Introduction
Simulation in medical education continues to emerge as a crucial component of residents’ training. Within the field of Otolaryngology, numerous simulations have been described across subspecialties, as various groups have recognised the educational value of hands-on learning for developing surgical skills.Reference Mahalingam, Awad, Tolley and Khemani1 Recent studies have suggested a role for Otolaryngology simulation for medical students as a way to better understand our field.Reference Kovatch, Wertz, Carle, Harvey, Bohm and Thorne2 Simulation in this capacity would provide to those filling training positions Otolaryngology (those filling training positions) an opportunity to enter training with foundational knowledge and technical skills prior to performing interventions on patients.Reference Kovatch, Wertz, Carle, Harvey, Bohm and Thorne2,Reference Sparks, Kavanagh, Vargas and Valdez3
Myringotomy with tube insertion is one of the most common procedures performed by Otolaryngologists. Nearly 670,000 children aged less than 15 years undergo myringotomy with tympanostomy tube insertion every year, which accounts for more than 20 per cent of all ambulatory surgical procedures in this age group.Reference Rosenfeld, Schwartz, Pynnonen, Tunkel, Hussey and Fichera4 Several models for myringotomy and tube insertion simulators are described in the literature.Reference Mahalingam, Awad, Tolley and Khemani1,Reference Sparks, Kavanagh, Vargas and Valdez3,Reference Malekzadeh, Hanna, Wilson, Pehlivanova and Milmoe5,Reference Owa and Farrell6 These models range in complexity and design, with some using virtual reality and three-dimensional printing.Reference Huang, Cheng, Bureau, Agrawal and Ladak7,Reference Wiet, Stredney and Wan8 The goal of any simulation is to present a model that is reproducible, affordable and, most of all, able to replicate the surgical experience in the operating theatre.
We surveyed the pediatric Otolaryngologists in our department on the nuances of the myringotomy procedure that challenge novice surgical trainees. These include microscope positioning, adequate positioning of the speculum within the ear canal, efficient and safe removal of cerumen, determining the presence or absence and type of middle ear effusions, performing a myringotomy in the adequate location, and precise myringotomy tube insertion. With these important aspects in mind, we designed a cost-effective simulation. The model was a modification of that described by Malekzadeh et al. (‘SimTube’), which was recently used in a national simulation study.Reference Malekzadeh, Hanna, Wilson, Pehlivanova and Milmoe5,Reference Wiet, Deutsch, Malekzadeh, Nalekzadeh, Onwuka and Calledner9
Materials and methods
This study was submitted and approved for institutional review board exemption by the Albert Einstein College of Medicine's Office of Human Research Affairs. All testing was performed in the temporal bone laboratory at the Montefiore Medical Center Department of Otolaryngology in Bronx, New York. All participants were Otolaryngology residents at our institution across all post-graduate years. All participants provided informed consent to undergo the simulation test on a volunteer basis.
Model design
Our model was designed using easily accessible materials and was intended for use in a temporal bone laboratory setting. We trimmed 3 ml syringes along the 2.5 ml line to replicate the average length of an ear canal. The cut was angled at 45 degrees to model the anatomical angle of the tympanic membrane (Figure 1). Aluminium foil was carefully casted and rolled to fit the syringe lumen. The degree of ear canal trauma was determined by examining markings on the aluminium foil at the end of the simulation.

Fig. 1. Preparation of ear canal model. With the plunger removed, a 3 ml syringe is cut along the 2.5 ml mark at an angle to replicate the tympanic membrane.
The tympanic membrane was created by adhering two Tegaderm™ (polyurethane polymer) sheets, with the adhesive sides facing each other and a small piece of paper placed between them. A three-digit number was typed onto the paper using a font size of 4 points. The membrane was laid over the end of the ear canal (Figure 2). The time to establish adequate microscope positioning and focus on the eardrum was later measured by asking the participants to correctly identify the number encased in the eardrum (Figure 3).

Fig. 2. Creating the tympanic membrane. (a) A piece of paper with printed text is applied to the adhesive side of a Tegaderm™ sheet using a Rosen pick. (b) The second Tegaderm sheet is placed on top of the other with the small printed text enclosed between them. (c) Both Tegaderm sheets are placed across the end of the previously cut 3 ml syringe.

Fig. 3. Endoscopic view through the ear tube model. This figure demonstrates the view of the tympanic membrane through the model. Air–fluid level is depicted on the image, which would represent middle-ear effusion. Examinees are asked to focus the microscope on the printed (‘257’) text.
The middle ear space was created using mini water balloons. Apple juice and milk were used as serous and purulent effusions, respectively. Using a syringe with an 18-gauge angiocatheter, the fluid was inserted into the balloon to create an effusion in the middle ear space (Figure 4). The addition of the middle ear space and possible effusion added another dimension to the simulation, and allowed participants to suction middle ear fluid should there be an effusion present. A small rolled piece of orange Play-Doh® modelling compound was placed into the canal to simulate cerumen or a foreign body commonly found in the ear canal of a pediatric patient.

Fig. 4. Creating the middle ear space and effusion. (a) The model with a mini water balloon in place to replicate the middle ear. (b) Liquid is introduced into the balloon using a large angiocatheter on a syringe to simulate middle-ear effusion.
The model was secured using a temporal bone holder and was covered with a piece of paper to block the examinee's view of the balloon, leaving only the opening to the canal visible (Figure 5). Examinees were provided with a wax curette, Baron ear tube suctions, alligator forceps, ear speculums, a myringotomy knife and a collar button tympanostomy tube (Figure 5c). Figure 6 demonstrates the typical set up of the simulation from the perspective behind the microscope.
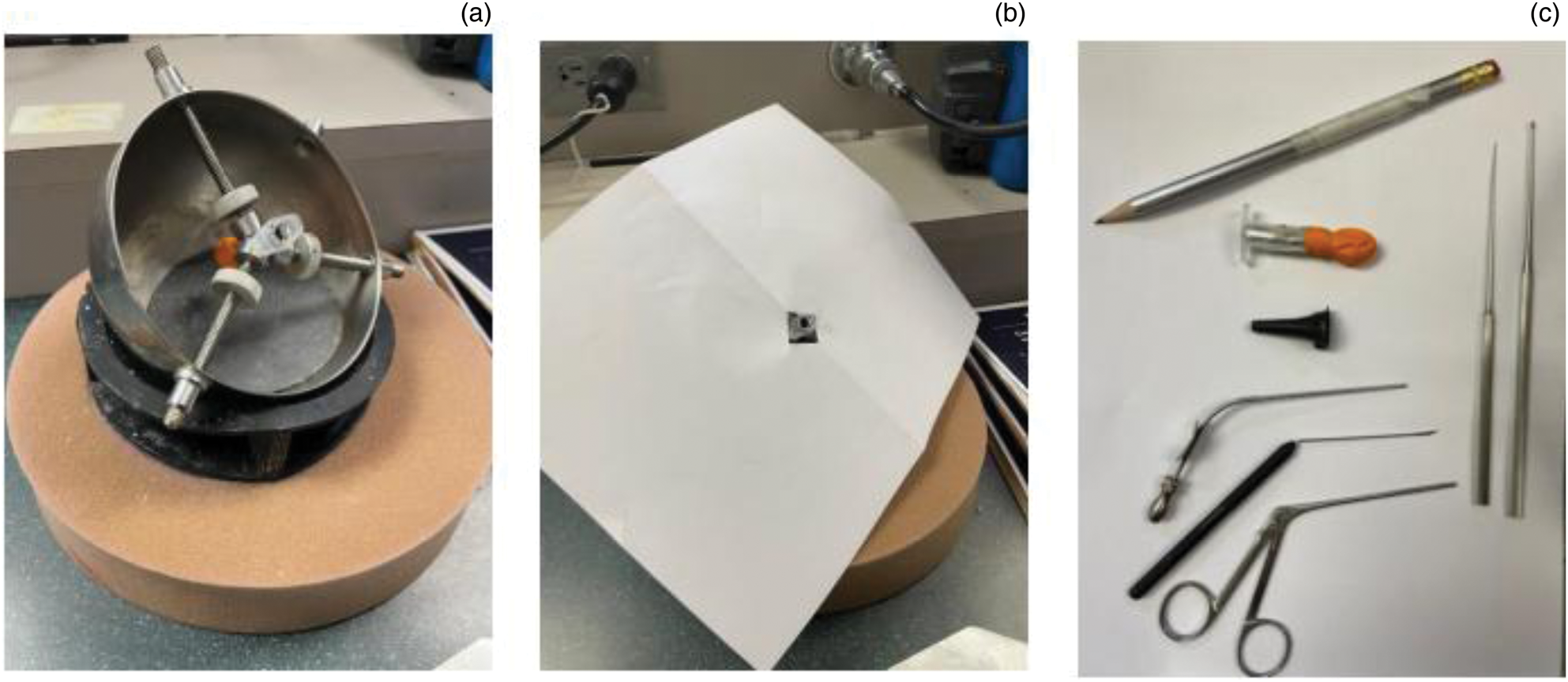
Fig. 5. Setting up the model for use. (a) The model is secured in a standard temporal bone holder. (b) The model is covered with a sheet of paper to block the examinees’ view of the distal portion. This final set up aims to replicate the view a surgeon would encounter in the operating theatre. (c) Standard myringotomy instruments are provided for the examinees. The pencil shown is an example of what can be used to shape the aluminium foil to be inserted into the syringe.

Fig. 6. Use of the microscope. Examinees perform the simulation in our institution's temporal bone laboratory using this microscope set up.
Testing
Participants were evaluated on their performance using a modified version of the Objective Structured Assessment of Technical Skills for surgical trainees by Wiet et al.Reference Wiet, Deutsch, Malekzadeh, Nalekzadeh, Onwuka and Calledner9 We utilized a Delphi technique to develop our modifications and a finalised global grading scale.
Ratings were performed by the authors, which included a board-certified pediatric Otolaryngologist. The graders were trained prior to evaluation of the participants, to enhance inter-grader reliability. Factors for grading included: overall time of procedure, microscope positioning and focus, atraumatic and efficient cerumen removal, identification of the presence and type of middle ear effusion, canal wall trauma, tympanic membrane damage, and tube placement. Individual scores for these categories are outlined on the grading sheet in Figure 7. Time scales were used based on a consensus expert opinion at our institution. For tympanic membrane damage, ‘significant damage’ was determined as that which resulted in the inability to place a tube or would warrant surgical repair in a real-life scenario. Each category had a scoring breakdown ranging from 1 to 5 points, as detailed on the grading form. The maximum possible score was 40.

Fig. 7. Grading rubric. This rubric is used for evaluating participants on different tasks of the model. PGY = post-graduate year; pt = point; s = seconds
Results
Eleven residents from all post-graduate years participated in the simulation. Residents’ post-graduate years and scoring are shown in Table 1.
Table 1. Participant scoring

Table shows the grading for each resident who participated in the simulation along with scored categories. TM = tympanic membrane
Scores ranged from 14 to 34, out of a maximum of 40. The average score among junior and senior residents was 24 and 31, respectively. Though the trend in scoring suggests that more experienced residents performed better on the simulation, statistical analysis of the data was limited by the low number of participants. One resident incorrectly identified the presence and type of effusion. The lowest score category was total simulation time. The simulation was liked by all participants and felt to be representative of the operating theatre experience.
Discussion
Simulation within Otolaryngology is increasingly recognized as an important area for innovation and medical education.Reference Deutsch, Wiet, Seidman, Hussey, Malekzadeh and Fried10 In the wake of the (Covid-19) pandemic, elective cases and opportunities for clinical application have decreased for trainees. With these challenges faced by Otolaryngology residents, the need for simulation models has become more apparent for developing skills that include otomicroscopy, myringotomy and ventilation tube insertion.Reference Shenton and Aucott11–Reference Gallo, Locatello, Orlando, Martelli, Bruno and Cilona13 A recent international survey of Otolaryngologists during the Covid-19 pandemic reported that 90 percent of respondents supported the use of surgical simulation in training. However, many did not have access to these tools at their institutions.Reference Munjal, Kavanagh, Ezzibdeh and Valdez14 Contributing innovative and cost-effective approaches to simulation within Otolaryngology can provide more institutions with the opportunity to utilize training models for developing surgical skills.
Our model represents an easy-to-replicate, low-cost simulation tool that captures several important, nuanced aspects of myringotomy with tube insertion, often overlooked in previously reported ear tube simulation models. This is the first model to our knowledge to create a middle ear space using a water balloon, and able to replicate not only the presence or absence of a middle ear effusion, but also characterise the effusion as serous or purulent. The ability to practise identifying middle ear effusions and suctioning middle ear contents is important for improving otological surgical skills.
Another novel aspect of our model is the ability to objectively examine ear canal trauma using the aluminium foil. Ear canal wall trauma can lead to frustrating bleeding and a more challenging procedure. We found that aluminium foil was an adequate, inexpensive tool to track this. The lowest scores measuring canal wall trauma were seen in the junior resident group, suggesting this tool might be helpful in providing real-time feedback to novice trainees.
For our tympanic membrane, we used double-layered Tegaderm material, which provides a sturdy structure, and may be preferable to cut vinyl or rubber gloves that are often used in other simulation models.Reference Mahalingam, Awad, Tolley and Khemani1 The use of the double sheet further allows the placement of a small piece of paper within the membrane. This enabled us to evaluate residents’ ability to focus and position the microscope.
There are some limitations to this study. Although residents with more surgical experience achieved higher performance scores when using this model, this trend could not be statistically analysed because of the limited number of participants. Additionally, we did not study the ability of the simulation model to improve performance in the operating theatre; this could be explored in future studies. We also see opportunities in expanding the model to make it more challenging and useful for advanced otological techniques. These include modifications to simulate working in stenosed ear canals, performing intratympanic injections and creating tasks to improve endoscopic otological skills.
Conclusion
This study proposes an easy-to-replicate, low-cost simulation model that captures several important, nuanced aspects of myringotomy with tube insertion, often overlooked in previously reported ear tube simulation models.
Data availability statement
All authors have agreed to make any data available should it be requested.
Competing interests
None declared










