Introduction
The nasal vestibular cyst was first described by Emil Zuckerkandl in 1882 and is also known as the nasoalveolar cyst or Klestadt cyst. It is a non-odontogenic, soft-tissue lesion that occurs in the superior region of the upper lip or at the base of the nasal ala, lateral to the midline. It originates from the entrapment of embryonic nasal epithelium in a facial cleft and is formed by the merging of the maxillary, medial and lateral nasal processes.Reference Chen, Su, Lin and Hwang1 Nasal vestibular cysts are usually unilateral, more common in women and typically arise during the fourth and fifth decades of life. A slowly growing painless swelling behind one nasal ala is the usual presenting complaint.Reference Chen, Su, Lin and Hwang1–Reference Sheikh, Chin, Fang, Liu, Baredes and Eloy3
In the past, patients usually underwent surgical removal of the cyst via a transoral sublabial transverse incision. But within a period of time, post-operative patients sometimes complained of facial or perinasal swelling and numbness. Recently, endoscopic endonasal marsupialisation (or excision) has been more frequently reported in the literature.Reference Chen, Su, Lin and Hwang1,Reference Su, Chien and Hwang4,Reference Hao, Yan and Tao5 However, a recent meta-analysis showed that the post-operative facial or perinasal swelling, pain, and overall recurrence rates of the two approaches do not have a statistically significant difference.Reference Sheikh, Chin, Fang, Liu, Baredes and Eloy3
In this study, our team used a transoral sublabial approach but modified the incision from a transverse incision to a longitudinal incision to remove the nasal vestibular cyst. We report the surgical results and discuss the benefits of this modified surgical procedure.
Materials and methods
Clinical data
This was a prospective case series study. A total of 28 patients diagnosed with a nasal vestibular cyst were included in this study series from January 2015 to December 2019. This study took place at the Department of Otolaryngology–Head and Neck Surgery, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China.
The diagnosis of nasal vestibular cyst was based on anatomic location, computed tomography (CT) scanning (Figure 1a and b) and histopathological findings. Odontogenic cysts and maxillary bone cysts were excluded from this study. This study was approved by the Ethical Committee of the Tongji Medical College at Huazhong University of Science and Technology.
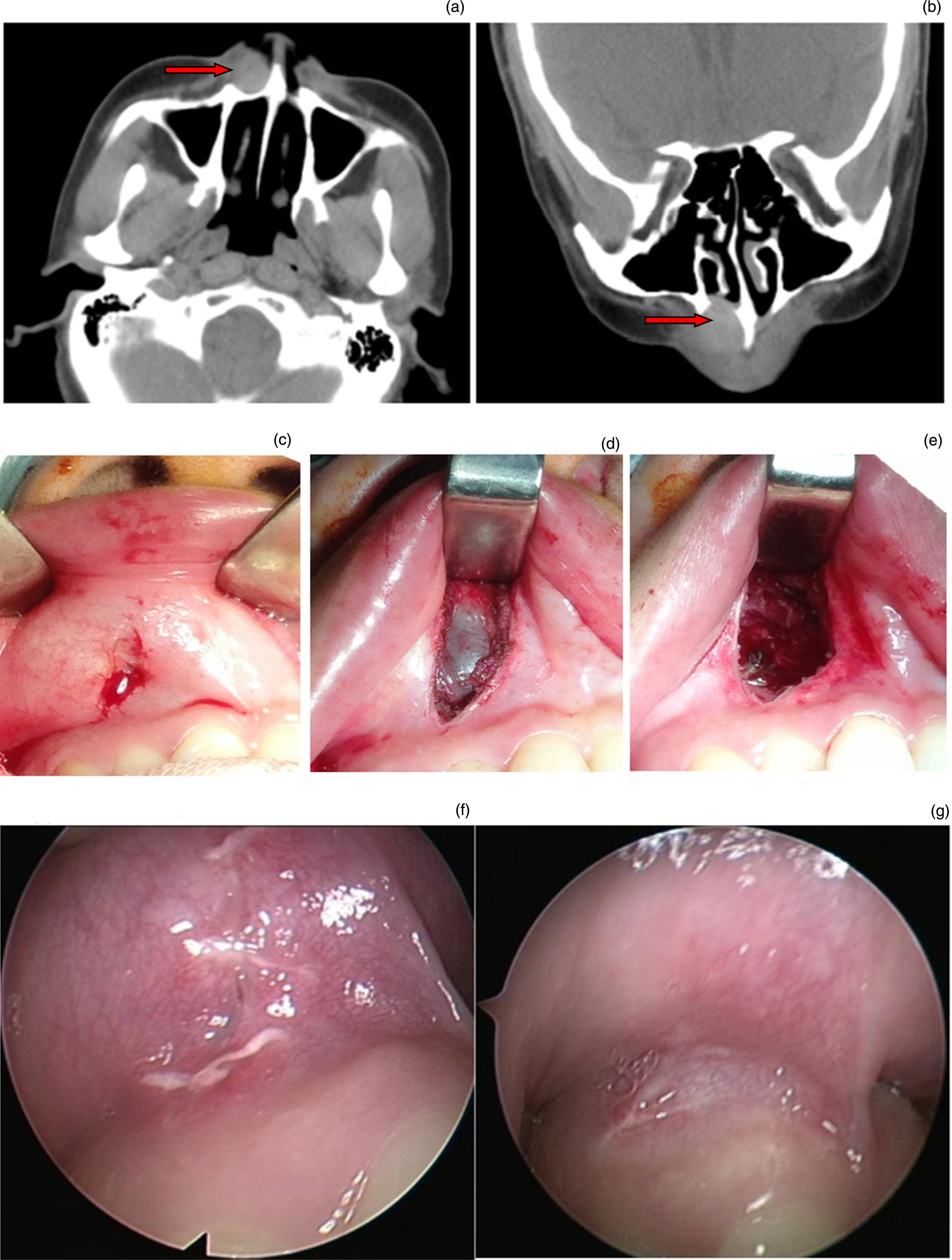
Fig. 1. A case of a nasal vestibular cyst. (a) Axial plane and (b) coronal plane pre-operative paranasal sinus computed tomography images showing a right nasal vestibular cyst with a distinct border (the red arrow indicates the mass). (c) A modified longitudinal incision at the most prominent point of the cyst via a transoral sublabial approach. (d) The cyst was revealed. (e) The cyst was completely removed: the surgical field was clear. (f) The incision reached clinical primary healing on the 7th day after surgery. (g) The incision was completely healed on the 30th day after surgery.
The main clinical information collected included main medical history, clinical presentation, pre- and post-operative condition, histopathological findings, complications, and follow-up outcomes.
Surgical procedure
Under general anaesthesia through an orotracheal intubation, all cases underwent operation to remove the nasal vestibular cyst through a modified transoral sublabial longitudinal incision. Each patient was supine with a neutral head position. A tracheal tube was fixed on the opposite side of the cyst. Oral mucosa was sterilised routinely. A longitudinal incision was made on the hump of the upper alveolar ridge (Figure 1c). Following elevation of a mucoperiosteal flap, the cyst was revealed (Figure 1d). A combination of blunt and sharp dissection was performed along the surface of the cyst, carefully separating the cyst and the surrounding tissue until it was completely removed (Figure 1e). The cyst was sent for histopathological examination. Bleeding of the surgical field was stopped by bipolar coagulation, and the incision was sutured with an absorbable suture after irrigation. Nasal packing was necessary only if the floor of the nasal vestibule and nasal cavity was broken. Post-operative management was typical, including antibiotics, oral health and so on.
Efficacy evaluation
Post-operative complications such as haematoma, infection, oronasal fistula, malformation and recurrence were recorded for each patient.
Patients were asked to mark degree of numbness of the nasal alar and upper lip on a visual analogue scale (VAS; Figure 2). A score of 0 indicated no numbness, and a score of 10 indicated the worst numbness imaginable. The degree of numbness was classified as mild (1–3), moderate (4–7) and severe (7–10).

Fig. 2. The visual analogue scale score. A score of 0 shows no numbness, and a score of 10 represents the worst numbness imaginable.
Results
The case series consisted of 2 male and 26 female patients (mean age: 42 years; range, 26–61), with 27 primary cases and one patient with recurrence. Symptom duration at the visit time varied from 3 months to 6 years. The main complaint was a gradually increasing mass in the nasal alar and upper lip. Thirteen of 28 patients had the cyst infection with pain and erythema. No nasal alar and upper lip numbness was recorded. The patient with recurrence, a 54-year-old female who complained of repeated mucus retention and erosion of the nasal vestibule after endoscopic endonasal marsupialisation in another hospital five years ago (Figure 3), had post-operative histopathological findings showing inflammatory granulation tissue with mucous glandular tissue on the surface.
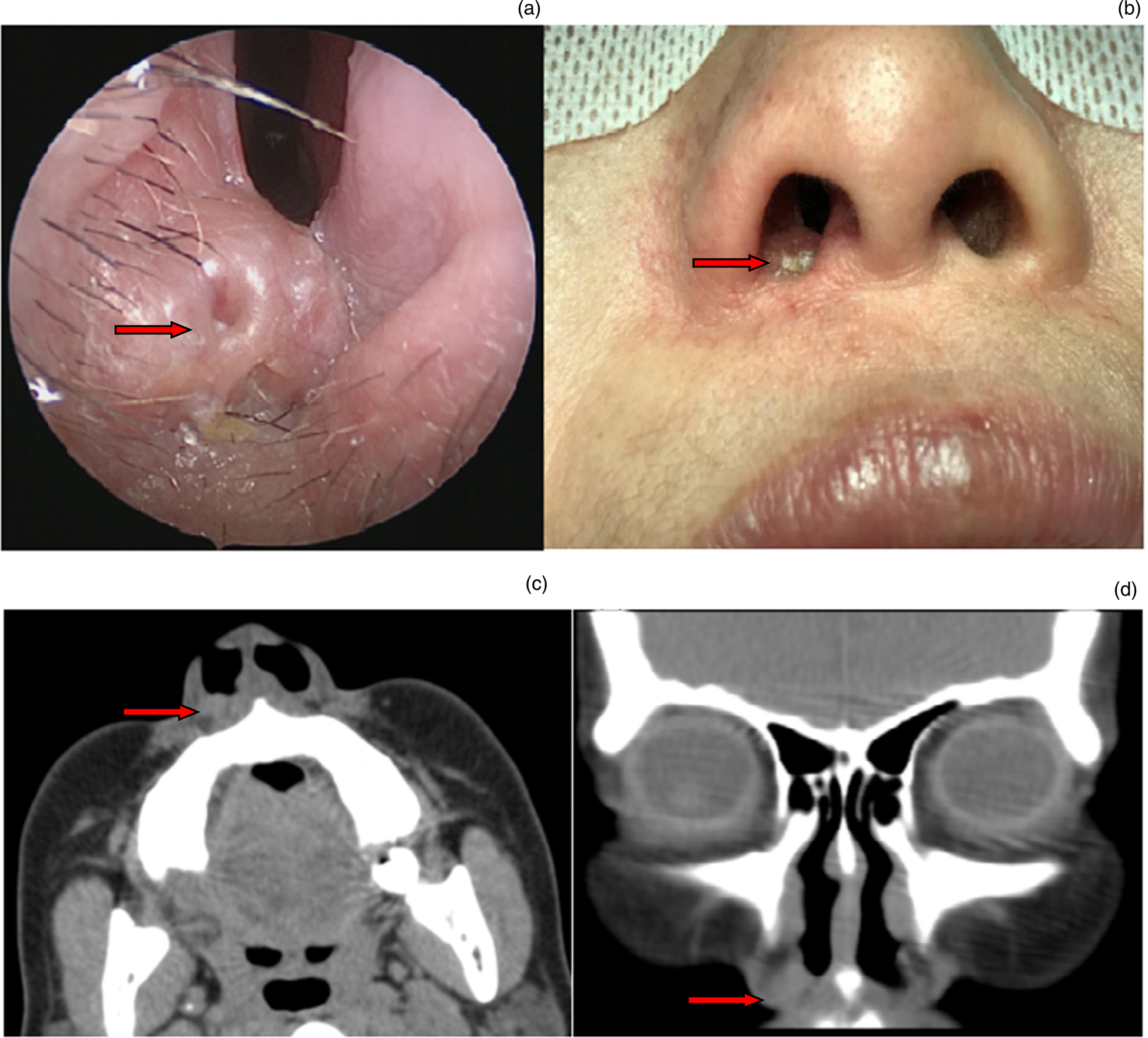
Fig. 3. A case of a recurrent nasal vestibular cyst after endoscopic endonasal marsupialisation. (a) Endoscopic view of a recurrent nasal vestibular cyst. (b) Infected skin of right nasal vestibule and upper lip. (c) Axial plane and (d) coronal plane pre-operative paranasal sinus computed tomography images showing the presence of a right nasal vestibular cyst. The red arrow indicates the mass.
All of the longitudinal incisions reached clinical primary healing one week after surgery. All patients were free of post-operative haematoma, infection, oronasal fistula and malformation (Figure 1f and g).
No patients complained of numbness of the nasal alar and upper lip before surgery. In the first week after surgery, the number of cases with a VAS score of mild, moderate and severe numbness was 4 (14.3 per cent), 1 (3.6 per cent) and 0, respectively. In the first month after surgery, the number of cases with VAS scores indicating mild, moderate and severe numbness were 1 (3.6 per cent), 0 and 0, respectively. The only patient who complained of mild numbness was fully recovered by the time she returned the following month. The patients were followed up for 2 to 57 months without recurrence.
Discussion
A nasal vestibular cyst is thought to be a cyst arising from non-odontogenic epithelium with secretory function. Two main theories have been put forward about their pathogenesis. One theory presumes that the cyst originates from entrapped embryonic nasal respiratory epithelium in a facial cleft. Another theory postulates that the cyst may emanate from misplaced epithelium of the nasolacrimal duct.Reference Yuen, Julian and Samuel6 The two theories may not be mutually exclusive as both show the cyst originates from respiratory epithelium with secretory function. Therefore, complete removal of the cyst was proposed to avoid the risk of mucus retention and infection induced by the secretory function of residual epithelium.Reference Yuen, Julian and Samuel6
A transoral sublabial approach is usually adopted to remove nasal vestibular cysts. A transnasal endoscopic approach has been more reported recently. In 1999, Su et al. firstly reported the method for transnasal endoscopic marsupialisation of a nasal vestibular cyst. All but 1 of the 16 patients were successfully treated with this technique, considered to be a new, less invasive method.Reference Su, Chien and Hwang4
Many studies comparing the above two approaches were reported recently. One author considered that transnasal endoscopic marsupialisation was an effective treatment for nasal vestibular cysts, associated with less cost and fewer complications than transoral sublabial excision. Meanwhile, they suggested that creating a sufficiently large stoma was crucial to prevent the retention of mucus or recurrence of the disease after marsupialisation. They considered that transoral sublabial excision may be a better choice than transnasal endoscopic marsupialisation in patients with small lesions.Reference Chao, Huang, Chang, Chen, Chen and Lee7 However, Li et al. considered that total excision via the sublabial approach was a more reasonable surgery than transnasal endoscopic marsupialisation of the cyst.Reference Li, Yang and Wang8 In this study, one recrudescent patient repeatedly suffered from mucus retention and erosion of the nasal vestibule after endoscopic transnasal marsupialisation in another hospital five years prior to the study (Figure 3). The histopathological specimen showed inflammatory granulation tissue with mucous glandular tissue.
In addition to transnasal endoscopic marsupialisation, there are also reports about transnasal endoscopic excision. In a study by Huang et al., transoral sublabial excision was performed in 23 patients with nasal vestibular cysts and transnasal endoscopic excision was performed in 30 patients. After comparing their duration of surgery, hospital stay time, total cost and incidence rate of post-operative lip swelling or numbness, it was concluded that the transnasal endoscopic excision was a simple, less invasive, low-cost and effective surgical procedure for the treatment of nasal vestibular cysts.Reference Huang, Li, Yang, Li, Ye and Liu9 In another study, 42 patients with nasal vestibular cysts underwent transnasal endoscopic excision, followed up for six months to five years, and no complications or recurrence were observed.Reference Hao, Yan and Tao5 However, in spite of the advantages of the transnasal endoscopic approach, a systematic review showed that transnasal endoscopic marsupialisation (or excision) and the transoral sublabial approach offered no statistically significant difference in post-operative facial or perinasal swelling, pain or overall recurrence rate.Reference Sheikh, Chin, Fang, Liu, Baredes and Eloy3
Findings from literature and clinical practice show that a classical transverse incision via a transoral sublabial approach may lead to higher incidence of post-operative nasal alar and upper lip swelling or numbness and more blood loss, whereas a transnasal endoscopic approach is prone to mucus retention, infection or recurrence due to stoma stenosis.
For a very small cyst, it is difficult to find the cyst in the nasal cavity through a nasal endoscope. Through study and review of anatomy, it was found that the nasal vestibule, nasal alar and upper lip are innervated by the infraorbital nerve, an entirely sensory nerve.Reference Hu, Kwak, Koh, Abe, Fontaine and Kim10,Reference Nderitu, Butt and Saidi11 The infraorbital artery, accompanying the infraorbital nerve, is located within the deep medial cheek fat and supplies the lateral nasal and superior labial regions.Reference Kim, Lee, Gil, Hu, Tansatit and Kim12 Both the infraorbital nerve and infraorbital artery branches are radially distributed from up to down.Reference Hu, Kwak, Koh, Abe, Fontaine and Kim10,Reference Kim, Lee, Gil, Hu, Tansatit and Kim12 According to the distribution characteristics of the infraorbital nerve and infraorbital artery, a modified longitudinal incision via transoral sublabial approach was designed to remove nasal vestibular cysts. Because the longitudinal incision is aligned with the direction of the branches of infraorbital nerve and infraorbital artery, it may avoid injuring infraorbital nerve and artery branches as much as possible, so as to alleviate post-operative nasal alar and upper lip swelling or numbness and reduce blood loss. In this study, 28 patients with a nasal vestibular cyst received a modified longitudinal incision via a transoral sublabial approach. All cysts were completely removed with little intra-operative bleeding and without significant post-operative nasal alar and upper lip numbness. No post-operative haematoma, infection, oronasal fistula and malformation occurred in any of the patients. All patients were followed up for 2 to 57 months without recurrence.
Conclusion
The modified longitudinal incision via a transoral sublabial approach is a simple, minimally invasive and effective surgical procedure for the removal of nasal vestibular cysts. The surgical procedure can alleviate post-operative nasal alar and upper lip numbness, reduce intra-operative blood loss and decrease recurrence.
Competing interests
None declared





