Introduction
Benign paroxysmal positional vertigo (BPPV) is due to either canalithiasis or cupulolithiasis, and its prevalence increases with age.Reference Oghalai, Manolidis, Barth, Stewart and Jenkins1 Little is known about the homeostasis and turnover, if any, of otoconia, and their fate remains unclear once they have come loose from their underlying support structure in the utricle and macule. The effect of underlying diseases of bone, such as osteoporosis and Paget's disease, on the prevalence of BPPV is unknown. Otosclerosis, which involves abnormal turnover of otic capsule bone, has been shown to be associated with osteoporosis.Reference Clayton, Mikulec, Mikulec, Merchant and McKenna2 Recent investigation has suggested that up to 75 per cent of Swiss women between the ages of 50 and 80 years have osteoporosis or osteopenia and could be at higher risk of BPPV.Reference Vibert, Kompis and Hausler3
Osteoporosis is a major public health problem. The prevalence of osteoporosis is 30 per cent among postmenopausal Caucasian women over the age of 50 years in the United States, based on World Health Organization criteria (i.e. bone density more than 2.5 standard deviations below the mean for young adult women).Reference Melton4 Fracture incidence increases with age, and women have a more than twofold increased incidence of osteoporotic fractures compared with men. Common risk factors for osteoporosis, in addition to age and female gender, include Caucasian ethnicity, family history, sexual hormone deficiency, corticosteroid use, low calcium intake, smoking and alcohol. Historically, osteoporosis has presented clinically with fractures. However, over the last 10 years there has been a dramatic increase in osteoporosis detection by bone densitometry screening.
With increased clinician awareness and improved treatment options, there has been an increase in the diagnosis and treatment of osteoporosis. The current United States Food and Drug Administration approved treatments for osteoporosis include alendronate, risedronate, raloxifene (a selective oestrogen receptor modulator), calcitonin and teriparatide (recombinant human parathyroid hormone). Etidronate, a first generation bisphosphonate, was often used during the 1990s prior to the development of the newer bisphosphonates alendronate and risedronate.
The combination of BPPV and osteoporosis in an individual patient would be expected to increase the morbidity of both diseases; BPPV would make a fall more likely, and osteoporosis would increase the likelihood that a fall would result in fracture. In this study, we performed a retrospective analysis of clinical cases of BPPV and controls, to determine if there was any evidence for an association between BPPV and osteoporosis, which might serve to justify a more systematic, prospective investigation of the relationship between these two common diseases.
Materials and methods
The study was approved by the Saint Louis University institutional review board.
A computerised database was used to identify the medical records of women aged 51 to 80 years diagnosed with BPPV at two different otology clinics, based upon clinical evaluation and videonystagmography testing between 2003 and 2007. These charts were analysed for the presence or absence of osteoporosis. For the purpose of this study, patients were assigned a diagnosis of osteoporosis if they reported taking any of the following medications (on their intake questionnaire during their initial otology clinic visit): alendronate, risedronate, etidronate, raloxifene, calcitonin or teriparatide. Hormone replacement therapy or calcium supplementation alone was not considered indicative of osteoporosis.
The same computerised database was used to identify the records of women with symmetric sensorineural hearing loss and without known vestibular problems, which were then analysed for the presence or absence of osteoporosis based on the criteria above.
Data were divided into decades for subgroup analysis. Since the prevalence of both BPPV and osteoporosis changes with age, subgroup analysis was used to further define the association between these two diseases as a function of age.
Statistical evaluation was performed using two-tailed chi-square analysis, or Fisher's exact test if one of the comparison groups had no patients.
Results
Results are summarised in Table I. In the group as a whole, chi-square analysis showed no significant association between BPPV and osteoporosis, although a trend was observed toward decreased prevalence of osteoporosis in patients with BPPV. Subdivision of results by patient age showed a statistically significant negative association between BPPV and osteoporosis for the 51–60 year age group (Fisher's exact test, p = 0.045). Analysis of women in their 60s showed a trend toward a negative association between BPPV and osteoporosis (chi-square, p = 0.20).
Table I Analysis of women with and without treated osteoporosis and with and without BPPV
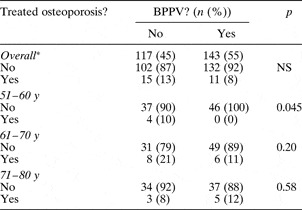
*n = 260. BPPV = benign paroxysmal positional vertigo; NS = not significant; y = years
Discussion
The results of this study suggest a trend towards a negative association between clinical BPPV and treated osteoporosis in women. Analysis reached statistical significance (p = 0.045) for women in their sixth decade, and there was a trend towards a negative association for women in their seventh decade and in the overall analysis. Evaluation of women in their eighth decade showed no association of BPPV and osteoporosis, perhaps due to the known increase in prevalence of both osteoporosis and BPPV with advancing age.
It remains unclear whether the negative association observed between BPPV and treated osteoporosis in this study is due to a negative association between the underlying disease processes of osteoporosis and BPPV, or due to a therapeutic effect on BPPV of the medication used to treat osteoporosis. Since patients were defined as having osteoporosis based on use of medication for osteoporosis treatment, it remains unclear whether untreated osteoporosis is also negatively associated with BPPV. Recently, it has been shown that BPPV refractory to treatment is associated with low bone density in women not currently being treated with osteoporosis medication.Reference Jang and Kang5 The fact that recalcitrant BPPV is associated with untreated low bone density, and that (as shown in the current study) women with treated osteoporosis (i.e. bone density less than T = −2.5) are less likely to have BPPV (Table I), suggests the possibility that anti-osteoporosis medication may be useful in the treatment or prevention of BPPV.
• Benign paroxysmal positional vertigo (BPPV) is due to either canalithiasis or cupulolithiasis, and its prevalence increases with age
• This retrospective analysis of clinical BPPV cases and controls sought to determine whether there was an association between BPPV and osteoporosis
• There was a negative association between BPPV and treated osteoporosis in women aged 51 to 60 years, and a trend towards a negative association for women aged 61–70 years and for the group as a whole
• Osteoporosis, or the medication used to treat it, may provide protection against BPPV
In this study, the prevalence of osteoporosis in women over the age of 50 years (i.e. 13 per cent (15/117) in the control group and 8 per cent (11/143) in the BPPV group) fell well below the known prevalence (30 per cent), probably due (at least in part) to underdiagnosis or undertreatment of osteoporosis by patients' general physicians; the disease is notoriously undertreated. The prevalence found here is also comparable to that reported in a similar retrospective analysis of otosclerosis and osteoporosis.Reference Clayton, Mikulec, Mikulec, Merchant and McKenna2
This study provides impetus for further characterisation of the association between osteoporosis and BPPV. The preventative effect on BPPV (if any) of medications used to treat osteoporosis should be further evaluated.
Acknowledgements
We thank Dana Oliver and Stanton Jones for their assistance with data handling and analysis.



