Introduction
Squamous cell carcinoma is the most common form of laryngeal cancer. Of the three anatomical subsites of the larynx, glottic involvement is by far the most common, accounting for 60–75 per cent of laryngeal cancers. Minimally invasive surgical techniques, such as transoral laser microsurgery, have allowed glottic cancers to be treated with primary surgery.Reference Jones, De, Foran, Harrington and Mortimore1
Several studies have previously demonstrated the effectiveness of transoral laser microsurgery for the treatment of early glottic cancer, showing locoregional control rates of 70–94 per cent, with the disease-specific survival rate nearing 100 per cent.Reference Sjögren2 Despite these good overall outcomes, treatment of recurrence is sometimes necessary. Traditionally, salvage treatment has consisted of either radiotherapy or total laryngectomy.Reference Horwich, Rigby, MacKay, Melong, Williams and Bullock3
The functional implications of total laryngectomy are of significant concern. Radiotherapy typically can only be utilised for a single curative intent treatment course and has its own associated toxicities. Therefore, repeat transoral laser microsurgery may be an enticing avenue for salvage treatment of recurrent glottic cancer.
One study examined the oncological outcomes and utility of repeat transoral laser microsurgery specifically. Roedel and colleagues demonstrated favourable disease-specific survival in patients with early-stage recurrence.Reference Roedel, Matthias, Wolff and Christiansen4 No studies have detailed the functional voice outcomes of repeat transoral laser microsurgery aside from a brief mention.Reference Fink, Sibley, Kunduk, Schexnaildre, Kakade and Sutton5
As the data remain sparse, we sought to provide additional evidence for the oncological safety of repeat transoral laser microsurgery. Additionally, we present the first study to specifically examine the functional outcomes of repeat transoral laser microsurgery for early glottic cancer recurrences.
Materials and methods
Study design, demographics and diagnosis
A retrospective chart review of prospectively collected data for all patients undergoing repeat transoral laser microsurgery resection of glottic cancer at our institution was conducted. All patients undergoing repeat transoral laser microsurgery surgery between January 2003 and July 2018 were included. Patients were excluded if the initial transoral laser microsurgery procedure represented salvage surgery, or if they had previously received radiation treatment. Where indicated, patients were excluded when information was lacking from the chart review. The study was performed under the Nova Scotia Health Authority Research Ethics Board.
Patients were staged according to the appropriate American Joint Committee on Cancer edition at the time of diagnosis, including the sixth, seventh and eighth editions. There is notably no change in glottic cancer staging between these editions.
Beyond the first recurrence, any new carcinoma or carcinoma in situ event in the glottis was considered to be a recurrence. All procedures considered to be repeat transoral laser microsurgery were performed because of clinical or radiological suspicion of recurrence, or frankly overt recurrence.
Treatment schematic
For simplicity of comparison, patient groups were created according to the number of interventions required. By virtue of this study, all patients received a second transoral laser microsurgery procedure beyond their first transoral laser microsurgery. Group A consisted of patients that received no additional treatment beyond the second transoral laser microsurgery procedure. Group B received an additional treatment (three procedures) and group C received one further treatment (four procedures). No patients received any further treatment beyond four procedures.
Functional outcomes
Data were prospectively collected in a transoral laser microsurgery database, including Voice Handicap Index-10 questionnaire results. The Voice Handicap Index was originally developed as a 30-item questionnaire, by Jacobson and colleagues, to quantify the psychosocial consequences of voice disorders.Reference Jacobson, Johnson, Grywalski, Silbergleit, Jacobson and Benninger6 Rosen and colleagues then developed an abbreviated, 10-item version of the Voice Handicap Index questionnaire.Reference Rosen, Lee, Osborne, Zullo and Murry7
Mean Voice Handicap Index-10 scores were compared between the pre-operative period of the second transoral laser microsurgery procedure and the one-year post-operative follow-up period (i.e. before a third treatment, if received).
Complications, including tracheostomy and requirement for gastrostomy tube placement, were considered for the first post-operative year following the second transoral laser microsurgery procedure.
Statistical analysis
Statistical analysis was completed using the commercially available software SPSS (version 21; IBM, Chicago, Illinois, USA). Categorical variables were compared using the chi-square test. Both patient survival and recurrence rates were compared using Kaplan–Meier curves, with significance determined by Mantel–Cox log rank test methods. The overall survival rate was calculated, with events being considered any cause of patient death, with patients alive at time of last follow up being censored. Local and locoregional recurrence rates were calculated, with events being considered either local or regional recurrences, and patients with no previous recurrence at time of last follow up, or at time of death, being censored.
Results
Demographics
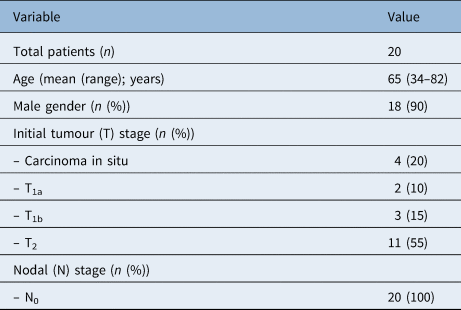
Thirty-four patients were identified and 20 were included in the study. The majority of patients initially had tumour (T) stage T2 disease and no patients had nodal disease on initial presentation (Table 1). Mean follow-up time was 94 months (range, 11–185 months). Mean time between the first and the second transoral laser microsurgery procedure was 35 months (range, 2.6–85 months). The times between each treatment are displayed in Figure 1.

Fig. 1. Times between each treatment. The times to a second transoral laser microsurgery (TLM) procedure (Tx1), and third (Tx2) or fourth (Tx3) treatment are in reference to the first transoral laser microsurgery procedure.
Table 1. Patient demographics and staging
Oncological outcomes
Almost half of the patients (45 per cent) received one repeat transoral laser microsurgery procedure (a second transoral laser microsurgery procedure) and required no further procedures. Eleven of 20 patients (55 per cent) required at least three treatments (Figure 2). The additional treatments included radiotherapy (with or without concurrent chemotherapy), transoral laser microsurgery with adjuvant radiotherapy (with or without concurrent chemotherapy), transoral laser microsurgery alone, or total laryngectomy (Figure 2). There was no association between the presence of positive margins during the first transoral laser microsurgery procedure and the need for additional procedures beyond the second transoral laser microsurgery procedure (relative risk = 0.89, 95 per cent confidence interval = 0.3–2.6). In light of the small sample size, the presence of positive margins for two procedures was not assessed.

Fig. 2. Summary of treatment requirements and outcomes. *Recommended to have total laryngectomy but patient elected for transoral laser microsurgery (TLM). Tx0–3 = first to fourth treatment, respectively; RT = radiotherapy; CC = concurrent chemotherapy; ART = adjuvant radiotherapy; ACC = adjuvant concurrent chemotherapy; TL = total laryngectomy
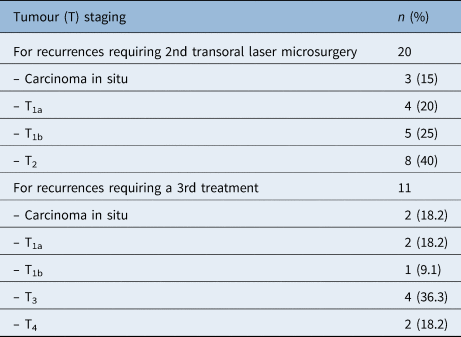
The most common stage of recurrent tumours in patients requiring a second transoral laser microsurgery procedure was T2 (Table 2). In patients requiring an additional treatment (i.e. three procedures), 6 of 11 patients (55 per cent) had stage T3 or T4 disease at the time of the second recurrence (Table 2).
Table 2. Tumour staging of subsequent recurrences
Without stratification into treatment groups, the overall five-year survival rate was 90 per cent (Figure 3). The disease-specific survival rate was 100 per cent. Overall five-year locoregional control in all patients was 64.3 per cent (Figure 4).

Fig. 3. Kaplan–Meier survival curve for all patients, without group stratification (see Materials and methods).

Fig. 4. Kaplan–Meier survival curve of locoregional control rates for all patients, without group stratification (see Materials and methods).
In group A (two transoral laser microsurgery procedures), no patients had recurrence. Both group A and group B (three treatments) contained two patients that died (22.2 per cent of each group), while group C (four treatments) had a 100 per cent survival rate. The five-year survival rate of group A was marginally better than that of group B (88.9 vs 87.5 per cent, Figure 5). The mean follow-up duration, from the time of the most recent treatment, for group A, group B and group C, was 94.4 months (range, 48.9–115.4 months), 39.4 months (range, 0.9–129.7 months) and 44.8 months (range, 4.0–85.6 months), respectively.

Fig. 5. Kaplan–Meier survival curve representing overall survival of patients sub-stratified into groups A (two transoral laser microsurgery procedures), B (three treatments) or C (four treatments) (see Materials and methods).
Functional outcomes
Twelve patients had Voice Handicap Index-10 scores available for analysis (60 per cent). There was improvement in mean Voice Handicap Index-10 scores following the second transoral laser microsurgery procedure, when comparing the pre- and post-operative periods (mean Voice Handicap Index-10 score of 15.5 vs 11.5, p = 0.373). Four patients had initial (pre-first transoral laser microsurgery) pre-operative Voice Handicap Index-10 scores available. The mean Voice Handicap Index-10 score for these patients was 18.75.
Two patients required tracheostomy tube placement for upper airway compromise secondary to glottic scarring following their third treatment. No other major complications occurred. No complications occurred as a direct result of a second transoral laser microsurgery procedure.
Two patients underwent laryngeal sacrifice for salvage treatment, yielding an oncological organ preservation rate of 90 per cent. Both of these were for a third treatment. Another patient required a functional total laryngectomy for a non-functional larynx after a third transoral laser microsurgery procedure and adjuvant chemoradiation, yielding a final organ preservation rate of 85 per cent. However, one group C patient who received a fourth transoral laser microsurgery treatment was advised to have a total laryngectomy, which they refused.
Discussion
Transoral laser microsurgery has evolved rapidly over the past two decades and created a paradigm shift in how laryngeal cancer is treated. Despite excellent outcomes for the treatment of early glottic cancer, recurrences occasionally occur and require further intervention. This study adds evidence to the oncological safety of repeat transoral laser microsurgery, and demonstrates, for the first time, satisfactory functional outcomes.
Unsurprisingly, the majority of patients with initial recurrence had stage T2 tumours in this study. Although the American Joint Committee on Cancer does not sub-stratify T2 into T2a and T2b, recent evidence has pointed toward worse outcomes in patients with T2 disease and impaired vocal fold mobility compared to those with normal movement. Locoregional control has been demonstrated to be significantly reduced in patients labelled as T2b, with lower overall survival.Reference Canis, Martin, Ihler, Wolff, Kron and Matthias8 Furthermore, T2b patients appear to have poorer functional outcomes in terms of patient-perceived voice quality (institutional results, pending publication). The current study was not designed to identify T2a versus T2b patients. In the future, it would be interesting to investigate the relationship between T2 sub-stratification and the outcomes of repeat transoral laser microsurgery, in a larger patient cohort.
By its nature, this study represents a group of patients with difficult-to-control disease, as all those included in this study had a recurrence after their primary surgery. Despite this, the overall survival rate was remarkably high, the five-year locoregional control rate following the second transoral laser microsurgery treatment was reasonable, and the organ preservation rates were excellent. The five-year locoregional control rate amongst all patients in this study was satisfactory given the disease they represent, but is notably worse than the locoregional control rates typically cited for primary transoral laser microsurgery treatment.Reference Day, Sinha, Nussenbaum, Kallogjeri and Haughey9,Reference Warner, Lee and Homer10 Importantly, no patients in group A (two transoral laser microsurgery procedures only) were recommended further treatment but declined. That is, all disease in group A was successfully controlled with a single repeat transoral laser microsurgery procedure.
Voice outcomes were satisfactory despite repeat transoral laser microsurgery procedures, even demonstrating an improvement between the pre- and post-operative periods. The improvement was even more pronounced in those patients with initial Voice Handicap Index-10 scores available from before the first transoral laser microsurgery treatment. While objective voice measurements are possible, the clinical utility should be questioned; the Voice Handicap Index-10 is intended to be a patient-oriented assessment of vocal satisfaction.Reference Batalla, Cueva, González, Pendás, Gil and Llames11
• Despite good locoregional control with transoral laser microsurgery, glottic cancer recurrences do occur
• Typically, radiation or total laryngectomy is required for salvage treatment
• This study highlights the possibility of repeat transoral laser microsurgery for treating recurrent early glottic cancer
• Locoregional control was adequate overall in this patient population with aggressive disease
• Voice and functional outcomes were reasonable with this approach
• Repeat transoral laser microsurgery may be a feasible option for early-stage glottic cancer recurrence
Limitations of this study include its small sample size, limited voice data availability and retrospective nature. Patient numbers were limited by strict inclusion criteria. The limited sample size likely accounts for the T1a recurrence patients having worse survival than T1b and T2 patients together, as it is unlikely that patients with less involved recurrences would have worse outcomes after repeat transoral laser microsurgery. Owing to the rarity of patient death in early glottic cancer, the majority of data points were censored in Kaplan–Meier analysis. Furthermore, no patients died as a result of their disease, giving a disease-specific survival rate of 100 per cent in our study. While voice data were limited, the number of patients with available data does represent the largest group investigated in this setting,Reference Fink, Sibley, Kunduk, Schexnaildre, Kakade and Sutton5 and this is the only study to specifically analyse these patients.
Lastly, this study was not designed to address radiotherapy outcomes compared to transoral laser microsurgery outcomes in recurrence patients initially treated with transoral laser microsurgery. Future investigations are warranted for this as well. Data for this study were collected prospectively as part of an institutional transoral laser microsurgery database, but it is retrospective in its nature. Future multi-institutional randomised trials are likely needed to fully address the use of repeat transoral laser microsurgery with comparison to other salvage modalities.
Conclusion
We have shown that repeat transoral laser microsurgery offers a reasonable chance at locoregional control, and does not appear to adversely affect survival. Additionally, there is improvement of Voice Handicap Index-10 scores with repeat transoral laser microsurgery, and salvage total laryngectomy rates remain low. Repeat transoral laser microsurgery appears to be a safe salvage treatment for early glottic cancer recurrences, with satisfactory functional outcomes.
Competing interests
None declared









