Introduction
Dacryocystorhinostomy (DCR) is a surgical procedure that aims to create a window between the proximal part of the lacrimal obstruction and the nasal cavity. DCR can be performed via an endonasal approach (endoscopic) or an external approach by using the projection of the lacrimal sac on nasal wall skin.Reference Ali, Psaltis, Murphy and Wormald1,Reference Ali, Psaltis, Bassiouni and Wormald2 The endoscopic endonasal DCR technique was first described by McDonogh and MeiringReference McDonogh and Meiring3 in 1989. Subsequently, endoscopic DCR was performed more frequently in primary acquired nasolacrimal duct obstruction, and successful results were reported.Reference Onerci4
The success rate of endoscopic DCR is similar to the external technique.Reference Jawaheer, MacEwn and Anijeet5 The most important causes of failure in endoscopic DCR are rhinostomy in an inappropriate anatomic site, creating a small rhinostomy, formation of synechia and granulation tissue.Reference Keren, Abergel, Manor, Rosenblatt, Koenigstein and Leibovitch6 Laser, electrocautery, electrical drill and other cutting instruments have been used for incision of the nasal mucosa and lacrimal sac and for the removal of the bone overlying the lacrimal sac and canal.Reference Leong and MacEwen7 Mucosal flap techniques have been described to reduce the development of synechia and granulation tissue on the exposed bone areas.Reference Ali, Psaltis, Murphy and Wormald1,Reference Khalifa, Ragab and Saafan8 Additionally, silicone stents are applied after surgery to prevent obstruction, and there are inconsistent results regarding stent application.Reference Schulz, Altman and Moher9 In this study, an endoscopic DCR with lacrimal and double nasal mucosal flaps procedure was compared with the endoscopic DCR technique without flap preservation.
Materials and methods
This study was designed as a prospective randomised, controlled trial. The study was conducted on patients who were diagnosed with primary acquired nasolacrimal duct obstruction and accepted surgery. All endoscopic DCR operations were performed by the same surgeon (EC). Data and outcomes were collected between January 2017 and March 2020 at a tertiary university hospital.
Two groups were created based on the surgical technique. The permuted block randomisation method was used for patient selection. Block size was determined as six, and patients were then selected to groups (Figure 1). The eligible patients were accepted to two parallel study groups with similar surgical indications. After the randomisation, patients underwent endoscopic DCR surgery with the lacrimal and double nasal mucosal flaps or endoscopic DCR without flap preservation. The study was conducted according to the Consolidated Standards of Reporting Trials guidelines.Reference Schulz, Altman and Moher9
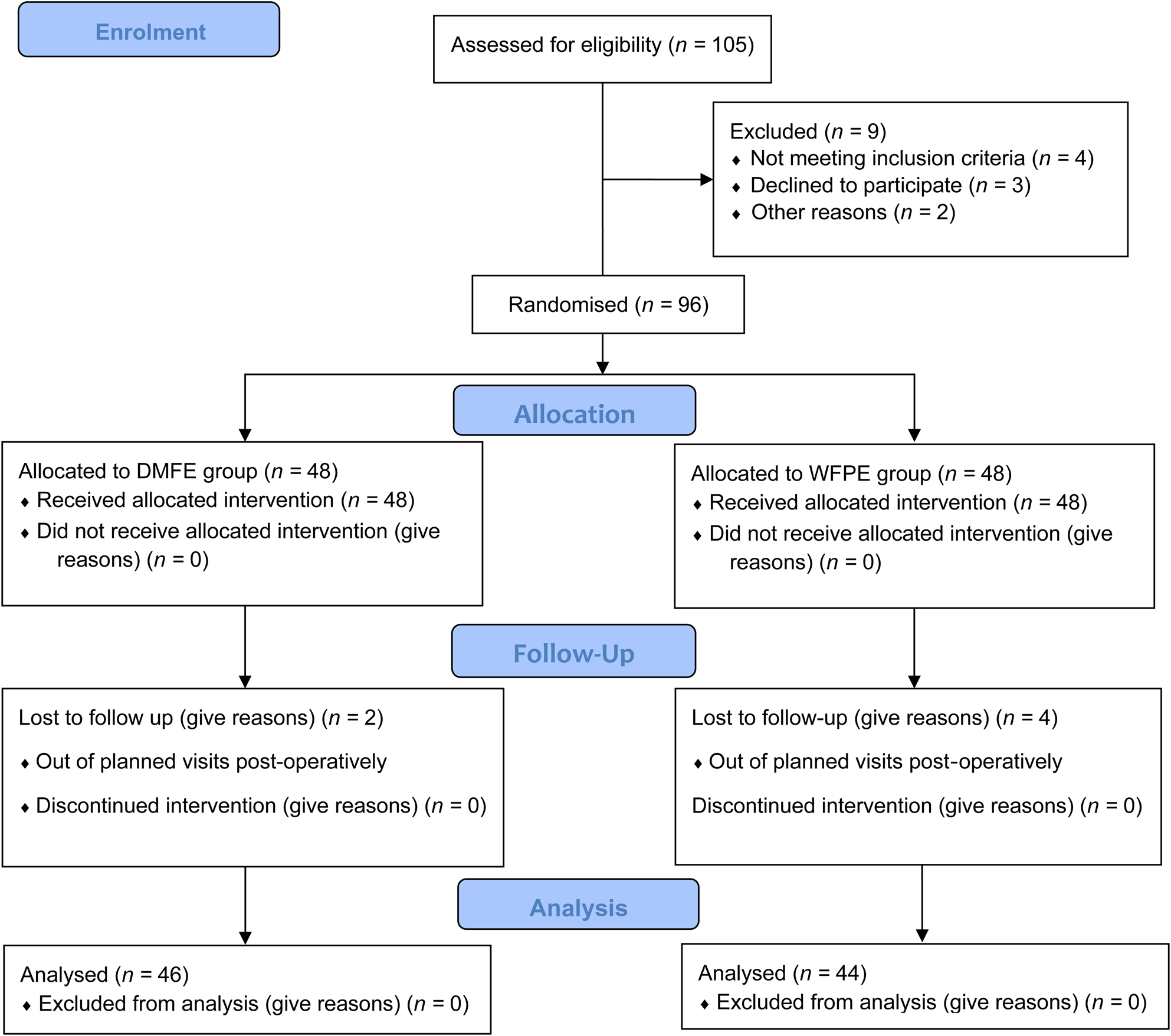
Fig. 1. Flow diagram of study. DMFE = endoscopic dacryocystorhinostomy with lacrimal and double nasal mucosal flaps; WFPE = endoscopic dacryocystorhinostomy without flap preservation
All surgical procedures were performed under general anaesthesia. Endoscopic nasal examination and ophthalmological consultation were performed in all patients pre-operatively. Patients diagnosed with saccal and post-saccal nasolacrimal duct obstruction were included in the study groups. All patients underwent paranasal sinus computed tomography.
Patients with a medical history of previous lacrimal, paranasal sinus or facial surgery, trauma or granulomatous disease were excluded. Patients who had evidence of pre-saccal canalicular obstruction were not included in the study. Paediatric patients (less than 18 years old) were also excluded. No other paranasal surgical procedures were performed during the endoscopic DCR procedures.
All patients had similar medication and post-operative care after the surgery (oral antibiotics: cefuroxime axetil; topical antibiotics: ofloxacin; topical steroid: dexamethasone for seven days with nasal saline irrigation for four weeks). Patients underwent a routine examination at the end of the first and second weeks and the first, second and third month after the surgery (Figure 2). Examination of wound healing, bleeding, crusting and discharge was completed in the first two weeks. Evaluation of granulation tissue formation was carried out at the end of the second month. Assessment of mucosal scar contracture was performed in the third month. Functional success was defined as the free flow of dye into the ostium in the functional endoscopic dye test (a drop of fluorescein 2 per cent), which was performed six months after surgery.
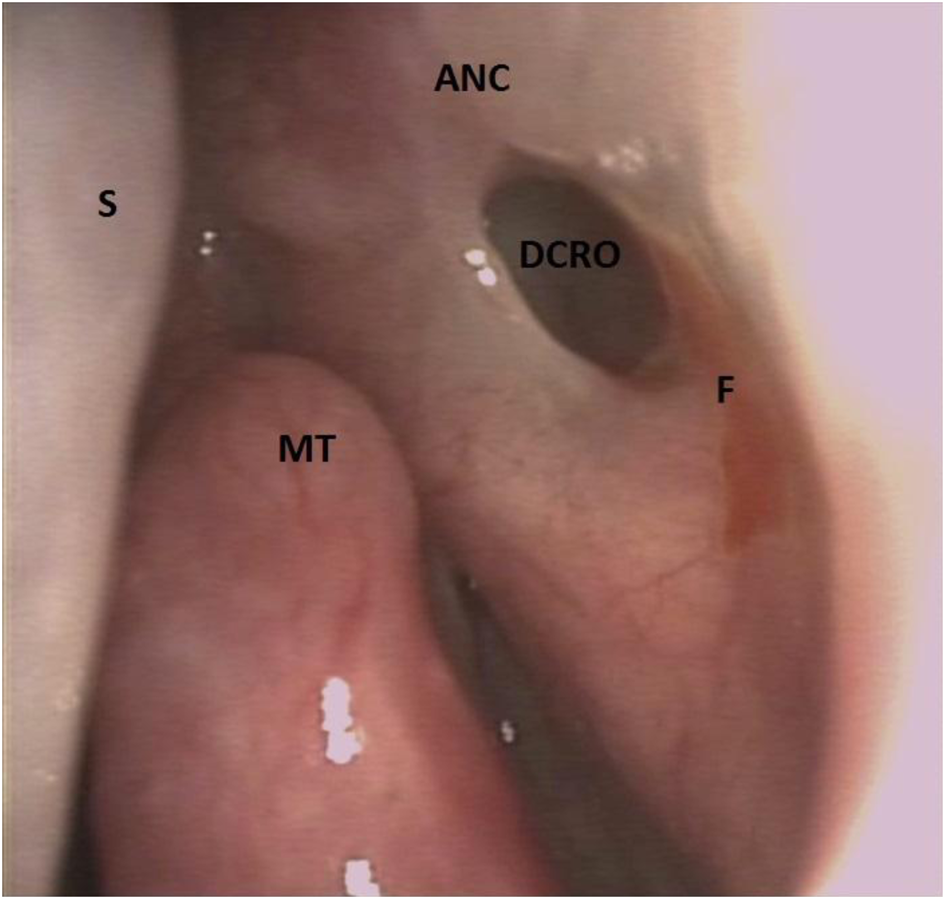
Fig. 2. Left endoscopic view of the rhinostomy opening at the post-operative third month. ANC = agger nasi cell; S = nasal septum; DCRO = dacryocystorhinostomy opening; F = fluorescein remnant; MT = middle turbinate
Lacrimal and double nasal mucosal flaps technique
Pre-operatively, the nasal mucosa was decongested with oxymetazoline intranasal spray. The lateral nasal wall and the head of the middle turbinate were infiltrated with 1 per cent lidocaine hydrochloride with epinephrine bitartrate (1:100 000).
A posterior curvilinear incision was performed along the maxillary line using a sickle knife. A second parallel incision was made 7–9 mm anterior to the first incision, starting 4–5 mm above the axilla of the middle turbinate to the insertion of the inferior turbinate. A 9–11 mm horizontal incision was made across the previous two curvilinear incisions above the insertion of the inferior turbinate. The second 2–4 mm horizontal incision was made at the inferior border of the axilla (Figure 3a). A freer periosteal elevator was used to elevate the mucosal flaps with the periosteum from the underlying bone. An approximately 7–9 × 12–15 mm rectangular-shaped superiorly based mucosal flap was elevated and raised superiorly. Afterwards, a 2–4 × 8–10 mm posteriorly based flap was elevated up to the insertion of the uncinate process (Figure 3b). A 7–9 × 12–15 mm rectangular-shaped mucosal-free window was created with a double mucosal flap. The frontal process of the maxilla and the lacrimal bone were removed with a 2–3 mm cutting burr with an angled hand-piece in reverse mode. The lacrimal duct and the body of the lacrimal sac were exposed. The inferior punctum was dilated, and the lacrimal sac was cannulated with a lacrimal probe. An ‘H-shape’ incision was made over the sac, and two lacrimal flaps were created anteriorly and posteriorly (Figure 3c). The lacrimal canal was irrigated with saline solution to confirm patency. Lacrimal flaps were laid anteriorly and posteriorly. Preserved mucosal flaps were laid over the lacrimal flaps (Figure 3d and Figure 4). Double flaps were supported with 4 × 4 mm gelatine sponge pieces.
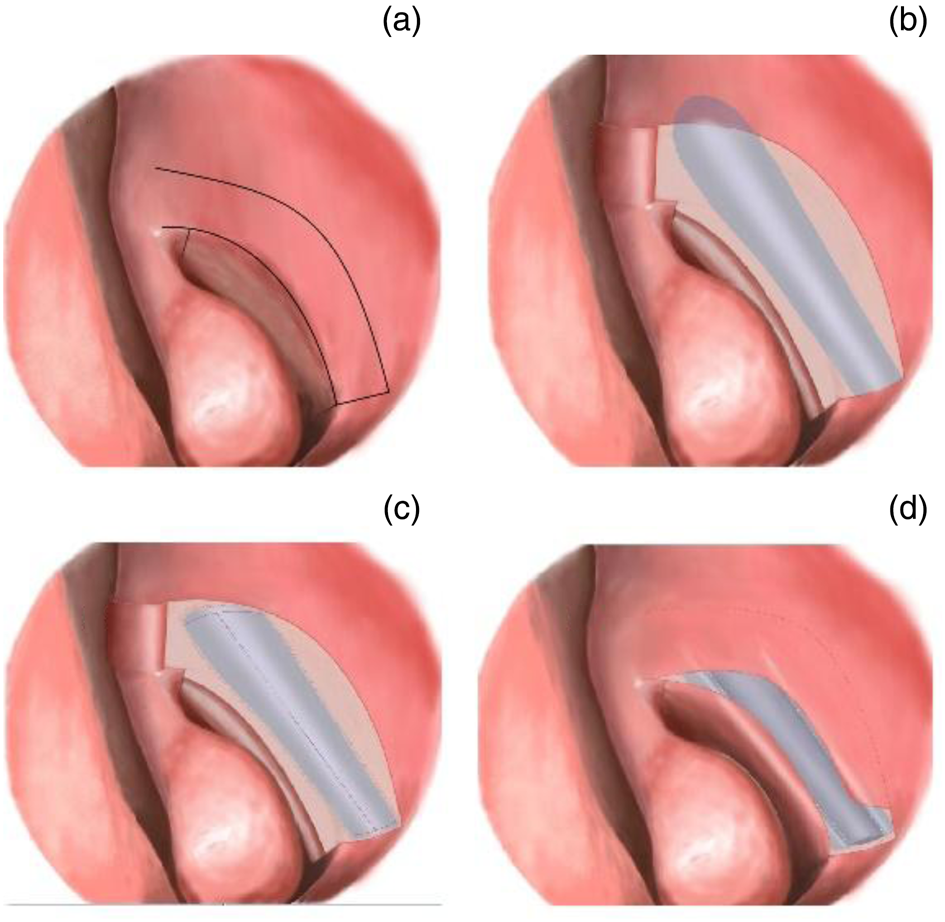
Fig. 3. Double nasal mucosal flaps technique showing: (a) lateral nasal wall with all incisions completed, (b) mucosal flaps elevated and reflected superiorly and posteriorly, (c) the lacrimal duct and the body of the lacrimal sac exposed with an ‘H-shape’ incision made over the sac and (d) mucosal flaps laid over lacrimal flaps
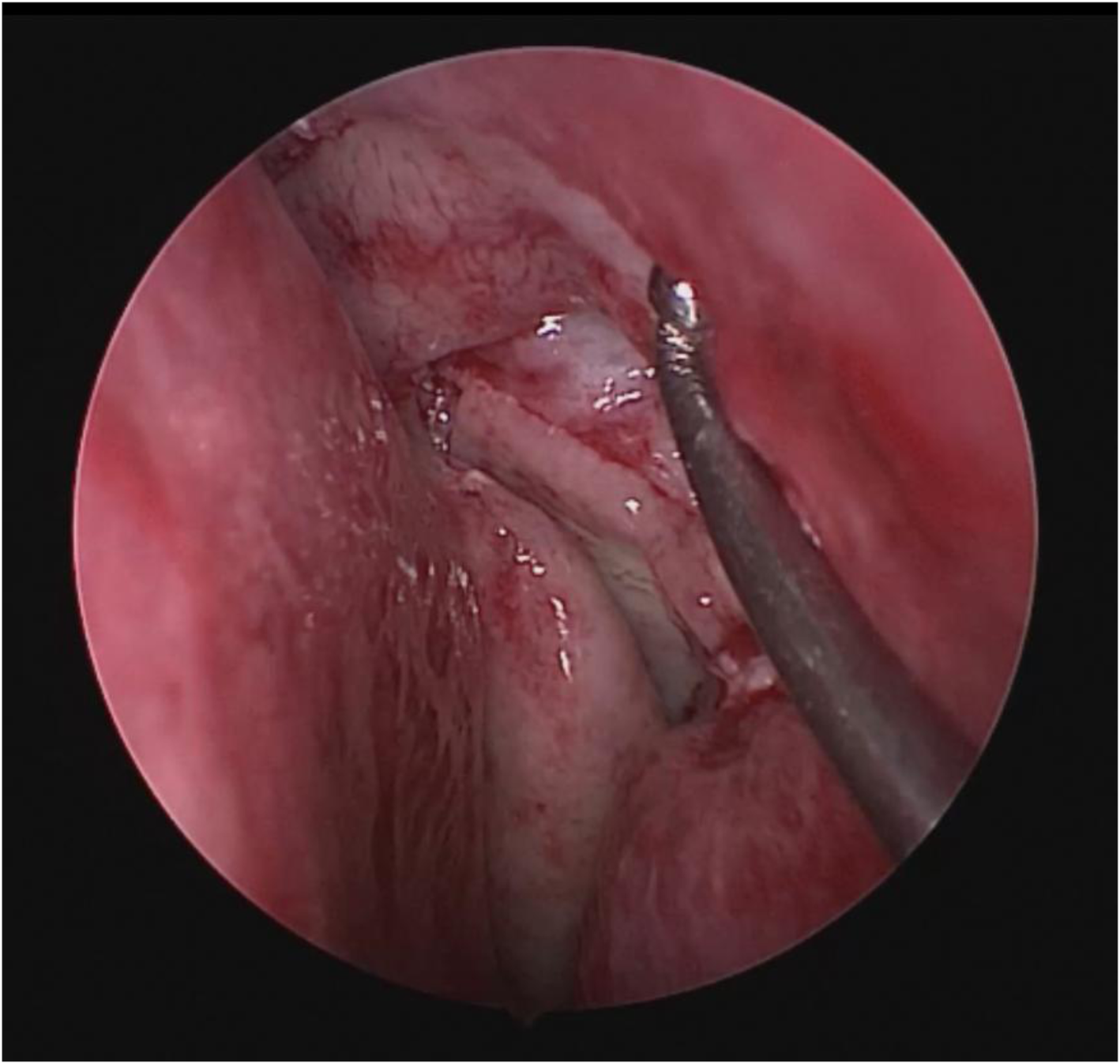
Fig. 4. Intra-operative view after mucosal flaps were laid over the lacrimal flaps
Technique without flap preservation
After the curvilinear incisions described before, only an inferior horizontal incision was made without a posterior 2–4 mm extension. The superiorly based elevated nasal mucosal flap was dissected with nasal scissors and was trimmed. A similar 7–9 × 12–15 mm rectangular-shaped mucosal-free window was created without flap preservation (Figure 5a). The underlying frontal process of the maxilla and the lacrimal bone were removed with a cutting burr similarly. The sac was widely opened with a sickle knife to create an ‘H-shaped’ incision (Figure 5b). Neither stenting nor packing was used.
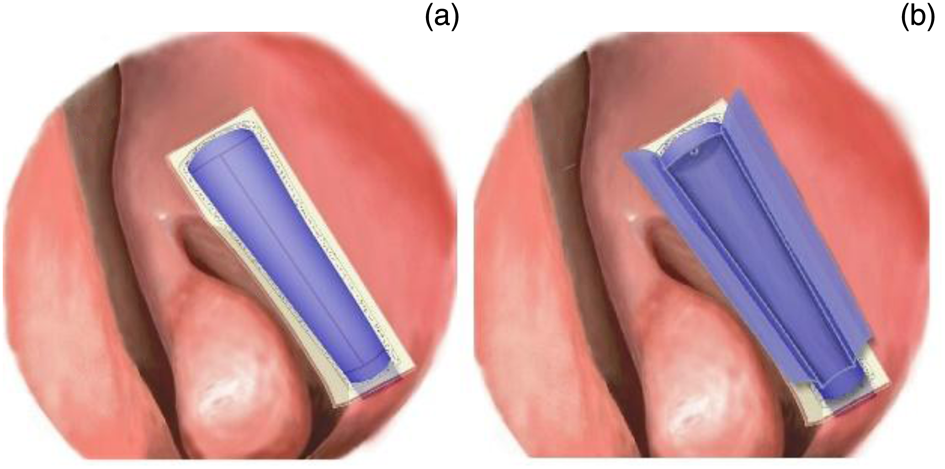
Fig. 5. Illustration of the endoscopic dacryocystorhinostomy technique without flap preservation. (a) The rectangular-shaped mucosal-free window was created without flap preservation and (b) the sac was widely opened after an ‘H-shape’ incision and lacrimal flaps were reflected
The data were analysed by using SPSS® (version 22) statistical software. The normality assumption was measured by the Kolmogorov–Smirnov test. Categorical variables were compared with the chi-square test, and scale variables were compared with a t-test. Results with a significance coefficient of p > 0.05 were considered statistically significant. The study protocol was approved by the Ethics Committee of the affiliated university (approval number: 06-19/01/2017). Written consent was obtained from the participants.
Results
A total of 104 endoscopic DCR procedures without stenting were performed in 96 patients. Six patients (lacrimal and double nasal mucosal flaps: 2; endoscopic DCR without flap preservation: 4) were lost to follow up and were excluded from the final analysis. Finally, the results of 96 endoscopic DCR surgical procedures without stenting in 90 patients were evaluated.
The mean age of the patients was 53.1 ± 14.4 years. The mean follow-up period was 25.8 ± 8.4 months. The operation time was 29.7 ± 6.7 minutes in the endoscopic DCR without flap preservation group and 27.7 ± 8.1 minutes in the lacrimal and double nasal mucosal flaps group, and the difference between the groups was not statistically significant (p = 0.122; Table 1). Forty-six patients were included in the lacrimal and double nasal mucosal flaps group and 44 patients were included in the endoscopic DCR without flap preservation group. The female to male ratio was 2.06 (31:15) in the lacrimal and double nasal mucosal flaps group and 2.14 (30:14) in the endoscopic DCR without flap preservation group. Four patients in the lacrimal and double nasal mucosal flaps group and two patients in the endoscopic DCR without flap preservation group underwent bilateral endoscopic DCR surgery. Demographic and clinical data of the patients are summarised in Table 2.
Table 1. The average and standard deviation of age, follow-up period and operation time

DCR = dacryocystorhinostomy; SD = standard deviation
Table 2. Distribution of findings according to study group

* Statistically significant value. DCR = dacryocystorhinostomy
After six months, functional success rates, evaluated by using the endoscopic fluorescein dye test in both groups, were 89.6 per cent and 97.9 per cent, respectively (p = 0.092). Nine patients (18.8 per cent) in the endoscopic DCR without flap preservation group and two patients (4.2 per cent) in the lacrimal and double nasal mucosal flaps group (p = 0.025) had insufficient healing one week after surgery. Granulation tissue formation at the end of the second month was detected in nine patients (18.8 per cent) in the endoscopic DCR without flap preservation group and in one patient (2.1 per cent) in the lacrimal and double nasal mucosal flaps group (p = 0.008). Mucosal scar contracture rates between the study groups were not significantly different (Table 2). No complications were detected in either study groups after surgery. Among the patients who were considered to be functionally unsuccessful, two patients had mucosal contracture and granulation tissue formation around rhinostomy, four patients had only granulation tissue and one patient had contracture.
Discussion
Granulation tissue formation is among the leading causes of failed endoscopic DCR surgical procedures.Reference Ali, Psaltis, Murphy and Wormald1,Reference Ali, Psaltis, Bassiouni and Wormald2,Reference Kim, Kim, Jin, Kim and Hwang10–Reference Dave, Mohammed, Ali and Naik14 Kumar et al.Reference Kumar, Mishra, Sethi, Mallick, Maggon and Sharma15 examined a 20-year time frame and 423 endoscopic DCR cases retrospectively, and they found synechiae with a rate of 6.1 per cent and perirhinostomal granulation tissue, with a rate of 3.7 per cent, as the most common reason for failure and recurrence. A systematic review of the literature for mucosal and lacrimal flap technique in endoscopic DCR surgery was performed by Green et al.Reference Green, Gohil and Ross16 in 2016. They reported that granulation tissue and synechiae were the most common causes for the reclosure of the nasolacrimal stoma after endoscopic DCR operations. They suggested that mucosal-sparing techniques had decreased granulation tissue formation and did not have different complication rates.Reference Green, Gohil and Ross16 Önerci et al.Reference Önerci, Orhan, Öǧretmenoǧlu and Irkeç11 showed development of granulation tissue, especially around the silicone tube, with a rate of 3 per cent. They considered granulation tissue formation as the most common reason for failed endoscopic DCR operations. In this study, the rate of recurrent nasolacrimal obstruction because of exposed bone spicules in the nasal cavity was reported as 3 per cent.Reference Kim, Kim, Jin, Kim and Hwang10 In accordance with the literature, the two most common pathologies causing rhinostomy contraction were granulation tissue (n = 10) and scar contracture (n = 5). After the post-operative treatment with nasal steroid sprays and local debridement, granulation tissue caused surgery failure in five patients and scar formation in one patient.
The benefits of silicone tube insertion or stenting are questionable.Reference Kumar, Mishra, Sethi, Mallick, Maggon and Sharma15 Successful results have been reported in the literature without using silicone tube insertion and using mucosal flaps.Reference Ciğer, Balci, Arslanoğlu and Eren17,Reference Kingdom, Barham and Durairaj18 A meta-analysis of long-term outcomes after DCR showed success rates of 94 per cent with stent placement versus 90.6 per cent without stent placement.Reference Kingdom, Barham and Durairaj18 The authors restricted indication of the use of silicone tube insertion with or without mucosal flaps as they may increase the formation of granulation tissue.Reference Kingdom, Barham and Durairaj18–Reference Liang and Lane21 Longari et al.Reference Longari, Dehgani Mobaraki, Ricci, Lapenna, Cagini and Ricci22 compared the results of endoscopic DCR procedures with or without silicone tube insertion with posterior based mucosal flap preservation, and they reported a higher percentage of rhinostomy closure in the stent group, mainly because of peristomal granulation formation (odds ratio, 3.64) and scar tissue formation (odds ratio, 2.25). However, another meta-analysis reported that there was no significant difference in the surgical complication rate or the risk of synechia and granulation tissue formation between the endoscopic DCR procedures with and without stent placement.Reference Kang, Shim, Shin, Kim, Lee and Jung23 We prefer the silicone tube insertion application in a limited number of indications, which are also mentioned in the literature.Reference Kingdom, Barham and Durairaj18
Çukurova et al.Reference Çukurova, Caner Mercan, Çetinkaya, Gümüsssoy and Söken24 used a posterior based single mucosal flap in 126 endoscopic DCR cases and reported the surgical success rate as 93 per cent with silicone tube insertion. They detected granulation tissue formation in 9 patients (7.2 per cent) as the cause of failure.Reference Çukurova, Caner Mercan, Çetinkaya, Gümüsssoy and Söken24 Pradhan et al.Reference Pradhan, Bhardwaj, Mandal and Majhi25 operated on 28 patients diagnosed with nasolacrimal duct obstruction with the preservation of posterior mucosal and lacrimal flap with silicone tube insertion. After a 12-month follow-up period, the recurrence rate was 12 per cent (3 patients), and they found that peristomal granulation tissue was the cause of obstruction in all 3 patients with recurrence. Janakiram et al.Reference Janakiram, Suri and Sharma12 described an inferiorly based mucosal flap technique without stenting (success rate, 95.2 per cent), and they recommended this modified endoscopic DCR technique for avoiding bone exposure, granulations and delay of mucosal healing. Kansu et al.Reference Kansu, Aydin, Avci, Kal and Gedik20 compared the surgical outcomes of 27 endoscopic DCR procedures with posterior mucosal flap preservation with the outcomes of 51 endoscopic DCR procedures with removal of posterior mucosal flap. A silicone tube insertion was performed for all patients. They reported the surgical success rates of endoscopic DCR with and without mucosal preservation as 100 per cent and 88.3 per cent, respectively (p = 0.080). They found granulation tissue formation in one patient (3.7 per cent) in the mucosal flap group and in seven patients (13.7 per cent) in the group without mucosal flap preservation.Reference Kansu, Aydin, Avci, Kal and Gedik20
Yuen et al.Reference Yuen, Lam, Tse, Chan, Wong and Chan26 defined a large posterior lacrimal flap technique for endoscopic DCR surgery with silicone tube insertion. They reported the success rate as 89.1 per cent (41 of 46) in the lacrimal flap group and 71.7 per cent (38 of 53) in the group without flap preservation (p = 0.031). In this study, granulation tissue formation was detected in 6.5 per cent (3 of 46) of patients with a lacrimal flap and in 17.0 per cent (9 of 53) of patients with flap removal. Granulation tissue leading to closure of the rhinostomy site (66.6 per cent)Reference Yuen, Lam, Tse, Chan, Wong and Chan26 was considered as the main reason for failure. Similarly, Mueller et al.Reference Mueller, Freitag, Lefebvre, Lee and Bleier27 described a superior based flap technique for revision endoscopic DCR surgery. Silicone tube insertion was also performed for all patients. They reported both anatomical and functional success rates of 100 per cent, after a mean follow up of 26.93 ± 10.33 months. The authors did not report any granulation tissue formation, synechiae or other post-operative complications.Reference Mueller, Freitag, Lefebvre, Lee and Bleier27
Massegur et al.Reference Massegur, Trias and Adema28 defined an endoscopic DCR technique with superior and inferior mucosal flaps overlying a posteriorly based lacrimal flap and compared the results with an inferiorly based mucosal flap technique. In this study, all endoscopic DCR procedures were performed in conjunction with silicone tube insertion. They found a success rate of 87.5 per cent in the double mucosal flap group and 92.7 per cent in the single mucosal flap group. Granulation and synechia were detected with a rate of 3.1 per cent and 10.4 per cent in the single mucosal flap group and 7.5 per cent and 7.5 per cent in the double mucosal flap group, respectively.Reference Massegur, Trias and Adema28
Ji et al.Reference Ji, Zhong, Tu and Wu29 described a V-shaped posteriorly based mucosal flap in combination with the posteriorly based lacrimal flap without silicone tube insertion. They compared the results with the removed nasal mucosal flap group and found a significant success rate with lower complication ratios. They reported a success rate of 98 per cent in the flap group and 84 per cent in the resection group (p < 0.05). They also detected a high granulation rate of 39 per cent in the mucosal resection group versus 15 per cent in the mucosal flap group (p < 0.05). One-year follow up of patients showed scar tissue formation in the mucosal preservation and resection groups (9 per cent and 31 per cent, respectively; p < 0.05).Reference Ji, Zhong, Tu and Wu29 Zloto et al.Reference Zloto, Koval, Yakirevich, Ben Simon, Weissman and Ben Artsi30 compared the results of two endoscopic DCR techniques with or without mucosal flaps in addition to silicone tube insertion. There was no significant difference in surgical success rates between procedures (86.8 per cent versus 82.1 per cent, respectively; p = 0.478). Data for granulation tissue, scar or synechiae were not specified in this study.Reference Zloto, Koval, Yakirevich, Ben Simon, Weissman and Ben Artsi30 Wang et al.Reference Wang, Fang and Zhao31 defined a lobulated pedicled mucosa flap technique without silicone tube insertion, similar to the surgical procedure defined in this study. They reported 100 per cent anatomical success and 94 per cent functional success (mean follow-up period, 25.3 ± 1.2 months).Reference Wang, Fang and Zhao31 The success rates achieved in the current study are consistent with the literature (endoscopic DCR without flap preservation = 89.6 per cent vs lacrimal and double nasal mucosal flaps = 97.9 per cent; p = 0.092). In this study, the improvement in the endoscopic DCR without flap preservation group was significantly insufficient in the early two phases (coagulation and inflammation) of wound healing (Table 2). In the endoscopic DCR without flap preservation group, granulation tissue was significantly higher than that in the lacrimal and double nasal mucosal flaps group (18.8 per cent vs 2.1 per cent; p = 0.008). Granulation tissue formation, scars, synechiae and fibrosis, which are the most common causes of failure in endoscopic DCR surgical procedures, are actually related to the late phases of wound healing (tissue formation and remodelling).Reference Watelet, Bachert, Gevaert and Van Cauwenberge32
Granulation formation appears to be the major challenging factor regarding rhinostomy patency. Ali et al.Reference Ali, Wormald and Psaltis33 discussed the ostium granulomas following DCR in 47 patients with a follow-up period of 2 years. In this retrospective study, 30 per cent of the patients (n = 14) had previously undergone endoscopic DCR surgery. Six patients (12.7 per cent) underwent surgical excision following topical nasal steroid or intralesional triamcinolone treatment. The most common location of granulation tissue was reported as the edge granuloma in 46.8 per cent of patients. The authors emphasised the importance of superior edge granulomas, which are the most common, and pointed out the bare bones. The association between granulation tissue formation and functional success of endoscopic DCR was not discussed in this study. In the present study, granulation tissue formation was found in 10 patients at the end of the second month following surgery, and 4 of these patients spontaneously regressed by the end of the sixth month.
• Important endoscopic dacryocystorhinostomy (DCR) failure causes are rhinostomy in an anatomically inappropriate place, inadequate rhinostomy width, synechia formation and granulation tissue
• Mucosal flap techniques can reduce development of synechia and granulation tissue on the exposed bone areas
• Endoscopic DCR technique with mucosal and lacrimal flaps was superior to the technique with flap sacrifice for wound healing and granulation prevention
• Operative success, operative time and complication rates of both techniques are similar
• Mucosal and lacrimal flaps prevent wound complications associated with failure of endoscopic DCR operations
In endoscopic DCR with double mucosal flaps technique, surgeons used one mucosal flap to cover the denuded bone on the edge of the new ostium and the other flap to support the lacrimal flap posteriorly.Reference Zloto, Koval, Yakirevich, Ben Simon, Weissman and Ben Artsi30,Reference Wang, Fang and Zhao31,Reference Mueller, Freitag, Lefebvre and Bleier34 Endoscopic DCR surgical procedures create a mucosal defect in the lateral nasal wall. Subsequently, complications occur because of the exposed bone and inappropriate orientation of the mucosal wound borders. This study showed that the double mucosal flaps technique is a convenient procedure for the management of mucosal defects and related issues in endoscopic DCR. In accordance with findings in the literature, the lacrimal and double nasal mucosal flaps technique does not require silicone tube insertion and does not extend the operative time. The most important challenge of endoscopic DCR with mucosal flaps is the creation of mini-flaps endoscopically in the lateral nasal wall. The most common causes of failure reported in the literature are complications because of inadequate wound healing. Moreover, inadequate ostial patency can be associated with inappropriate bone repair. Unfortunately, there are no studies in the literature regarding the histopathological features. In the present study, the assessment of wound healing was accomplished by physical examination (clinical features). Recent studies have shown that endoscopic DCR with the mucosal flaps technique is advantageous over other procedures with flap sacrifice. Furthermore, the mucosal flaps seem to support the healing process. The output parameters in this study are subjective, and the team evaluating the results are the same authors (possibility of bias). In addition, the sample size in this study is small to make a valid comparison. These are the main limitations of this study.
Conclusion
This is a distinct study that compares endoscopic DCR with mucosal flaps and flapless techniques without using silicone tube insertion and provides a wound healing perspective for the management of endoscopic DCR success. The lacrimal and double nasal mucosal flaps technique is superior to endoscopic DCR without flap preservation, considering the potential complications of wound healing. Future research could examine the histopathological features with the mucosal preservation technique (lacrimal and double nasal mucosal flaps) in a larger sample.
Competing interests
None declared









