Introduction
Head and neck manifestations of Lyme borreliosis are common, occurring in up to 75 per cent of cases.Reference Lesser, Dort and Simmen1, Reference Moscatello, Worden, Nadelman, Wormser and Lucente2 Thus, the otolaryngologist may be called upon to diagnose cases lacking the typical history of erythema migrans or recent tick bite (as occurs in approximately 10–40 per cent of all cases).
Borreliosis is caused by the Borrelia burgdorferi sensu lato species complex, which is further divided into at least 11 different genomic species.Reference Stanek and Strle3 Ticks (Ixodes ricinus species complex) act as vectors for the transmission of Lyme borreliosis from rodents to humans, and borreliosis is currently the most prevalent tick-transmitted illness in the northern hemisphere.
The borrelia spirochete shares structural similarities with Treponema pallidum and, like syphilis, borreliosis may cause systemic illness. However, it is unusual to observe the complete progression of the disease, in which a tick bite leads to a skin lesion, followed by involvement of the cardiovascular and nervous systems, and then arthritis. When diagnosing Lyme borreliosis, one should remember that there is no disease without signs or symptoms, and thus there is no diagnosis in the absence of clinical manifestations.Reference Stanek and Strle3 In everyday medical practice, the only sign that enables a reliable clinical diagnosis is a typical erythema migrans skin lesion (which occurs in 60–90 per cent of patients with symptomatic infection).Reference Mullegger4
Earlobe lymphocytoma, meningoradiculoneuritis (Garin–Bujadoux–Bannwarth syndrome) and acrodermatitis chronica atrophicans are highly indicative of Lyme borreliosis, but even so, serological and/or microbial (i.e. culture or polymerase chain reaction) analysis is needed for accurate diagnosis. Most other signs and symptoms are of low or even no diagnostic value.Reference Stanek and Strle3
Case report
A previously healthy 10-year-old girl was referred by her general practitioner because of an unexplained, slowly progressive, thickened, blue-purple right auricle of several months' duration (Figure 1). After specific questioning, the patient and her mother vaguely remembered an insect bite to the patient's right pinna. They denied any fever, rhinorrhoea, cough, rash, bruising, bleeding or trauma. Upon specific questioning, they also denied any erythema migrans like skin lesions.
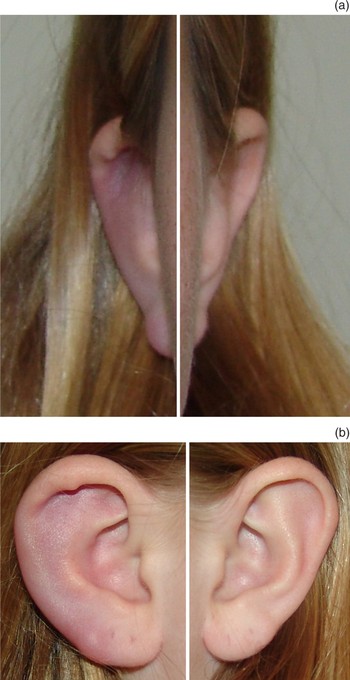
Fig. 1 (a) Anterior and (b) lateral composite views of the patient's right and left ears, 3 days before commencing a 10-day course of oral doxycycline.
Ear microscopy findings and pure tone audiometry were normal. Initial laboratory investigation indicated significantly increased levels of borrelia-specific immunoglobulin (Ig)M and marginally increased levels of IgG antibodies. Testing for borrelia C6 peptide serum antibodies was positive. Liver enzyme tests were normal, and no other laboratory indicators of infection were found (the erythrocyte sedimentation rate was 8 mm/hour, the C-reactive protein level less than 1.0 mg/l and the white blood cell count normal (6.7×109/l; 38 per cent lymphocytes)). Tests for rheumatoid factors, anti-nuclear antibodies (AnA), anti-proteinase and anti-myeloperoxidase were all negative.
With these results (i.e. right-sided earlobe lymphocytoma and positive borrelia serology), the patient was diagnosed with Lyme disease, and was treated with a 10-day oral course of doxycycline 100 mg twice daily (starting three days after the Figure 1 photographs were taken). Under this treatment, the blue discolouration and thickening of the right pinna resolved completely within several weeks (two weeks after the Figure 1 photographs had been taken, there was hardly any observable difference between the right and left auricle left (Figure 2)).
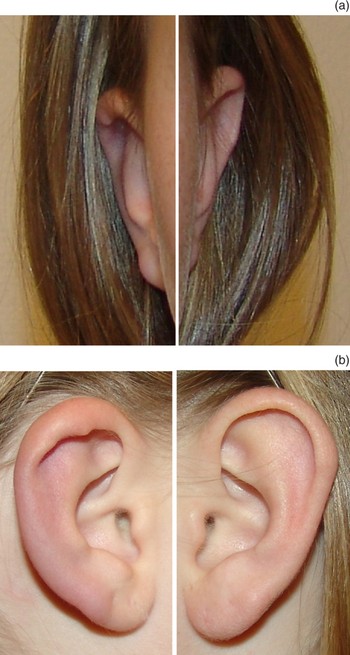
Fig. 2 (a) Anterior and (b) lateral composite views of the patient's right and left ears; photographs taken two weeks after Figure 1.
Discussion
Borrelial lymphocytoma is a solitary, bluish-red swelling or nodule with a diameter of up to a few centimetres, consisting of a dense, B-cell lymphocytic infiltration of the dermis and subcutis. The infiltration is polyclonal with a predominance of B lymphocytes, and often shows germinal centres. The lesion is most frequently located on the earlobe in children, and in the region of the areola mammae in adults. This rare manifestation of Lyme disease arises later and is of a longer duration than erythema migrans, but finally also resolves spontaneously. Borrelial lymphocytoma has been defined as a subacute manifestation of early disseminated Lyme borreliosis, but may sometimes occur at the site of a tick bite (i.e. early localised infection), as was possibly the case in our patient.Reference Asbrink and Hovmark5
A diagnosis of borrelial lymphocytoma can be supported by the presence of (or a history of) erythema migrans, by positive serology (as in our patient) or both. Histological examination is needed in patients with lymphocytoma at a location other than the earlobe.Reference Stanek and Strle3
Borrelial lymphocytoma is the most common type of cutaneous B-cell pseudolymphoma, but is the least common skin manifestation of Lyme borreliosis. The clinical differential diagnosis includes insect bite reactions, primary cutaneous (malignant) lymphoma, foreign body granuloma, sarcoidosis, cutaneous metastasis, keloid, perichondritis and granulomatous contact dermatitis.Reference Mullegger4, Reference Grange, Wechsler, Guillaume, Tortel, Tortel and Audhuy6
Lyme disease is a multisystem illness which primarily affects the skin, nervous system, heart and joints. Within this framework, more or less specific head and neck involvement is seen in the majority of patients.Reference Lesser, Dort and Simmen1, Reference Moscatello, Worden, Nadelman, Wormser and Lucente2
In patients who live in or have travelled through endemic areas, (bilateral) facial nerve palsy (especially in childhood) and (bilateral) sudden hearing loss should prompt the otolaryngologist to consider Lyme disease in the differential diagnosis (although still rare).Reference Quinn, Boucher and Booth7
Neuroborreliosis can arise at any time during the course of Lyme borreliosis. Early neuroborreliosis typically features aseptic meningitis and involvement of the cranial and peripheral nerves.Reference Stanek and Strle3
Recently, Oymar and Tveitnes reported the clinical characteristics of children with neuroborreliosis in an endemic area of Scandinavia (from 1996 to 2006, within a university hospital setting).Reference Oymar and Tveitnes8 A total of 143 children were diagnosed with neuroborreliosis. The most common clinical presentations were symptoms of mild meningitis (75 per cent) and/or facial nerve palsy (69 per cent). All cases were diagnosed between April and December, in keeping with similar studies from other northern European countries, and most were diagnosed between June and October (the peak Lyme disease season), as was our case.
• Lyme borreliosis is the most common tick-borne disease in the northern hemisphere
• The diagnosis can be very difficult because many of the symptoms are similar to those of other disorders
• When confronted with unclear skin lesions and/or other unusual symptoms, especially facial nerve palsy and/or sudden hearing loss, the otolaryngologist should not hesitate to include Lyme disease in the differential diagnosis
Although the causal relationship between Lyme borreliosis and sensorineural hearing loss is difficult to verify, Lyme neuroborreliosis is a rare but potentially treatable cause of sudden deafness and/or vestibular neuronitis.Reference Quinn, Boucher and Booth7 It can be accompanied by musical or other auditory hallucinations.Reference Stricker and Winger9
Conclusion
In view of the likelihood of head and neck manifestations of Lyme disease, the otolaryngologist may be called upon to diagnose cases lacking a history of erythema migrans or recent tick bite.Reference Mullegger4 Lyme disease is a clinical diagnosis, and laboratory tests should only be used to clarify diagnostic issues. Diagnosing Lyme disease can be very difficult because many of its symptoms are similar to those of other disorders. When confronted with unclear skin lesions and/or other unusual symptoms, especially facial nerve palsy and/or sudden hearing loss, the otolaryngologist should not hesitate to include Lyme disease in the differential diagnosis. The presented case serves as a reminder that a non-traumatic, blue-coloured ear lesion should trigger investigation for Lyme disease.




