Introduction
Subperiosteal abscess is the most common complication of acute mastoiditis, and is usually present at the patient's initial visit to the emergency department, or complicates the course of the disease during hospitalisation.Reference Luntz, Brodsky, Alper, Bluestone, Casselbrant, Dohar and Mandell1 The diagnosis of a subperiosteal abscess can be based on clinical and radiological findings, and is confirmed definitively at surgery. The clinical diagnostic criteria are those of acute mastoiditis combined with retroauricular fluctuance and/or bulging of the postero-superior wall of the external auditory canal.
All researchers agree that parenteral antibiotics must be administered to patients suffering from acute mastoiditis with or without subperiosteal abscess formation. In contrast, a variety of surgical treatments for typical mastoid subperiosteal abscess (i.e. not associated with cholesteatoma or other intracranial complications) have been reported. Some ear surgeons favour the standard surgical approach, which includes myringotomy with or without ventilation tube insertion and simple mastoidectomy, as first-line treatment of subperiosteal abscess.Reference Gliklich, Eavey, Iannuzzi and Camacho2–Reference Neely, Brackmann, Shelton and Arriaga4 Other authors have reported more conservative surgical management, with myringotomy and incisional drainage or needle aspiration of the abscess, preserving mastoidectomy for refractory cases or those presenting with associated cholesteatoma or intracranial complications.Reference Bauer, Brown and Jones5–Reference Lahav, Handzel, Yehuda and Halperin7
At present, there is no commonly accepted optimal surgical treatment for mastoid subperiosteal abscess. Thus, we studied, and herein report, our results for the use of both approaches, that is, with and without simple mastoidectomy, in a large paediatric sample.
Patients and method
With the approval of the institutional review board, we retrospectively studied the medical records of 164 children admitted with a diagnosis of acute mastoiditis over a 9-year period (2002–2010). Thirty-four of these children also presented with a subperiosteal abscess. One case of subperiosteal abscess, associated with chronic otitis media and cholesteatoma, was excluded from the study.
The medical records of children with subperiosteal abscess were reviewed for: age; gender; history of pre-admission middle-ear infection; clinical signs; treatment before and after admission; surgical, bacteriological and radiological findings; and final outcome.
The diagnosis of acute mastoiditis and subperiosteal abscess was based on clinical grounds. The clinical criteria used to make the diagnosis of acute mastoiditis comprised: recent history, symptoms and signs of acute otitis media; retroauricular erythema and/or swelling and/or pain; and antero-inferior protrusion of the auricle. The diagnosis of subperiosteal abscess was based on clinical symptoms and signs of acute mastoiditis coupled with retroauricular fluctuance and/or bulging of the postero-superior wall of the external auditory canal. All subperiosteal abscess diagnoses were definitively confirmed or rejected intra-operatively.
Broad-spectrum intravenous antibiotics were given to every child with subperiosteal abscess immediately after admission.
First-line surgical treatment comprised either: (1) myringotomy and simple (cortical) mastoidectomy; or (2) myringotomy and drainage of the abscess, via incision or needle aspiration. Generally, children were treated with one of the two protocols irrespective of their clinical and laboratory findings on admission; the choice of treatment type was at the discretion of the ENT surgeon on duty, since both approaches were used in our department. However, the presence of an otogenic epidural or perisinus abscess was considered an indication for cortical mastoidectomy in all cases of acute mastoiditis with or without subperiosteal abscess.
In all cases, specimens of pus were obtained from the middle ear (during myringotomy) and from the abscess cavity, in the operating theatre, and sent for microbial culture and sensitivity testing.
In typical cases with an obvious clinical diagnosis, computed tomography (CT) scans were not ordered. Imaging studies (i.e. temporal bone CT or magnetic resonance imaging (MRI) or magnetic resonance angiography) were recommended only in cases of suspected intracranial complication, recurrent mastoiditis or atypical mastoiditis, when the diagnosis was in doubt.
All children were re-evaluated two to three days after admission. The initial management was deemed to be successful, or not, on the basis of the following clinical and laboratory criteria: progressive restoration of auricular displacement; regression of retroauricular local signs; and partial or complete recovery of non-specific inflammatory parameters (i.e. white blood cell count and differential analysis, C-reactive protein level and erythrocyte sedimentation rate). Unresponsive cases were further treated with simple mastoidectomy.
The t-test for normally distributed, two-tailed, independent samples was used to compare the mean hospital stay of the children treated with the two different surgical methods.
Results
The studied population consisted of 34 children (13 girls and 21 boys) aged from 2 months to 8 years (mean age, 31.6 months; median age, 27 months) suffering from mastoid subperiosteal abscess.
On admission, the presenting clinical signs were, in descending order of frequency: retroauricular inflammation (i.e. swelling and/or erythema and/or tenderness; n = 34, 100 per cent); auricle protrusion (n = 34, 100 per cent); retroauricular fluctuance (n = 26, 76.5 per cent); and postero-superior canal wall bulging (n = 22, 65 per cent).
Computed tomography or MRI scans were performed for eight children (23.5 per cent). Imaging studies were ordered for the following reasons: facial nerve paresis (n = 1); symptoms suggesting central nervous system involvement (e.g. unusual earache or headache, persistent high fever, unsteadiness, vomiting, or altered mental state; n = 4); persistent otorrhoea after myringotomy (n = 1); or persistence of clinical and laboratory findings for more than 3 days (n = 2). In one child, the mastoid subperiosteal abscess was associated with an epidural abscess, which was diagnosed on MRI (Figure 1).
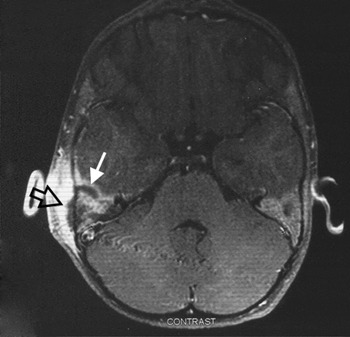
Fig. 1 Axial, T1-weighted magnetic resonance imaging scan with contrast, showing severe postauricular soft tissue thickening and a right mastoid subperiosteal abscess (outlined arrow) accompanied by a middle fossa epidural abscess (white arrow). Enhancement of the overlying dura of the middle cranial fossa can also be seen.
Twenty children had been prescribed oral antibiotics prior to admission: 10 were taking a second-generation cephalosporin, 3 amoxicillin-clavulanate, 3 low-dose amoxicillin and 4 a macrolide. All children received empirical intravenous antibiotics directly after admission. In most cases (32 of 34), a combination of a third-generation cephalosporin (cefotaxime or ceftriaxone) and clindamycin was given.
All children (n = 34) were operated upon under general anaesthesia within 24 hours of admission. Thirteen underwent myringotomy plus simple mastoidectomy. The remaining 21 underwent myringotomy plus abscess drainage, either by incision or needle aspiration. Six children also received an ipsilateral ventilation tube.
There were no observed treatment failures among the 13 children undergoing simple mastoidectomy. All these children were cured without any further complications or the need for additional therapeutic measures, having an uneventful post-operative period.
Of the 21 children treated with myringotomy and abscess drainage, 12 (57 per cent) were also cured without needing any supplementary treatment. However, nine (43 per cent) required simple mastoidectomy due to a deterioration, or lack of improvement, in their clinical condition and/or laboratory parameters within the first 48–72 hours. This second operating session took place on days 3 to 5 after admission. Following mastoidectomy, the nine children in this subgroup did not require any further intervention, and displayed a typical post-mastoidectomy course of recovery (Figure 2).
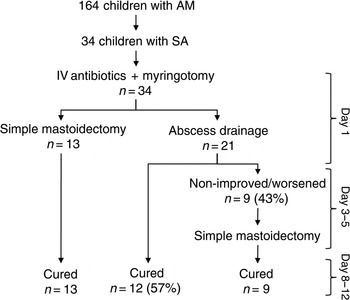
Fig. 2 Flow diagram showing the patients, methods and results of the study. AM = acute mastoiditis; SA = subperiosteal abscess; IV = intravenous
The mean duration of hospitalisation in our series was 10.37 days (standard deviation, 2.9 days; range, 5–18 days; median, 10 days). Children undergoing immediate mastoidectomy had a mean hospital stay of 10.1 days. Children who were cured with abscess drainage (without mastoidectomy) had a mean hospital stay of 7.2 days, while those who eventually required additional simple mastoidectomy had a mean stay of 11.4 days. There was no statistically significant difference in the length of hospital stay, comparing children undergoing simple mastoidectomy versus initial abscess drainage (with or without eventual additional simple mastoidectomy) (p = 0.762). However, children who did well with abscess drainage (without mastoidectomy) had a significantly shorter hospital stay than those of the same group who eventually underwent simple mastoidectomy (p = 0.024).
Two of the children undergoing simple mastoidectomy developed a surgical wound infection. There were no other complications during hospitalisation in this series. Radical or modified radical mastoidectomy was not employed.
The child with the epidural abscess was treated with ceftriaxone plus clindamycin for 18 days, myringotomy and simple mastoidectomy, through which the intracranial abscess was accessed and drained.
Analysis of the pus specimens collected during myringotomy revealed Streptococcus pneumoniae (n = 18, of which 10 were of medium sensitivity and 8 sensitive to penicillin), negative cultures (n = 5), Staph. coagulase-negative (n = 3), Str pyogenes (n = 3), mixed infections (n = 2), bacteroides species (n = 2) and Str constellatus (n = 1).
All children were given oral antibiotics for a further 7–10 days after discharge. The child with the epidural abscess received 15 days of oral antibiotic therapy.
All children received regular post-operative follow up for at least six months. No long-term intratemporal or intracranial complications, cases of masked mastoiditis, or other sequelae were noted.
One year after their first acute mastoiditis episode, two children suffered recurrent acute mastoiditis without subperiosteal abscess, and were readmitted and treated appropriately.
Discussion
Subperiosteal abscess, occurring as a complication of acute mastoiditis, has always been a surgical entity, and mastoidectomy has been the standard treatment. In 1983, Hawkins and Dru were the first to report incisional drainage of the abscess without mastoidectomy.Reference Hawkins and Dru8 However, three of their five patients required further surgery, consisting of mastoidectomy. Since then, a number of reports have appeared concerning the implementation of non-conventional management of mastoid subperiosteal abscess, using incisional or needle aspiration for draining the abscess cavity.Reference Bauer, Brown and Jones5–Reference Lahav, Handzel, Yehuda and Halperin7, Reference Khafif, Halperin, Hochman, Gertler, Poria and Shindel9, Reference Luntz, Brodsky, Nusem, Kronenberg, Keren and Migirov10 Most of these reports describe drainage of a mastoid abscess as an effective, safe procedure for treating acute mastoiditis with subperiosteal abscess, and one which enables avoidance of the more demanding and risky mastoidectomy. However, not all patients who had their abscesses thus drained experienced an uneventful post-operative period. In a considerable proportion of patients, multiple aspirations, repeated myringotomies or mastoidectomy were finally necessary, while others developed life-threatening intracranial complications while hospitalised and under treatment.Reference Lahav, Handzel, Yehuda and Halperin7, Reference Hawkins, Dru, House and Clark11, Reference Mallur, Harirchian and Lalwani12
In the majority of the children in the current study (21 of 34), primary surgical management included abscess drainage by surgical incision or needle aspiration, while 13 children were treated with a more aggressive protocol including simple mastoidectomy. The surgical approach was associated with myringotomy and parenteral antibiotic administration in all cases. Our results showed that abscess drainage by postauricular incision or aspiration was successful in 57 per cent of children, with no further surgery required. In the remaining 43 per cent of cases, abscess drainage failed to adequately improve the patient's clinical findings and/or laboratory parameters of acute mastoiditis, and simple mastoidectomy was eventually performed. Therefore, in our experience subperiosteal abscess drainage was not as effective as in other series, in which higher success rates (sometimes as high as 100 per cent) have been reported.Reference Taylor and Berkowitz6, 9, Reference Vera-Cruz, Roque Farinha and Calado13, Reference Tamir, Shwartz, Peleg, Shaul, Perez and Sichel14
On the other hand, in this study simple mastoidectomy proved an extremely efficient procedure for treating mastoid subperiosteal abscess, yielding the maximum success rate. None of our patients thus treated required a revision simple mastoidectomy. Additionally, there was no requirement to convert any patient's simple mastoidectomy into a radical or modified radical mastoidectomy, even in cases with contracted and sclerotic mastoid bones. Our one case with an epidural abscess was safely drained via simple mastoidectomy.
It is noteworthy that, apart from two surgical wound infections of minor importance, no intracranial or intratemporal complications were recorded in our series, either intra-operatively, post-operatively, or during the remainder of hospitalisation. Likewise, close, long-term post-operative follow up (at least six months) failed to identify any cases with long-term sequelae. We believe that this represents a finding of major clinical importance. In contrast, other authors have reported the development of severe intracranial complications, worsening of pre-existing ones, and the need for revision mastoidectomy, in children under treatment for acute mastoiditis.Reference Luntz, Brodsky, Nusem, Kronenberg, Keren and Migirov10, Reference Mallur, Harirchian and Lalwani12, Reference Migirov, Yakirevitch and Kronenberg15–Reference Quesnel, Nguyen, Pierrot, Contencin, Manach and Couloigner18
• There is currently no commonly accepted optimal surgical treatment for paediatric mastoid subperiosteal abscess
• This study assessed simple mastoidectomy versus abscess drainage
• Simple mastoidectomy proved to be an extremely effective procedure for the management of mastoid subperiosteal abscess
• Abscess drainage was safe but not always curative
• Abscess drainage plus myringotomy and appropriate antibiotics can be a first-line treatment, but poor responders require simple mastoidectomy
Prompt surgical measures undertaken within the first few hours of admission could account for this observed difference, regarding the appearance of severe complications in patients under treatment. Myringotomy accompanied by subperiosteal abscess or mastoid drainage was performed in all children on the day of admission. Moreover, we did not undertake repeated aspirations or incisional drainage following an initial unsuccessful attempt. Instead, such failures of initial abscess drainage led us to undertake simple mastoidectomy – the standard method of subperiosteal abscess treatment – within 3 to 5 days. Therefore, our patients remained exposed to an inadequately controlled, severe infection for only a short time period, and under the safeguard of broad spectrum antibiotics.
The selection of antibiotics appropriate for subperiosteal abscess treatment may be another reason for our patients' favourable clinical outcomes. All the children in our study received a combination of intravenous antibiotics, commencing at most few hours after admission, which theoretically covered almost the whole spectrum of micro-organisms known to be involved in acute mastoiditis. In our experience, combined antibiotic therapy (i.e. cefotaxime or ceftriaxone plus clindamycin) is a safer option for patients than monotherapy, without necessarily risking more adverse effects or costing more.
There was no significant difference between the duration of hospitalisation of children treated with mastoidectomy (n = 13) versus abscess drainage (n = 21). However, the operating time and the length of general anaesthesia were much shorter in children undergoing incisional or aspiration drainage, compared with those undergoing simple mastoidectomy.
Conclusion
Without overlooking the limitations of this retrospective review (i.e. a non-randomised study with relatively few patients), we can conclude that simple mastoidectomy remains the most reliable and effective procedure for the management of mastoid subperiosteal abscess. Drainage of the abscess was found to be a safe method, but statistically was clinically effective in only 57 per cent of our patients. Incisional and aspiration drainage techniques for mastoid subperiosteal abscess are both simple to perform, non-aggressive, quick, at low cost, and have no associated morbidity or local complications. They can be used as an initial, conservative approach for treating acute mastoiditis with subperiosteal abscess, in association with myringotomy and appropriate antibiotic coverage. According to our experience, however, non-responding patients should be treated with simple mastoidectomy in less than 5 days, in order to avoid the risk of further extension of the infectious process.




