Introduction
Sinonasal undifferentiated carcinoma is a rare aggressive tumour originating from the Schneiderian epithelium lining the sinonasal tract. Since Frierson et al. identified this tumour type in 1986, fewer than 200 cases have been reported.Reference Frierson, Mills, Fechner, Taxy and Levine 1 Sinonasal undifferentiated carcinoma predominantly affects men in the fifth decade of life.Reference Chen, Daly, El-Sayed, Garcia, Lee and Bucci 2 , Reference Wadsworth, Bumpous, Martin, Nowacki, Jenson and Farghaly 3 Neck nodal involvement can occur in 10 per cent of patients, although rates as high as 28 per cent have been reported.Reference Lin, Sparano, Spalding, Eisbruch, Worden and Heth 4 , Reference Xu, Dziegielewski, McGaw and Seikaly 5 Hematogenous metastasis, although uncommon, is reported to involve the lung, liver, brain and bone. Given their rarity, treatment of such tumours is based on experiences described in case reports and small retrospective series. There is no standard of care for these tumours, although aggressive multimodality approach is considered the best option for long-term disease control and patient survival. Even after aggressive multimodality treatment, outcomes remain dismal: the five-year overall survival rate is reported as 20–60 per cent in various patient series.Reference Lin, Sparano, Spalding, Eisbruch, Worden and Heth 4 , Reference Rosenthal, Barker, El-Naggar, Glisson, Kies and Diaz 6 This report describes the use a multimodality approach for treating 16 sinonasal undifferentiated carcinoma patients.
Materials and methods
Patients
The medical records of sinonasal undifferentiated carcinoma patients treated at the All India Institute of Medical Sciences, New Delhi, from 2004 to 2012 were retrieved from departmental archives, and 16 patients with histopathologically confirmed disease were identified. This retrospective analysis was approved by the institutional review board.
All patients had undergone a detailed evaluation at the Head and Neck Clinic by a multidisciplinary team comprising a head and neck surgeon, a radiation oncologist and a medical oncologist. The assessment included a physical evaluation, laboratory investigations (including a complete blood count and liver and renal function tests), computed tomography (CT) and/or magnetic resonance imaging (MRI) of the head and neck area, and X-ray and/or CT of the thorax. All patients underwent endoscopic biopsy. Patients were considered for surgical resection, if possible, and offered post-operative radiotherapy (RT) if high-risk features were present. Patients with inoperable tumours received definitive RT, and those with a good performance status received additional chemotherapy. Patients not fit enough for definitive treatment were offered palliative RT.
Surgery
All suitable patients underwent surgery. Tumour invasion of the skull base, intracranial extension or orbital apex involvement were the most common reasons for selecting non-surgical treatment options. Patients with involvement of the orbital apex were not considered for orbital exenteration. Elective neck dissection was not performed.
Radiotherapy
Three-dimensional (3D) conformal RT planning was used for all patients undergoing definitive and post-operative RT. A customised head and neck thermoplastic immobilisation cast was used to hold patients in a supine position during RT. Planning CT was performed using a large-bore CT scanner (Philips, Amsterdam, Netherlands) and a 3-mm slice thickness. Planning CT along with clinical and/or endoscopy findings was used to define the gross tumour volume. Radiologists participated in the decision to include or exclude treatment-related changes. The clinical target volume included the whole ipsilateral maxillary sinus, the bilateral ethmoid sinus and the nasal cavity, along with the sphenoid sinus and opposite maxillary sinus if there was clinical suspicion of involvement, and restricted by natural barriers such as bone. Retropharyngeal nodes were included for patients with a node-negative (N0) neck, and ipsilateral levels Ia–V were included for those with a node-positive neck. The clinical target volume was isotropically extended by 5 mm to generate the planning target volume.
Post-operatively, a dose of 60 Gy in 30 fractions over 6 weeks was applied to the planning target volume. In patients with microscopic residual disease (R1 resection) and extra-capsular extension, the dose was escalated to 64 Gy. Patients were treated with a definitive RT dose of 70 Gy if risk levels for all potentially affected organs were within tolerable limits. For palliative RT, a dose from 20 Gy in 5 fractions to 50 Gy in 25 fractions was administered, depending on patient symptoms and general condition.
Chemotherapy
Patients with a Karnofsky performance status of 70 or higher and normal laboratory findings (i.e. blood count, kidney and liver function tests) received platinum-based concurrent chemotherapy at the discretion of the treating physician. Patients given definitive RT also received two cycles of neoadjuvant chemotherapy to reduce the tumour size before RT planning. Patients with residual disease after definitive RT also received adjuvant chemotherapy.
Toxicity assessment and follow up
Acute toxicities during RT were assessed using the acute radiation morbidity scoring scheme of the Radiation Therapy Oncology Group. All patients were assessed weekly during RT; those receiving concurrent chemotherapy also had weekly complete blood count testing. After completing treatment, patients were evaluated at the Head and Neck Cancer Clinic after one month and then every three months for the first two years, and six-monthly in subsequent years. Patients underwent clinical examination at each follow up and CT and/or MRI every four to six months, or earlier if there was clinical suspicion of disease progression.
Results
Patient characteristics
This study included data for 16 sinonasal undifferentiated carcinoma patients treated at the All India Institute of Medical Sciences. Of these, 13 were male (81 per cent) and the median age at diagnosis was 47.5 years (range 8–65 years). The disease epicentre was in the nasal cavity for six patients (38 per cent), the maxilla for five patients (31 per cent) and the ethmoid sinus for three patients (19 per cent). Imaging showed that four patients (25 per cent) had intracranial extension while three (19 per cent) had intra-orbital extension. At presentation, three patients (19 per cent) had sphenoid sinus involvement and one had infratemporal fossa involvement. Epistaxis was the commonest symptom (nine patients; 56 per cent), followed by nasal obstruction (three patients; 19 per cent). Fifteen patients (94 per cent) presented with a tumour–node–metastasis stage T4 primary tumour and one (6 per cent) presented with T3 disease; three (19 per cent) had neck nodal metastasis.
Treatment
Four patients (25 per cent) underwent primary surgery: one underwent endoscopic excision, one underwent craniofacial resection and two underwent total maxillectomy. Of these, R0 resection was achieved in three patients and R1 resection in one (who had undergone total maxillectomy). No patient underwent elective neck node dissection.
A total of 13 patients underwent RT: 2 (12 per cent) received post-operative RT (median dose 67 Gy), 1 (6 per cent) received pre-operative RT (dose 50 Gy), 6 (38 per cent) received definitive RT (median dose 70 Gy, range 54–70 Gy) and 4 (25 per cent) received palliative RT. Nine patients (69 per cent) received 3D conformal RT, two (15 per cent) received intensity-modulated RT and two (15 per cent) received conventional RT. A 3D conformal RT plan for one patient is shown in Figure 1.
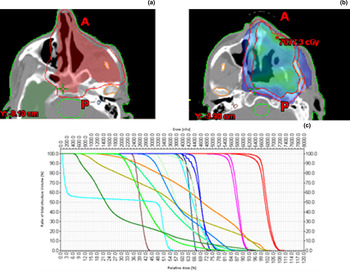
Fig. 1 A computed tomography based three-dimensional conformal plan of post-operative radiotherapy for a sinonasal undifferentiated carcinoma patient, showing (a) target delineation, (b) colour wash and (c) a dose volume histogram. A = anterior; P = posterior
Six patients (38 per cent) received neoadjuvant chemotherapy (two each received paclitaxel plus carboplatin, cisplatin plus etoposide and cisplatin plus 5-fluoro-uracil) before definitive RT or surgery. One patient who received neoadjuvant chemotherapy had severe grade IV neutropenia and empyema thoracis. Four patients (25 per cent) received concurrent chemotherapy with weekly cisplatin (dose 40 mg/mReference Chen, Daly, El-Sayed, Garcia, Lee and Bucci 2 ), which was well tolerated. The median number of concurrent chemotherapy cycles was five (range three to five). Patient characteristics and treatment details are summarised in Table I.
Table I Patient characteristics and treatment details

Total, n = 16. *Unless otherwise indicated. TNM = tumour–node–metastasis; 3D = three-dimensional; 5-FU = 5-fluoro-uracil; RT = radiotherapy
Patient survival
The median follow up was 10.4 months (range 1.0–42.6 months; Table II). The estimated median progression-free survival time was 29.3 months (Kaplan–Meier survival curve shown in Figure 2). The estimated one- and three-year progression-free survival rates were 77 per cent and 41 per cent, respectively. At the last follow up, five patients were alive without disease. The two-year local control rate was 86 per cent. For patients who received curative and palliative therapy, the median survival time was 28.8 months (range 22.6–42.5 months) for those who underwent surgery, 7.2 months (range 2.4–34.1 months) for those who received definitive RT and 3.2 months (range 0.8–21.4 months) for those who received palliative RT.

Fig. 2 Kaplan–Meier survival curve showing progression-free survival of sinonasal undifferentiated carcinoma patients.
Table II Treatment and last follow-up findings for all sinonasal undifferentiated carcinoma patients

Pt = patient; no = number; y = years; RT = radiotherapy; NACT = neoadjuvant chemotherapy; FU = follow up; mon = months; M = male; F = female; PORT = post-operative radiotherapy; pre-op = pre-operative; 5-FU = 5-fluoro-uracil
Failure pattern
Three patients had positive neck nodes at presentation and another developed neck nodal recurrence; thus, the nodal disease risk was 25 per cent in this patient series. One patient had salvage surgery to remove residual primary tumour. At the last follow up, five patients had disease progression. The median time to disease progression was six months. One patient had isolated neck node recurrence, one patient had bone metastasis and three patients had local recurrence. None of these patients was suitable for salvage treatment; all were offered best supportive care only. No patient had long-term grade III or IV radiation-induced toxicity.
Discussion
Consistent with previous reports, the present study found sinonasal undifferentiated carcinoma to be a rare aggressive malignancy that mainly affects older men and presents at an advanced stage: 81 per cent of patients were men with a median age of 47.5 years and T4 disease at presentation.Reference Revenaugh, Seth, Pavlovich, Knott and Batra 8 – Reference Pitman, Costantino and Lassen 10 Orbital involvement, skull base invasion and intracranial extension have been reported in 20–25 per cent of patients.Reference Revenaugh, Seth, Pavlovich, Knott and Batra 8 , Reference Musy, Reibel and Levine 11 In the present series, 25 per cent of patients had intracranial extension, while 19 per cent had intra-orbital extension. Involvement of these critical structures poses a great challenge to achieving complete resection (R0, i.e. no residual disease), and patients often undergo radiochemotherapy. The neck nodal involvement rate of 19 per cent in the present series is consistent with previous reports 10–26 per cent of patients.Reference Lin, Sparano, Spalding, Eisbruch, Worden and Heth 4 , Reference Xu, Dziegielewski, McGaw and Seikaly 5 CT and MRI play pivotal roles in diagnosing sinonasal undifferentiated carcinomas, which appear as expansile lesions with significant bone erosion. Bone erosion is better visualised by CT, whereas MRI is better for visualising intracranial and intra-orbital extension.
Sinonasal undifferentiated carcinoma was previously thought to form part of the spectrum of sinonasal tumours with neuroendocrine differentiation. Hence, the differential diagnosis includes esthesioneuroblastoma, neuroendocrine carcinoma and small cell carcinoma. Morphological analysis of sinonasal undifferentiated carcinoma reveals a tumour composed of small to medium-sized cells. Immunohistochemical analysis reveals that these cells are immunoreactive for cytokeratin and show patchy staining for neuron-specific enolase and epithelial membrane antigen.Reference Wadsworth, Bumpous, Martin, Nowacki, Jenson and Farghaly 3 , Reference Singh, Ranjan, Arava and Singh 12
Surgery is considered the cornerstone of therapy.Reference Reiersen, Pahilan and Devaiah 13 Owing to non-specific symptoms, a third of patients present with extensive local tumours that are unsuitable for surgical resection. If there is cavernous sinus involvement or extension to the orbital apex, brain or infratemporal fossa, tumours are inoperable. In the present series, only 25 per cent of patients had operable tumours. A recent systematic review found surgery to be the single best treatment modality.Reference Reiersen, Pahilan and Devaiah 13 There is a recent trend toward minimal invasive endoscopic resection. Revenaugh et al. highlighted the advantages of minimal invasive endoscopic resection for identifying disease extension and achieving higher gross total resection rates.Reference Revenaugh, Seth, Pavlovich, Knott and Batra 8 In their series, R0 resection was achieved in 53 per cent of patients with T4 tumours who underwent minimal invasive endoscopic resection.
However, Rischin et al. questioned the necessity of surgical resection for sinonasal undifferentiated carcinoma. The two-year overall survival rate of 64 per cent in a cohort of patients treated with induction chemotherapy followed by radiochemotherapy reported by these authors was comparable to the results of different surgical series.Reference Rischin, Porceddu, Peters, Martin, Corry and Weih 14 In the present series, six patients were treated with a similar approach: neoadjuvant chemotherapy followed by definitive RT (with or without concurrent chemotherapy). Neoadjuvant chemotherapy reduced the tumour size, and thus helped in RT planning for these patients.
Radiotherapy is essential for managing sinonasal undifferentiated carcinoma and can be given in a pre-operative, adjuvant, definitive or palliative setting. Musy et al. published their experience of treating sinonasal undifferentiated carcinoma with pre-operative radiochemotherapy comprising pre-operative RT (50–54 Gy) and three cycles of cyclophosphamide, doxorubicin plus vincristine chemotherapy.Reference Musy, Reibel and Levine 11 Surgery was performed within 1 month of radiochemotherapy. The authors reported a two-year overall survival rate of 47 per cent for all evaluable patients. The addition of post-operative RT improves local control as tumour margins are usually close and patients usually present with advanced disease. Tanzler et al. reported 100 per cent local control in patients treated with surgery plus RT compared with only 40 per cent in those treated with RT alone.Reference Tanzler, Morris, Orlando, Werning and Mendenhall 15 Lin et al. reported a median survival time of 39.4 months in their non-surgical cohort and 24.6 months for patients with R0 resection.Reference Lin, Sparano, Spalding, Eisbruch, Worden and Heth 4 In a recent series, Yoshida et al. reported excellent outcomes for patients treated with a tri-modality approach.Reference Yoshida, Aouad, Fragoso, Farwell, Gandour-Edwards and Donald 16 The median overall survival time was 30 months in the tri-modality group compared with 7 or 9 months, respectively, for patients treated with surgery alone or with definitive chemoradiotherapy. Other published series also reported a median survival time of 9–30 months.Reference Rischin, Porceddu, Peters, Martin, Corry and Weih 14 – Reference Christopherson, Werning, Malyapa, Morris and Mendenhall 17 The median survival time of 29.3 months and the three-year progression-free survival rate of 41 per cent in the present cohort are consistent with those of published series. A summary of published data on the characteristics, treatment and outcomes of sinonasal undifferentiated carcinoma patients is given in Table III.
Table III Reported characteristics and treatment outcomes of sinonasal undifferentiated carcinoma patients

*Overall survival, unless otherwise indicated. y = year(s); Pts = patients; LC = local control; RC = regional control; PFS = progression-free survival; Sx = surgery; PORT = post-operative radiotherapy; CT = chemotherapy; RT = radiotherapy; CRT = chemoradiotherapy; NA = not available; NART = neoadjuvant radiotherapy; NACT = neoadjuvant chemotherapy; DMFS = distant metastasis free survival; N + = node positive; pre-op = pre-operative; 3D = three-dimensional; CSS = cause-specific survival; OS = overall survival; ACT = adjuvant chemotherapy; NACRT = neoadjuvant chemoradiotherapy; mon = months; POCRT = post-operative chemoradiotherapy; LRC = locoregional control; DFS = disease-free survival
The best treatment option for neck tumours has long been debated. Although 10–26 per cent of patients present with neck node-positive disease and 60 per cent develop neck node recurrence, many authors do not advocate elective neck node irradiation. However, in a series of 13 patients, Tanzler et al. reported excellent control of neck tumours with elective nodal irradiation (with vs without, 100 per cent vs 66 per cent).Reference Tanzler, Morris, Orlando, Werning and Mendenhall 15 In the present series, three patients had neck node metastasis at presentation and another patient developed neck nodal recurrence, making the overall nodal disease risk 25 per cent. Lin et al. reported a similar nodal disease risk of 26 per cent.Reference Lin, Sparano, Spalding, Eisbruch, Worden and Heth 4 In the present series, five patients received elective nodal irradiation; interestingly, none of these had nodal recurrence. However, one patient treated without elective nodal irradiation had isolated neck nodal recurrence. These findings indicate the importance of considering elective nodal surgery and RT.
Recurrence of sinonasal undifferentiated carcinoma is common, although no definite failure pattern has been documented. Available reports describe local, regional and distant failure, either singly or in different combinations. In the present series, locoregional recurrence was most common. In the present study, the local control rate at two years was 86 per cent, comparable to previous reports.Reference Lin, Sparano, Spalding, Eisbruch, Worden and Heth 4 , Reference Christopherson, Werning, Malyapa, Morris and Mendenhall 17
-
• Sinonasal undifferentiated carcinoma is a rare, aggressive tumour with a dismal five-year overall survival rate
-
• Although a node-positive neck and neck node recurrence are common, elective neck node irradiation is not generally advocated
-
• In this series, 19 per cent of patients had neck nodal metastasis at presentation
-
• The median follow up was 10.4 months (range 1–42.5 months)
-
• The estimated median progression-free survival time was 29.3 months
-
• One- and three-year progression-free survival rates were 77 per cent and 41 per cent, respectively
Limitations of the present study were its retrospective nature and small sample size, although large patient numbers would be difficult in a single institute series. Despite these limitations, the results are encouraging and consistent with Western literature. As recurrence is mainly local, it seems logical to provide post-operative RT to sinonasal undifferentiated carcinoma patients. As 25 per cent of patients have nodal recurrence, the elective nodal treatment should be considered for all patients. A strength of the study is that a multimodality approach proved to be feasible and effective in an unselected patient population outside the context of a clinical trial.
Conclusion
Sinonasal undifferentiated carcinoma generally presents in advanced stage. Surgery should be considered whenever feasible to improve patient survival. Combined post-operative RT and chemotherapy should be used to optimise local and systemic disease control. Patients who undergo definitively RT can receive neoadjuvant chemotherapy to effectively reduce tumour size and help in RT planning. Elective nodal treatment should be considered to improve patient survival because of the high nodal involvement rate.







