Introduction
Inverted papilloma is a benign epithelial growth derived from the underlying stroma of the nose and paranasal sinuses. It is invasive and associated with malignancy, with a propensity to recur. It constitutes 0.5–4 per cent of all primary nasal and paranasal sinus tumours, with an incidence of 0.6 cases per 1,00,000 people.Reference Hyams1 External surgery was previously considered the best surgical option for this condition. However, with the advent of endoscopes and powered instrumentation, an endoscopic procedure has become the standard of care for extensive inverted papilloma.Reference Jameson and Kountakis2
Materials and methods
A retrospective study of 10 sinonasal inverted papilloma patients was conducted in a semi-urban location from June 2010 to February 2014. All patients underwent anterior rhinoscopy, nasal endoscopy, contrast-enhanced computed tomography (CT) imaging of the paranasal sinuses and pre-operative biopsy. After histopathological diagnosis of the tumours, all patients underwent an endoscopic procedure. Stage II tumours were removed using combined approach endoscopic sinus surgery, whereas stage III tumours were treated by endoscopic modified medial maxillectomy. All patients were followed up for between seven months and three years. One recurrence after combined approach endoscopic sinus surgery was later removed by endoscopic modified medial maxillectomy. No further recurrence was noted after long-term follow up. All cases were reported as inverted papilloma without malignant transformation.
To perform the modified endoscopic medial maxillectomy, the patient was placed in a reverse Trendelenburg position and local anaesthesia infiltrated. Part of the anterolateral maxillary wall adjacent to the pyriform aperture was then removed en bloc. After cauterising the pyriform aperture region with bipolar cautery, an incision was made over the bone forming the pyriform aperture (Figure 1). The musculoperiosteal flap was elevated from the anterolateral wall of the maxilla and three osteotomies were performed: an inferolateral incision from the inferolateral point of the pyriform aperture to a point 4 mm lateral to it; a superolateral incision from the superolateral point of the pyriform aperture to a point 3 mm lateral to it; and a lateral incision to join the two osteotomies already made (Figures 2 and 3). Removal of this bone causes the maxillary sinus to become continuous with the nasal cavity so that the tumour can be approached centrifugally. Next, the inferior turbinate was crushed and cut, and a debrider was used to debulk the tumour while retaining its pedicle, which is generally located at the lateral recess, floor or sinus ostium. For this, an incision was then made at the inferior meatus–bony osteotomy junction, and the ascending maxillary process was removed. Dacryocystorhinostomy was then performed, and the inner periosteum removed. Finally, the inner maxillary wall was drilled and cauterised at the tumour origin, followed by closure.
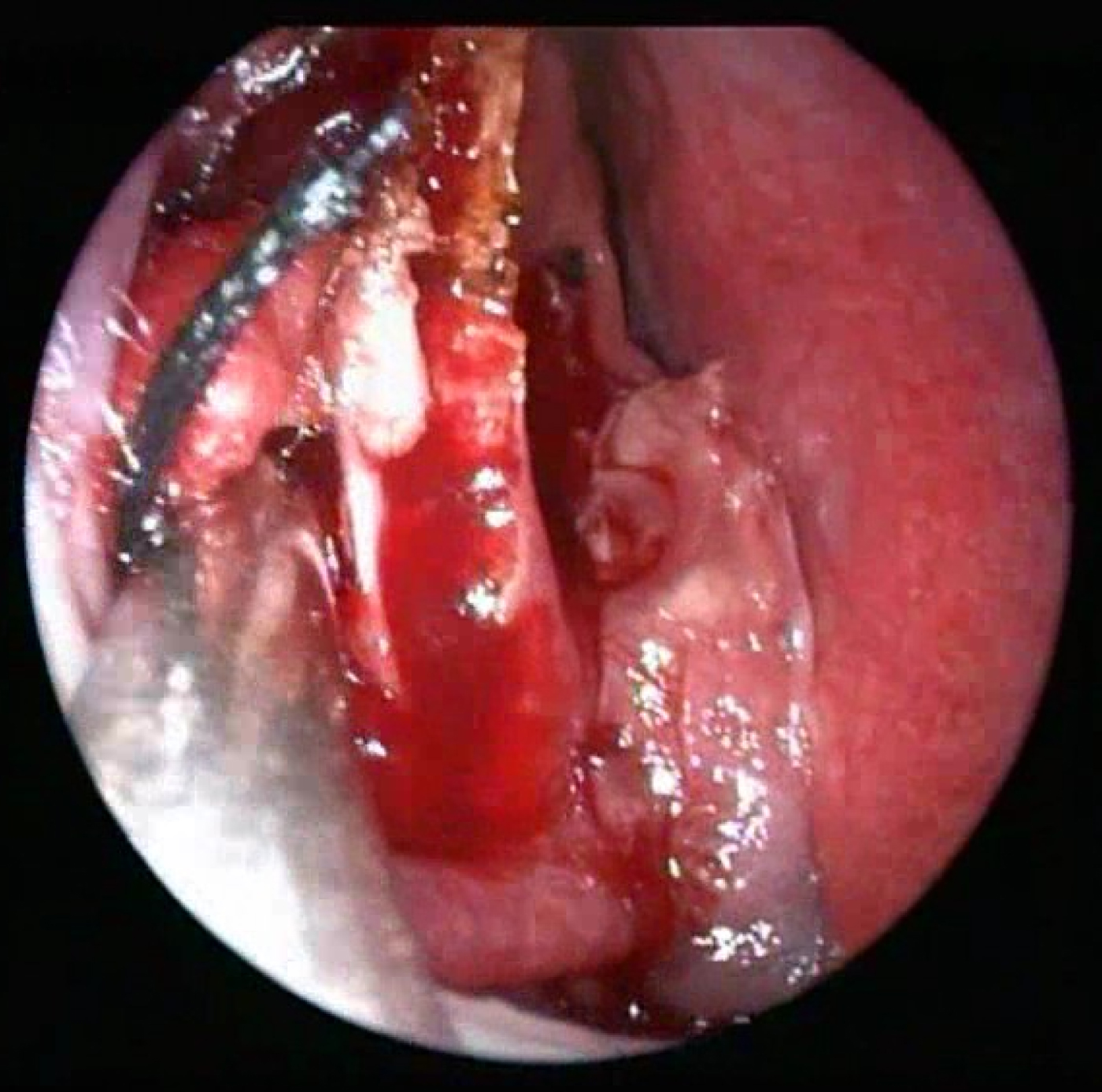
Fig. 1 Intra-operative photograph showing incision at the pyriform aperture (right side).

Fig. 2 Schematic diagram showing the sites of inferolateral osteotomy (ILO), lateral osteotomy (LO) and superolateral osteotomy (SLO).

Fig. 3 Intra-operative photograph showing the superolateral, inferolateral and lateral osteotomies at anterolateral maxillary wall (right side).
Results
This retrospective study analysed the age, sex, clinical behaviour, tumour origin, stage of presentation and surgical options of 10 inverted papilloma patients.
Patient characteristics
Most patients were aged 41–60 years, and most were male (male:female ratio 7:3). All patients had nasal obstruction, 8 (80 per cent) had a nasal mass, 8 (80 per cent) had nasal discharge and 5 (50 per cent) had epistaxis. Detailed patient characteristics are shown in Table I.
Table I Patient characteristics and treatment

Pt no = patient number; F = female; Rt = right; NO = nasal obstruction; EMMM = endoscopic modified medial maxillectomy; yr = years; M = male; CA-ESS = combined approach endoscopic sinus surgery; mth = months; Lt = left
Tumour origin and treatment
To standardise reporting and reduce selection bias, KrouseReference Krouse3 proposed a staging system for inverted papilloma based primarily on disease extent, location and the presence of malignancy (Table II).
Table II Krouse staging system for inverted papilloma3

PNS = paranasal sinus; OMC = ostiomeatal complex
In this case series, three patients presented at stage II and seven at stage III. The tumour originated from the maxillary floor in five patients, the middle meatus in three patients, and the lateral wall and anterior wall in one patient each. Three patients underwent combined approach endoscopic sinus surgery and seven underwent endoscopic modified medial maxillectomy (see Table I for details).
Discussion
In 1935, Ringertz described the histology of inverted papilloma as inversion of the underlying connective tissue. Norris later coined the term ‘inverted papilloma’.Reference Norris4 In 1975, Vrabec described the tumour as an ‘inverted Schneiderian papilloma’ because it was thought to arise from the Schneiderian membrane.Reference Vrabec5 The grossly inverted papilloma is pinkish-grey in colour, polypoidal, vascular, and exhibits exophytic growth with frond-like projections from the bulk of the lesion. Microscopic inspection shows that the epithelium rests on an intact basement membrane, with characteristic invaginations into underlying connective tissue stroma. Therefore, the lesion appears to be endophytic rather than exophytic from this perspective.Reference Han, Smith, Loehrl, Toohill and Smith6
Patients usually present with nasal obstruction, nasal mass, discharge from the nose and nasal bleeding; males are more commonly affected (male:female ratio 3:1). Inverted papilloma is usually unilateral, but is bilateral in 4.9 per cent of cases. Eighty-two per cent of inverted papilloma cases present with at least one sinus involved. Maxillary sinus involvement occurs in 69 per cent of cases, ethmoid sinus involvement in 53–69 per cent, sphenoid sinus involvement in 11–20 per cent and frontal sinus involvement in 11–16 per cent.Reference Krouse7 Consistent with previous reports, most patients in our case series were aged 41–60 years, with a clear male preponderance (male:female ratio 7:3).Reference Vrabec5, Reference Banhiran and Casiano8, Reference Batsakis9
The radiographic features of inverted papilloma comprise a heterogeneous mass with calcification and bony remodelling around the mass. Contrast-enhanced CT scanning shows bowing of the bones located near the mass, with widening of the infundibulum.Reference Phillips, Gustafson and Facer10 The constant pressure and mass effect commonly cause bony remodelling in the medial, anterior wall of the maxillary sinus and lamina papyracea.Reference Saha, Ghosh, Sen, Chandra and Biswas11 Magnetic resonance imaging shows the tumour to be iso- or hypointense on T1-weighted and hyperintense on T2-weighted images. The high recurrence, invasiveness and associated metachronous malignancy make radiological follow up imperative and drive the treatment strategy for inverted papilloma.
Complete resection of the neoplasm requires identification of the site where it is pedicled to the native mucosa. Pre-operative CT scanning and nasal endoscopy are used to plan the optimal surgical approach. An external approach (lateral rhinotomy and medial maxillectomy) with mid-facial degloving was originally adopted as the standard of care for inverted papilloma treatment. However, since the development of endoscopic sinus surgery in the 1980s, advanced endoscopic techniques have been used for extensive sinonasal neoplasm resection. In the endoscopic technique, the bulk of the tumour is first debrided, while retaining its pedicle attachment; the pedicle is then removed. The sinonasal cavity is optimally visualised and inspected to enable a more directed approach, while ensuring complete removal of the tumour and minimal damage to the surrounding mucosa. Once the tumour has been removed, the adjacent mucosa and underlying bone should be drilled or cauterised to remove tumour tissue located within the crevices of newly formed bone.
The aim of inverted papilloma surgery is complete resection, reduction of recurrence and post-operative tumour surveillance. The endoscopic approach meets all three criteria. Our preferred strategy is to treat stage I papillomas with endoscopic sinus surgery without much bone removal (Table III). In adjunctive procedures such as Caldwell–Luc, canine fossa trephination can also be added when treating stage II tumours to maximise visualisation and instrument access. Tumours of the maxillary sinus posterior wall can be approached via a large middle meatal antrostomy by removing bone posteriorly and superiorly.Reference Lawson, Le Benger, Som, Bernard and Biller12 For tumours originating from the anterior wall, a large area of the maxillary sinus that cannot be removed by combined approach endoscopic sinus surgery (that is, endoscopic sinus surgery with canine fossa trephination or Caldwell–Luc), should be approached via endoscopic medial maxillectomy. Tumours of the anterior wall, roof and floor of the maxillary sinus can also be removed using this technique. Stage III tumours of the frontal sinus can be treated via a modified Lothrop approach.Reference Banhiran and Casiano8 Tumours with extra-sinonasal extension and malignant transformation (stage IV) can be removed by an external approach such as lateral rhinotomy or a mid-facial degloving technique. By removing part of the anterolateral wall en bloc, the risk of tumour seeding is negligible.Reference Wormald, Ooi, van Hasselt and Nair13 In this technique, the most lateral recess of the maxillary sinus can be reached without the need for a septal window.
Table III Surgical options at our institute by tumour stage

ESS = endoscopic sinus surgery; CA-ESS = combined approach endoscopic sinus surgery; EMMM = endoscopic modified medial maxillectomy
The modified endoscopic medial maxillectomy technique is easy, reproducible, and requires less operative time than conventional endoscopic medial maxillectomy. However, there is a little more blood loss: 50 ml mean blood is lost in endoscopic medial maxillectomy versus 65 ml in endoscopic modified medial maxillectomy. Bleeding mostly occurred during osteotomies and removal of the anterolateral maxillary wall. This approach therefore provides excellent tumour exposure with minimal damage to the surrounding soft tissue and no cosmetic abnormality.
In this study, the recurrence rate was 10 per cent after the first procedure. Lawson et al. reported 12 per cent recurrence and Pasquini et al. reported a recurrence rate of only 3 per cent with endoscopic approaches.Reference Lawson and Biller14, Reference Pasquini, Sciarretta, Farneti, Modugno and Ceroni15 However, the endoscopic procedure is not without complication. The most common complication of endoscopic modified medial maxillectomy is crusting, which requires repeated clearance and clinic visits. Rare complications are epistaxis, temporary infra-orbital anaesthesia and periorbital ecchymosis.
• Inverted papilloma is a benign epithelial growth
• It is invasive, is associated with malignancy and has a propensity to recur
• Contrast-enhanced computed tomography imaging and biopsy are required for diagnosis and treatment planning
• Endoscopic medial maxillectomy is an excellent surgical option for extensive nasoantral inverted papilloma
• Removal of part of the anterolateral maxillary wall adjacent to the pyriform aperture makes the maxillary sinus continuous with nasal cavity and aids tumour access
• Removal of the tumour pedicle, adjacent mucosa and new bone by cautery or drilling reduces the recurrence rate
Most recurrences are noted within 5 years of diagnosis, but can be observed even after 10 years. Recurrence is not associated with cellular atypia or a specific histological pattern.Reference Batsakis9 Invagination of the mucosa into bony crevices occurs near the site of tumour attachment, and the formation of tumour tissue within these crevices leads to recurrence. Therefore, in our experience, removal of the mucosa and newly formed bone around the tumour pedicle is essential to reduce the recurrence rate of inverted papilloma.
Endoscopy helps visualisation of every nook and crevice of the sinonasal tract. Powered instrumentation, angled scopes and image guidance technology mean that the endoscopic approach is now the standard of care for extensive inverted papilloma.
Conclusion
This 3-year retrospective study involving 10 cases of histologically confirmed inverted papilloma indicates that pre-operative biopsy of the nasal mass should be mandatory for men aged over 30 years before a definitive surgical procedure is selected. Complete removal of the tumour pedicle and removal of the adjacent mucosa and newly formed bone around the pedicle is essential to reduce the likelihood of recurrence. Modified endoscopic medial maxillectomy is an easy, relatively quick and reproducible method that should be used to remove stage II and III inverted papillomas from the maxillary sinus.








