Introduction
Branchial sinuses and fistulae are congenital neck lesions which result from maldevelopment of the branchial apparatus during embryogenesis.Reference Schroeder, Mohyuddin and Maddalozzo1 The branchial apparatus, a series of six paired arches each associated with an external cleft and an internal pouch, is responsible for forming structures of the head and neck.Reference Stulner, Chambers, Telfer and Corrigan2 It is hypothesised that incomplete obliteration of a cleft and/or pouch can result in either a fistula or a sinus, although sinuses are generally more common than fistulae.Reference O'Mara and Amedee3 Abnormalities arising from the second cleft are commonest, accounting for 90 per cent of all branchial anomalies. First cleft anomalies account for 8 per cent of lesions, whilst those arising from the third and fourth pouch are far rarer.Reference Rajshekhar, Jaka and Singh4
Branchial sinuses and fistulae most commonly present during childhood; some authors have suggested the average age of presentation to be 3.6 and 2.6 years, respectively.Reference Schroeder, Mohyuddin and Maddalozzo1 However, cases amongst adults are not unknown. Patients may present with an external opening of the tract in the neck associated with a mucinous discharge.Reference Schroeder, Mohyuddin and Maddalozzo1, Reference Link, Bite, Kasperbauer and Harner5, Reference Chismona, Tamiolakis, Proimos, Perogamvrakis, Korres and Papadakis6 Alternatively, there may be a lateral neck mass, as sinuses can be associated with cystic lesions.Reference Link, Bite, Kasperbauer and Harner5 Patients may complain of pain and swelling in the neck due to infection of the tract and abscess formation; infections may be recurrent.Reference Chismona, Tamiolakis, Proimos, Perogamvrakis, Korres and Papadakis6, Reference Seki and Himi7
Whilst the diagnosis is clinical, imaging is important to enable identification of the course of the tract and its relation to surrounding structures. This aids planning of surgical excision, the definitive treatment for branchial sinuses and fistulae.Reference Schroeder, Mohyuddin and Maddalozzo1, Reference Rajshekhar, Jaka and Singh4, Reference Nicollas, Ducroz, Garabedian and Triglia8 Incomplete excision can lead to recurrence complicated by infection.
We present two cases of branchial cleft abnormalities in which magnetic resonance imaging (MRI) was undertaken. Although the surgical procedure was not entirely planned according to the magnetic resonance images, in retrospect these scans were extremely accurate in defining the course of the abnormality in both cases.
Case reports
Patient one
A 38-year-old woman presented with a discharging opening over her lower left neck which had been present for as long as she could remember. Recently, there had been an increase in pain and discharge, associated with an episode of left-sided tonsillitis. She reported experiencing regular tonsillitis which was always worse on the left side.
Examination revealed a skin pit anterior to the inferior third of the left sternocleidomastoid muscle. There were no masses palpable in the neck. The left tonsil felt harder than the right, but there was no irregularity or ulceration.
An MRI scan showed a narrow tract leading from the skin opening down to the underlying sternocleidomastoid muscle (Figure 1). There was no cystic lesion apparent, and the scan was otherwise normal. Despite the lack of a fistula on the scan, it was felt that the most likely diagnosis was a branchial fistula between the left tonsil area and the skin.
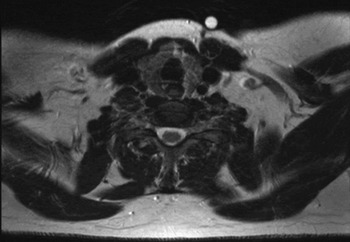
Fig. 1 Axial, T2-weighted magnetic resonance imaging scan of patient one, taken at the level of the thyroid gland. Extending from the skin marker (a cod liver oil capsule) on the left side of the neck, there is a T2 low signal tract which reaches the underlying sternocleidomastoid muscle. The lack of T2 high signal, and the fact that the tract is also of low signal on T1-weighted images, suggests that it is most likely to be the result of fibrous scar tissue and does not contain fluid. Imaging superior and inferior to this position failed to demonstrate any evidence of localised fluid collections or significant lymph node enlargement in the neck.
A decision was made to excise the tonsil and explore the tract. After performing an elliptical incision, the tract was followed superiorly and found to be a 6-cm, blind-ending sinus rather than a fistula. Histological analysis revealed a tract lined by respiratory-type epithelium, consistent with a branchial lesion.
Patient two
A 22-year-old woman presented with a skin opening over her lower right neck which had been discharging intermittently for a year. The patient recalled a neck swelling at the same site as a child, although this had not troubled her since.
Examination revealed a tiny opening in the lower right neck overlying the sternocleidomastoid muscle. This was diagnosed as a branchial sinus.
An MRI scan showed a 1–2 mm diameter tract extending cranially from the skin opening deep to the platysma on the anterior surface of the sternocleidomastoid muscle (Figure 2). At the level of the lower border of the mandible, the tract followed the anterior margin of the carotid sheath and coursed medially, where it became difficult to define from surrounding structures. There was no cystic lesion present.

Fig. 2 Axial, T2-weighted magnetic resonance imaging scan of patient two at (a) a level slightly inferior to the carotid bifurcation. The white arrow points to a low signal tract measuring 1–2 mm in diameter anteromedial to the right sternocleidomastoid muscle. Lack of T2 high signal implies that the tract was dry at the time of scanning. More superior to this position, the tract was seen to be positioned at the anterior margin of the carotid sheath and then to course medially towards the oropharynx, where it could not be clearly defined from the surrounding, normal anatomical structures.
An elliptical incision was made around the skin pit and the tract was dissected superiorly along the edge of the sternocleidomastoid muscle. A second incision was made two finger breadths below the mandible, and the tract was followed between the carotid vessels and deep to the digastric muscle. It was tied off where it entered the pharyngeal constrictor muscles.
Discussion
Established ENT texts fail to clarify best practice with regard to branchial lesion imaging. Indeed, the only suggested technique is a sinogram or fistulogram.Reference Hibbert and Kerr9 Although these have been reported to be useful in confirming the diagnosis, it has been suggested that other modalities are more appropriate. One study failed to find any advantage of using fistulography to aid excision, either pre- or intra-operatively.Reference Rattan, Rattan, Parihar, Gulia and Yadav10
The literature is largely dominated by case reports of third and fourth pouch branchial sinuses and fistulae, due to their rarity. There are only a few large-scale studies, and even fewer specifically concerned with imaging branchial anomalies. Nevertheless, some themes do emerge.
Although barium swallow studies have been considered useful in showing the presence of a tract in most cases, they can fail to show the tract if there is acute inflammation as this may occlude the tract opening.Reference Hamoir, Rombaux, Cornu and Clapuyt11, Reference Pereira, Losh, Oliver and Poole12 Their use is mainly reported in cases of third and fourth pouch anomalies, in cases with internal tract openings located in the pyriform fossae.Reference Link, Bite, Kasperbauer and Harner5, Reference Seki and Himi7, Reference Rea, Hartley and Bailey13
Although both barium studies and fistulograms may confirm the presence of a tract, cross-sectional imaging is necessary to delineate its anatomical course.Reference Seki and Himi7 Both MRI and computed tomography (CT) scanning are considered appropriate, however most authors favour CT.Reference Schroeder, Mohyuddin and Maddalozzo1, Reference Stulner, Chambers, Telfer and Corrigan2, Reference Chismona, Tamiolakis, Proimos, Perogamvrakis, Korres and Papadakis6–Reference Nicollas, Ducroz, Garabedian and Triglia8, Reference Hamoir, Rombaux, Cornu and Clapuyt11–Reference Park, Han, Sung, Kim, Kim and Chang14 When studies have compared CT with MRI directly, the focus has usually been the imaging of branchial cysts, which are demonstrated equally well by both modalities.Reference de Schepper, Monheim, Degryse and Van de Heyning15 In contrast, other authors have found that the MRI appearance of branchial lesions was variable compared with CT, and that, in one case of a sinus tract, the MRI scan was non-diagnostic.Reference Mukherji, Tart, Slattery, Stringer, Benson and Mancuso16 Despite this, it has been reported that both CT and MRI can identify the presence of a tract.Reference Keogh, Khoo, Waheed and Timon17 However, it is generally believed that, whilst both modalities can highlight inflammatory processes, CT is better at defining the tract because it can detect air density within it and has superior resolution.Reference Rea, Hartley and Bailey13, Reference Park, Han, Sung, Kim, Kim and Chang14, Reference Wang, Tiu, Chou and Chang18
Computed tomography fistulography is a relatively new technique in which dye is injected into the tract during CT scanning. This has been shown to be very effective, and has been reported to show the fistulous tract and its relationship to surrounding structures better than conventional CT.Reference Ryu, Lee, Lee, Lee, Choi and Kim19 Similar benefits have been reported for CT scanning undertaken shortly after a barium swallow study.Reference Yang, Cohen, Everts, Smith, Caro and Andersen20
Ultrasonography has been utilised in some cases, and may be a first-line investigation in children. It is effective in evaluating cystic lesions. However, its success in imaging sinuses and fistulae is variable, with reports that it failed to detect a tract in all patients studied (although the sample size was small).Reference Park, Han, Sung, Kim, Kim and Chang14, Reference Shrime, Kacker, Bent and Ward21 However, in certain cases in which air has been identified in the lateral neck, this has been considered pathognomonic of a third branchial cleft sinus.Reference Liberman, Kay, Emil, Flageole, Nguyen and Tewfik22
The two presented cases, encountered over a six-month period, illustrate the ability of modern MRI scans to accurately depict the extent and course of branchial cleft abnormalities. The MRI scans taken for these cases could have been relied upon to determine the necessary surgical procedure, to predict the length of operating time and to assist in obtaining informed patient consent.
• Branchial sinuses and fistulae, although uncommon, are not an insignificant ENT presentation
• Overall, there is little consensus on appropriate imaging for these abnormalities; however, in terms of cross-sectional imaging, computed tomography tends to be preferred to magnetic resonance imaging (MRI)
• We report two cases in which MRI accurately showed the extent and course of branchial sinuses; thus, we recommend MRI as first-line imaging both for diagnosis of these lesions, where appropriate, and for surgical planning
Of course, it must be remembered that imaging may not be required for typical second cleft sinuses and fistulae; therefore, the presented cases are purely illustrative of the capabilities of MRI with regard to such anomalies. However, first cleft sinuses and fistulae have a variable course and a close relationship to the facial nerve, and in this context accurate pre-operative imaging is important.Reference Solares, Chan and Koltai23 Imaging may also be necessary to confirm the diagnosis of a third or fourth pouch anomaly if there is any clinical uncertainty.
Although we present only a small case series, branchial cleft and pouch abnormalities are sufficiently rare for our findings to prompt recommendation of MRI as a first-line modality, if imaging is indicated.




