranasal sinuses and nasal cavity.Reference Omura, Watanabe, Fujishiro, Ebihara, Nakao and Asakage3 Because organised haematoma leads to erosion of adjacent structures, it is accepted as a histopathologically benign but clinically malignant lesion.Reference Unlu, Mutlu, Ayhan and Tarhan4
There are various hypotheses regarding the pathogenesis of organised haematoma.Reference Unlu, Mutlu, Ayhan and Tarhan4 These include blood leakage from the nasal cavity into the maxillary sinus, simultaneous submucosal bleeding due to rupture or tear of arterial branches supplying the maxillary sinus, and rupture of unrecognised aneurysms of the arterial branches within the maxillary sinus.
Patients with CRF are at increased risk of bleeding due to platelet dysfunction caused by uraemia and the use of anticoagulants during haemodialysis.Reference Hörl and Feehally2 Therefore, patients with CRF may be at increased risk of developing an organised haematoma.
Typical symptoms of organised haematoma of the maxillary sinus include recurrent epistaxis and nasal obstruction.Reference Lee, Park and Heo5, Reference Song, Jang, Chung and Lee6 Physical examination generally reveals various features similar to those caused by other nasal cavity masses such as nasal polyposis, mucocele, haemangioma, inverted papilloma and malignancy.Reference Song, Jang, Chung and Lee6 Histopathological examination shows haematoma, fibrosis, neovascularisation and no evidence of malignancy.Reference Lee, Park and Heo5 The previously reported clinical presentation, physical examination findings and histopathological examination results are similar to those found in our patients.
• Organised haematoma is a benign, non-neoplastic, haemorrhagic lesion
• It can arise in the maxillary sinus
• Two such lesions in chronic renal failure (CRF) patients are described
• Typical symptoms include unilateral, recurrent epistaxis and nasal obstruction
• Such symptoms in a CRF patient should prompt suspicion of this lesion
Magnetic resonance imaging is the most beneficial radiological examination for the pre-operative diagnosis of organised haematoma. The lesion itself shows intermingled, heterogeneous areas of low, intermediate and high signal intensity, on both T1- and T2-weighted images.Reference Suzuki, Inaba, Hiraki, Hashida, Wakasugi and Kadokawa1 The sinus mucosa surrounding the lesion is well enhanced on T1-weighted images with contrast, and there is high signal intensity on T2-weighted images. The central part of the lesion shows low signal intensity on T1-weighted images and high signal intensity on T2-weighted images, while the peripheral rim of the lesion has low signal intensity on T2-weighted images.Reference Omura, Watanabe, Fujishiro, Ebihara, Nakao and Asakage3 These features differ from those of infectious, inflammatory and neoplastic lesions.
The treatment of choice for organised haematoma is complete surgical evacuation.Reference Lee, Park and Heo5 Regarding the operative approach, as organised haematomas are benign and non-neoplastic, an endoscopic approach is desirable as it is less invasive.Reference Song, Jang, Chung and Lee6, Reference Shen, Som and Teng7 We suggest that pre-operative embolisation is unnecessary.
Conclusion
Organised haematoma of the maxillary sinus is a rare disorder. Endoscopic surgery is the treatment of choice. Magnetic resonance imaging is the best radiological investigation to assist diagnosis. Patients with CRF may be at increased risk of organised haematoma of the maxillary sinus because of their higher risk of haemorrhage. Therefore, when a CRF patient suffers from unilateral, recurrent epistaxis and nasal obstruction, a provisional diagnosis of organised haematoma of the maxillary sinus should be considered.