Introduction
Tonsillectomy is one of the most common elective surgical procedures performed in ENT. Post-tonsillectomy pain can be severe, and has negative effects on the patient's oral intake and time taken to return to their normal activities and daily life. Inflammation post-tonsillectomy is greatest on days 3 to 7, which coincides with maximum fibrin clot accumulation.Reference Isaacson 1 With separation of the fibrin clot, capillaries in the vascular stroma are exposed and vulnerable to minor trauma and bleeding;Reference Isaacson 1 hence, pain and risk of bleeding are greatest during this period of time.
Most adult patients are discharged home with strong analgesics such as opioids or opioid-like agents (Endone®, Panadeine Forte®, and tramadol). Opioids have side effects such as nausea, vomiting, constipation, respiratory depression and sedation. Non-steroidal anti-inflammatory drugs (NSAIDs) have been used in the past for post-tonsillectomy patients, but the potential risk of bleeding and gastrointestinal upset have caused some clinicians to use newer, more selective NSAIDs. These newer selective NSAIDs, also known as cyclooxygenase-2 inhibitors, such as celecoxib (Celebrex®), are associated with equivalent analgesic properties as classical NSAIDs, but have minimal side effects such as platelet dysfunction and gastrointestinal bleeding.
Classical NSAIDs block the synthesis of prostaglandins by inhibiting both constitutive cyclooxygenase-1 and inflammation-inducible cyclooxygenase-2. Cyclooxygenase-1 is known to be present in most tissues, and is thought to have a role as a housekeeper enzyme that regulates many normal physiological processes. Cyclooxygenase-1 inhibition may lead to operative site and gastrointestinal bleeding, and renal tubular dysfunction. In contrast, cyclooxygenase-2 expression is not detectable prior to an insult but increases rapidly in response to inflammation. Thus, cyclooxygenase-2 inhibition only leads to the anti-inflammatory, analgesic and antipyretic effects, without affecting the beneficial and protective effects of cyclooxygenase-1. In consequence, selective cyclooxygenase-2 inhibitors have been introduced as an alternative to the classical NSAIDs, in order to produce comparable analgesia without the potentially injurious side effects.
We hypothesised that if patients were to take one of the selective NSAIDs (i.e. cyclooxygenase-2 inhibitors) such as celecoxib, in addition to routine paracetamol and Endone (with the latter only being a rescue analgesic), that pain relief during the post-operative period would be better controlled. This may result in decreasing opioid (Endone) consumption, and improved recovery speed and experience. It was also anticipated that paracetamol (acetaminophen) may potentiate the analgesic and anti-inflammatory effects of the cyclooxygenase-2 inhibitors.Reference Graham, Graham and Day 2 This multimodal analgesic approach, in which different analgesics that act through different mechanisms and at different sites in the body are combined, results in additive and synergistic analgesia, with lowered adverse effects.Reference Buvanendram and Kroin 3 , Reference Kiefer and Dannhardt 4 Thus, we anticipated that ultimately there would be a reduction in the need and use of additional opioid analgesics and subsequently opioid-associated side effects.Reference Wickerts, Warrén Stomberg, Brattwall and Jakobsson 5
In accordance with our study objective, the primary endpoint was improvement of post-tonsillectomy pain in adult patients. Our secondary objectives were: to determine if the celecoxib group would take less opioid (Endone) overall, to assess whether their pain would be relieved earlier, to examine each group's re-admission rate, to assess the side effect profile of adult post-tonsillectomy patients and to determine the incidence of secondary haemorrhage post-tonsillectomy.
Materials and methods
All procedures contributing to this work complied with the ethical standards of the Australian guidelines. The study was approved by the Human Research Ethics Committee of Peninsula Health (protocol number: HREC/12/PH/55), and the Department of Health and Ageing, Therapeutic Goods Administration (trial number: 2013/0286). The study was registered with the Australian New Zealand Clinical Trials Registry (trial identification number: ACTRN12613000600741). The investigation complied with the Helsinki Declaration of 1975, as revised in 2008.
A single-centre (Frankston Hospital), double-blind, placebo-controlled, phase 3 clinical trial was conducted, from 2013 to 2015, in an adult population (aged 18–55 years), with a parallel group study design using an allocation ratio of 1:1.
A pre-study power analysis, based on the primary endpoint, estimated that 37 patients in each group would be required based on an arbitrarily chosen 20 per cent reduction in pain score and a standard deviation of 3. However, we decided to recruit 40 patients in each arm anticipating there may be a few dropouts. Differences were determined to be statistically significant when the p value was less than 0.05.
Patients were selected from the ENT surgical waiting list at Frankston Hospital. In total, 95 patients were interviewed in the out-patient clinic, by the operating surgeon, from June 2013 to June 2015, during the pre-operative stage, and were only selected if they satisfied the inclusion criteria. Patients included were aged 18–55 years, weighed more than 50 kg, and were undergoing either tonsillectomy or adenotonsillectomy, with indications for surgery being tonsillar hypertrophy, asymmetrical tonsillar enlargement, recurrent tonsillitis or previous quinsy. The exclusion criteria included: allergies to NSAIDs, opioids, codeine, Endone, paracetamol or sulphonamide; lactose intolerance; asthma; kidney, liver or cardiovascular disease; haemorrhagic diathesis; hypertension; obstructive sleep apnoea; or a requirement for other concomitant surgical procedures. Those patients who were taking NSAIDs (e.g. celecoxib, aspirin), who were on regular opiates or paracetamol, who had active peptic ulcer disease or gastrointestinal bleeding, or were taking medication that contained sulphonamide or other interacting drugs (such as warfarin, fluconazole or rifampicin) were also excluded. Women who were pregnant, nursing or trying to conceive were excluded too. Fourteen patients were excluded as they did not satisfy these criteria.
Informed written consent was obtained from each of the 81 selected patients during the pre-operative visit, before undergoing elective tonsillectomy at Frankston Hospital.
Of the 81 patients who had their tonsils removed, 1 was excluded from the study because of primary haemorrhage post-tonsillectomy; this was successfully managed on the ward and the patient was discharged home with tranexamic acid. The investigators decided not to include this particular patient in the study because the individual had been started on tranexamic acid and this would be a bias to whichever study group the patient fell into regarding incidence of post-tonsillectomy haemorrhage.
Eighty patients were recruited and randomly assigned into each study arm (40 patients per arm) (Figure 1). All patients received endotracheal intubation. There were no restrictions placed on the anaesthetist regarding the choice of drugs used during phases of general anaesthesia. However, as per the unit policy at Frankston Hospital, no NSAIDs were allowed for patients undergoing tonsillectomy during the peri- and post-operative periods, to avoid serious post-tonsillectomy haemorrhage due to any inhibitory effect of NSAIDs on platelet aggregation.

Fig. 1 Post-tonsillectomy trial flow chart. Eighty patients were recruited and divided equally into each arm, with no dropouts.
All patients were operated on by a single experienced surgeon, using a standardised method of electrodissection, with electrocautery set at 18 W (using a Valleylab Force FX™ Electrosurgical Generator C). Haemostasis was secured with cautery. The tonsillar fossae were soaked with local analgesic using 0.75 per cent ropivacaine (Naropin®) patties. Intra-operatively, all patients received 1.2 g intravenous benzyl penicillin as a prophylactic antibiotic and 8 mg of intravenous dexamethasone. Dexamethasone was given during tonsillectomy to reduce the incidence of post-surgical nausea and vomiting,Reference Tolska, Takala, Pitkäniemi and Jero 6 pain, and oedema, and to shorten the interval from surgery to food intake.Reference Kim, Lee, Kim, Ha, Lee and Yeo 7
Post-operatively, patients were transferred to the post-anaesthesia care unit for monitoring, and then moved to the ward once they had awoken and were deemed safe. During the post-operative period, patients received regular analgesics, with allowance for intravenous morphine or oral Endone (as a rescue analgesic), ondansetron and metoclopramide as anti-emetics, and other medications as deemed necessary. A single dose of 8 mg of intravenous dexamethasone was given in the morning on post-operative day 1 at 8:00 am.
All patients were discharged home after morning breakfast with regular medications and the study medication (package A or B, described below). Regular medications consisted of 1 g of paracetamol (4 times a day for 10 days), 500 mg of penicillin V (twice a day for 5 days), and 5 mg of Endone (6-hourly or when necessary, prescribed as a rescue analgesic; patients were given a maximum of 20 tablets).
Study medications were distributed by an independent pharmacist at the hospital with no clinical involvement in the study. The medications were distributed according to a randomised order, which had been generated using the randomisation function in Microsoft Excel® spreadsheet software (2010 version). Block randomisation was used with a predetermined ratio of 1:1 for every 20 participants. The celecoxib and placebo, which were identical in colour and size, were prescribed in capsule form. They were pre-packed in bottles and consecutively numbered for each participant according to the randomisation table. Each participant was assigned an order number and received the capsules in the corresponding pre-packed bottle. The allocation sequence and bottle contents were concealed from the investigator enrolling and assessing participants. This information was kept in sealed envelopes, stored in a locked cupboard, in the hospital pharmacy. Both the participants and investigators were blinded to the allocation.
Those who were assigned package A went home with the placebo medication: 1 capsule, twice a day, for 7 days. Those who were given package B went home with celecoxib 200 mg (Celebrex), twice a day, for 7 days.
The recording of pain and other secondary characteristics started from post-operative day 1 and continued to day 10. Patients measured their pain using an 11-point numeral rating scale, wherein 0 represented no pain and 10 represented the most severe pain ever felt. This numeral rating scale was chosen over other pain scales as it is a well-used, reliable and validated method of pain measurement.Reference Stelter, Hempel, Berghaus, Andratschke, Luebbers and Hagedorn 8 – Reference Ferreira-Valente, Pais-Ribeiro and Jensen 11
Patients completed the post-tonsillectomy diary at dinner time each day for the 10 days following surgery. This entailed: scoring their pain at rest, and when drinking and eating; recording the number of Endone tablets taken; noting any side effects; reporting any other medications taken that day; and recording those days when they experienced no pain on drinking or eating, or throughout the entire day, and the post-operative day that they returned to normal activities (Figure 2).
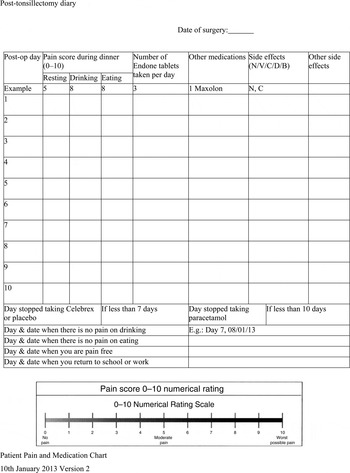
Fig. 2 Post-tonsillectomy diary. Participants were asked to complete the diary and return it to the investigator upon final review. Post-op = post-operation; N = nausea; V = vomiting; C = constipation; D = drowsiness; B = bleeding
All patients were followed up on post-operative days 5, 12 and 28 by the operating surgeon. Follow up on days 5 and 28 was conducted in person at Frankston Hospital. Follow up on day 12 was performed via a telephone call, unless the patient was sick and unwell, in which case they were required to present at the hospital for review by the investigator.
The post-tonsillectomy diary was collected during the final review on post-operative day 28. There were no dropouts and all patients were seen on final review with all diaries successfully completed (for every day) and collected. The sealed envelopes containing the allocation sequence and bottle contents information were opened only after the enrolled participants had completed the study (on day 28) and returned the post-tonsillectomy diary to the investigator.
Statistical methods
The collected data were entered into a Microsoft Excel spreadsheet. These data included: median pain scores at rest, and when eating or drinking, for each post-operative day (days 1 to 10); number of Endone tablets taken (per day and in total); number of participants who experienced nausea, vomiting, diarrhoea, constipation, bleeding or drowsiness; number of side effect incidents per day; first post-operative pain-free day; numbers and types of side effects encountered post-tonsillectomy; and incidence of post-tonsillectomy haemorrhage. The bleeding profiles were assessed using a four-point haemorrhagic scale.
The number of participants that experienced bleeding was analysed using the Pearson's chi-square test. As the data were not normally distributed, the severity of bleeding (based on the four-point haemorrhagic scale), and the re-admission rates for pain, vomiting, dehydration or poor oral intake, were analysed using a Wilcoxon–Mann–Whitney test to compare medians. Where possible, the effect size is shown by 95 per cent confidence intervals. In addition, when a contingency table contained a population of less than five, Fisher's exact test was used. All statistical analyses were performed using the Stata IC version 13 program (StataCorp, College Station, Texas, USA). Excel was also used to construct the graphs.
Results
Demographics
From June 2013 to June 2015, 80 patients were enrolled in the study, with 40 in the celecoxib group and 40 in the placebo group. The demographic and surgical characteristics of the two treatment groups are shown in Table I.
Table I Patient demographic and surgical data

Data represent numbers (and percentages) of participants. *n = 40; † n = 40; ‡ n = 80
Pain scores
As the data were not normally distributed, we compared median pain scores at rest (Figure 3), when drinking (Figure 4) and when eating (Figure 5) for the placebo and celecoxib-treated groups, for each post-tonsillectomy day (days 1 to 10). No statistically significant differences were observed in any of the three categories. The pain scores at rest, when eating and when drinking for each patient were summed, and the averages for the placebo versus celecoxib-treated groups were compared using a t-test for each day. However, there was still no statistically significant difference in pain on any day between the groups (Figure 6).

Fig. 3 Median pain scores at rest, from day 1 to day 10 (analysed using the Mann–Whitney test (p > 0.05 for all days, hence no significant between-group differences)).

Fig. 4 Median pain scores when drinking, from day 1 to day 10 (analysed using the Mann–Whitney test (p > 0.05 for all days, hence no significant between-group differences)).

Fig. 5 Median pain scores when eating, from day 1 to day 10 (analysed using the Mann–Whitney test (p > 0.05 for all days, hence no significant between-group differences)).

Fig. 6 Mean of all pains, from day 1 to day 10 (analysed using the Mann–Whitney test (p > 0.05 for all days, hence no significant between-group differences)).
Endone use
There was no statistically significant difference between the median total number of Endone tablets consumed by each group, with the celecoxib group patients taking a median of 22 Endone tablets each (interquartile range, 0–53) compared to a median of 18.5 tablets (interquartile range, 3–58) taken by patients in the placebo group (p = 0.48, Mann–Whitney test of median values; 95 per cent confidence interval = 0.35 to 0.61). In addition, there was no statistically significant difference in the number of Endone tablets taken when each day was compared (Figure 7).

Fig. 7 Total number of Endone tablets taken post-tonsillectomy, from day 1 to day 10 (analysed using the Mann–Whitney test (p > 0.05 for all days, hence no significant between-group differences)).
First pain-free day
There were no statistically significant differences in the first completely pain-free day (Table II). On average, it took approximately two weeks for pain to completely resolve. The pain-free period was defined as the first pain-free day reported, when there was no pain on drinking or eating, and the day the patient returned to work or college. The placebo group achieved an earlier pain-free time, with no pain when drinking at day 13 and no pain when eating at day 14. The celecoxib group were pain-free when drinking at day 13.5 and when eating at day 15. However, on average, both groups returned to work or college on the same day, day 15. The celecoxib group achieved a total pain-free day on day 16, 1 day earlier than the placebo group.
Table II Data regarding first pain-free days

*Analysed using the Mann–Whitney t-test (p > 0.05 for all parameters, hence no significant between-group differences). IQR = interquartile range; CI = confidence interval
Side effects
Only the following six side effects experienced post-tonsillectomy were recorded: nausea, vomiting, diarrhoea, constipation, bleeding and drowsiness. Of these, only vomiting was significantly different between groups; the number of vomiting episodes was higher in the celecoxib group compared to the placebo group (p = 0.001) (Figure 8). When the number of side effects experienced each day (from day 1 to day 10) were compared, both the placebo and celecoxib-treated groups reported the highest numbers on post-operative day 3, and the celecoxib group demonstrated significantly more side effects on day 9 (p = 0.02) and day 10 (p = 0.006) post-tonsillectomy (Figure 9).

Fig. 8 Frequency of each side effect in the 10 days post-tonsillectomy (analysed using the Mann–Whitney test). *Denotes a significant difference.

Fig. 9 Frequency of all side effects experienced in the 10 days post-tonsillectomy (analysed using the Mann–Whitney test). *Denotes significant differences.
Haemorrhage
Haemorrhage remains one of the most significant side effects following tonsillectomy. The best choice of analgesic is unclear because of the potential influences on the incidence and risk of haemorrhage. Although more patients from the celecoxib-treated group reported bleeding compared to the placebo-treated group, this difference was not statistically significantly different (p = 0.2, Fisher's exact test) (Table III).
Table III Frequency of bleeding by severity*

Data represent numbers (and percentages) of participants, unless indicated otherwise. *Categorised according to the four-point haemorrhagic scale: category 1 represents no bleeding; category 2 represents minimal bleeding, managed at home with ice gargling and cold packs (for up to 10 minutes); category 3 represents moderate bleeding, managed medically in hospital with ice gargling and silver nitrate cautery, without blood transfusion; and category 4 represents profuse bleeding, requiring general anaesthesia in the operating theatre or a blood transfusion. †Analysed using Fisher's exact test; no statistically significant differences were found.
Patients reported on bleeding severity using a four-point haemorrhagic scale, wherein 1 represented no bleeding; 2 reflected minimal bleeding, managed at home with ice gargling or cold packs (for up to 10 minutes); 3 referred to moderate bleeding, managed medically in hospital with ice gargling or silver nitrate cautery, without blood transfusion; and 4 represented profuse bleeding that required general anaesthesia in the operating theatre or a blood transfusion. The study did not show any statistically significant differences between the two groups of patients in terms of haemorrhage category. There was a two-fold increase in the incidence of minimal bleeds in the celecoxib group as compared to the placebo group. Compared to placebo, celecoxib resulted in a relative risk of 2.3 of having a minor bleed, and a relative risk of 0.38 of having a moderate bleed as compared to no bleed at all. Participants in the celecoxib group were 1.6 times more likely than those in the placebo group to experience bleeding.
Re-admissions
Six patients from the celecoxib-treated group and four from the placebo-treated group had to be re-admitted. The reasons for re-admission were: pain, vomiting, dehydration or poor oral intake (excluding bleeding). There were no statistically significant differences between the celecoxib- and placebo-treated groups for any of these reasons (p = 0.7).
Discussion
This study aimed to determine if a combination of paracetamol, Endone and a specific cyclooxygenase-2 inhibitor (celecoxib) would provide better analgesia following tonsillectomy than paracetamol and Endone alone. It was hoped that it would provide a better outcome by significantly reducing pain and adverse outcomes, and be associated with a low bleed rate. This study showed that celecoxib did not reduce the total intake of Endone or time taken to achieve a pain-free period, and there was no significant difference in pain, or number or type of bleeds during the post-tonsillectomy period. However, taking celecoxib was associated with significantly more vomiting.
The combination of paracetamol with NSAIDs (cyclooxygenase-2 inhibitors) has been shown many times to provide better analgesic efficacy and to exert an opioid-sparing effect, hence reducing the intake of opioids and the opioid-related side effects.Reference Salonen, Silvola and Kokki 12 – Reference Issioui, Klein, White, Watcha, Coloma and Skrivanek 14 For example, oral pre-medication administered 30–60 minutes before the induction of anaesthesia, with a combination of paracetamol (2 g) and celecoxib (200 mg) was shown to be highly effective in decreasing pain and improving patient satisfaction after ambulatory otolaryngological surgery (nasal and sinus surgery, tonsil and adenoid surgery, otological surgery, and head and neck surgery).Reference Issioui, Klein, White, Watcha, Coloma and Skrivanek 14 Thus, our apparently contradictory findings were of some surprise.
The addition of celecoxib did not significantly reduce pain at rest, when drinking or when eating. This could be because the combination of paracetamol (1 g four times a day) and celecoxib (200 mg twice a day), with Endone (5 mg), as a rescue analgesic, did not have any synergistic effects. Paracetamol is generally considered to be a weak inhibitor of prostaglandin synthesis and the in vivo effects of paracetamol are similar to those of cyclooxygenase-2 inhibitors.Reference Graham and Scott 15 It has been shown that paracetamol produces its analgesic activities through inhibition of the cyclooxygenase-2 pathway involved in prostaglandin synthesis, although the details of its action are still unclear.Reference Graham and Scott 15 Paracetamol has never been classified as a selective cyclooxygenase-2 inhibitor, yet its clinical effects are similar to those of selective cyclooxygenase-2 inhibitors such as celecoxib; hence, paracetamol has been described as ‘a selective COX-2 [cyclooxygenase-2] inhibitor’.Reference Graham and Scott 15
In addition, celecoxib in a 200 mg dosing is less effective than traditional NSAIDs used in a more common dose, hence its weak effect on relieving pain.Reference Rømsing and Møiniche 16 White concluded that 200 mg of celecoxib was equivalent to 2 g of acetaminophen (paracetamol) when administered before otolaryngological operations.Reference White 17 The analgesic efficacy of celecoxib is dose-related, with 400 mg being the currently recommended dose for acute pain prevention.
As the recommended dose for celecoxib is 400 mg per day for acute pain, 200 mg of celecoxib twice a day would seem to provide the required dosage; however, it may not be a strong enough analgesic agent when the total daily dose of celecoxib is divided into two separate 200 mg doses. In addition, the combination of 1 g of paracetamol four times day (which is equivalent to 100 mg of celecoxib four times a day) and 200 mg of celecoxib twice a day might have reached a ceiling effect, which we believe may be sub-therapeutic. According to Recart et al., NSAIDs are known to have a therapeutic ceiling effect with respect to analgesia, and thus these drugs may be less beneficial in reducing pain and opioid consumption after more extensive surgical procedures.Reference Recart, Issioui, White, Klein, Watcha and Stool 18 This was echoed by Schwartz, who described the therapeutic ceiling effect being the limiting factor associated with NSAIDs.Reference Schwartz 19 The therapeutic ceiling effect refers to the property of increasing doses of a given medication to have a progressively smaller incremental beneficial effect, until at some point the maximum beneficial effect has been reached and only the incidence and severity of adverse side effects increase.
Furthermore, the type of surgery may affect the efficacy of this combination of drugs; for example, in patients undergoing orthopaedic surgery, the combination of paracetamol and NSAIDs exerts an opioid-sparing effect and lower pain scores, but such an effect is not seen in patients undergoing soft tissue surgeryReference Salonen, Silvola and Kokki 12 such as tonsillectomy.
Pickering et al. conducted a double-blinded, placebo-controlled study of analgesia, comparing ibuprofen with rofecoxib (rofecoxib is an oral cyclooxygenase-2 inhibitor that has since been withdrawn over safety concerns) used in combination with paracetamol for analgesia following tonsillectomy in children.Reference Pickering, Bridge, Nolan and Stoddart 20 That study looked for an additive analgesic effect of the combination of rofecoxib and paracetamol. The results supported the idea that the combination of ibuprofen with paracetamol (but not rofecoxib) provided effective peri-operative analgesia in children. The addition of rofecoxib to paracetamol did not confer any additional analgesic benefit above paracetamol alone. This was a surprising finding which questions the role of cyclooxygenase-2 inhibitors for peri-operative analgesia.
The sites of action of both drugs may be relevant, as paracetamol inhibits brain cyclooxygenase, whereas rofecoxib inhibits both brain and peripheral cyclooxygenase. Hence, if both drugs were acting to inhibit the same brain site of cyclooxygenase, we could perhaps explain the observed lack of addictive effect (assuming that paracetamol is producing near maximal antagonism of brain cyclooxygenase).Reference Pickering, Bridge, Nolan and Stoddart 20
Schwartz published an article on peri-operative pain management, which mentioned that post-operative pain from dental, and oral and maxillofacial surgical procedures is largely mediated by its peripheral inflammatory component.Reference Schwartz 19 Centrally activated mechanisms also add to the overall perception of the painful stimulus. Hence, the management of pain should consider the factors necessary to reduce both the peripherally and centrally mediated processes that propagate pain.Reference Schwartz 19
Alternatively, it is possible that inducible cyclooxygenase-2 does not play a role in nociception in the early recovery period following tonsillectomy. In fact, Pickering et al. have suggested that central and peripheral cyclooxygenase-1 are involved in mediating early pain after tonsillectomy.Reference Pickering, Bridge, Nolan and Stoddart 20 Thus, using two fairly similar types of analgesic agent, celecoxib and paracetamol, which produce their analgesic effect through the same pathway of central cyclooxygenase inhibition, may not have yielded any additional benefits in conferring pain relief. This may explain why there was no significant decrease in the number of Endone tablets used during the post-operative period (as had been anticipated) because of the lack of additional analgesic effects of celecoxib. In fact, we found that the celecoxib-treated group took more Endone tablets than the placebo-treated group.
Tiippana et al. performed a study examining the effect of paracetamol treatment with or without dexamethasone treatment, versus cyclooxygenase-2 inhibitor (parecoxib and valdecoxib) treatment with or without dexamethasone treatment after laparoscopic cholecystectomy.Reference Tiippana, Bachmann, Kalso and Pere 21 That study showed no difference in pain intensity between the groups, and the effect of dexamethasone was similar in both the paracetamol and cyclooxygenase-2 inhibitor treated patients. However, more of the cyclooxygenase-2 inhibitor treated patients needed rescue medication on the 1st and 4th post-operative days compared to the paracetamol-treated patients. It is believed that visceral pain with involvement of the autonomic nervous system is an important factor following laparoscopic cholecystectomy. This may explain why this type of pain is more resistant to the analgesic effect of NSAIDs alone.Reference Tiippana, Bachmann, Kalso and Pere 21 It is perhaps not surprising that there were no statistically significant treatment group differences with regard to the day when patients were pain free and the day they returned to work or college. It is clear that the intake of celecoxib on top of regular paracetamol and Endone (as a rescue analgesic) did not hasten the patients’ return to normal activity.
With regard to the post-tonsillectomy side effects, the celecoxib group had significantly more vomiting, especially on days 9 and 10. This was in contrast to some other reports. For instance, Krishna et al. found that cyclooxygenase-2 inhibitors such as celecoxib had an improved adverse-effect profile.Reference Krishna, Hughes and Lin 22 In fact, Møiniche et al. reported that NSAIDs reduced the risk of post-operative nausea and vomiting.Reference Møiniche, Rømsing, Dahl and Tramèr 23 In addition, Iverson et al. determined that the use of a cyclooxygenase-2 inhibitor was associated with less post-operative nausea and vomiting because of the lower incidence of gastrointestinal irritation.Reference Iverson and Lynch 24 However, surgery-related factors that increase the incidence of post-operative nausea and vomiting include the site and duration of surgery. Otolaryngological and breast augmentation procedures have been linked to a higher incidence of post-operative nausea and vomiting.Reference Iverson and Lynch 24 Following a systemic review, McDaid et al. suggested that while paracetamol, NSAID and cyclooxygenase-2 inhibitor were all associated with reduced morphine consumption in the first 24 hours following surgery, only NSAIDs appeared to reduce morphine-related adverse effects.Reference McDaid, Maund, Rice, Wright, Jenkins and Woolacott 25 Hence, the increase in vomiting incidence observed on days 9 and 10 in the celecoxib group would most likely be due to the increased intake of the opioid analgesic Endone.
In this study, both treatment groups registered the highest numbers of side effects on post-operative day 3, which coincides with the day when the fibrin clot or eschar separates. This would explain why the pain and other associated side effects would be stronger or more frequent at this time following surgery. Secondary haemorrhage post-tonsillectomy is theorised to be the result of premature separation of the eschar from the tonsillar fossa.Reference Mösges, Hellmich, Allekotte, Albrecht and Böhm 26 – Reference Kim, Koo, Ahn, Lee and Kim 29 We did not expect any increase in numbers of bleeding episodes in the celecoxib group, as cyclooxygenase-2 inhibitors do not affect platelet aggregation and should lower the incidence of post-tonsillectomy bleeding.Reference Nikanne, Kokki, Salo and Linna 30 However, more of the patients in the celecoxib group experienced bleeding compared to the placebo group, with the celecoxib group exhibiting twice the number of minimal bleeds compared to the placebo group. The relatively high bleed rate reported in our study may be due to the fact that we categorised any bleeding post-surgery as a bleed, and all bleeds were recorded and subcategorised into the respective category, as outlined in Table III.
Few studies have reported higher post-tonsillectomy haemorrhage rates than ours, with the bleed rate typically falling between 7 and 10 per cent.Reference Stelter, Hempel, Berghaus, Andratschke, Luebbers and Hagedorn 8 , Reference Ranjit, Brett, Lu and Aw 31 However, Evans et al. performed a telephone interview, which revealed that 40 per cent of 60 patients experienced some post-tonsillectomy haemorrhage, but only 8.6 per cent of these incidents resulted in patient re-admission and operative intervention.Reference Evans, Khan, Young and Adamson 32 In another study, only patients who experienced blood actively flowing from the mouth for more than 1 minute were considered to have experienced significant bleeding; these events were recorded as post-tonsillectomy haemorrhages and included in their data.Reference Blakley 33 Sarny et al. performed a questionnaire-based study and found that the post-tonsillectomy haemorrhage rates reported in the literature differed considerably, with rates ranging from 0.1 to 40 per cent.Reference Sarny, Habermann, Ossimitz, Schmid and Stammberger 34 They concluded that haemorrhage rate is considerably higher than that assumed by investigating hospital records only, and is strongly related to the definition of post-operative bleeding and to the study design. Blomgren et al. found that 32.8 per cent of a mixed adult and paediatric population had experienced some degree of secondary haemorrhage following tonsillectomy.Reference Blomgren, Qvarnberg and Valtonen 35
Alhamarneh et al. performed a complete audit loop (an audit loop being the periodic performance of clinical audits after identifying appropriate issues, setting standards, measuring current practice against these standards, assessing recommendations, and implementing change) and concluded that adequate analgesia for the first week post-tonsillectomy is essential to keep the secondary haemorrhage rate within an acceptable range.Reference Alhamarneh, Raja and England 36
-
• Post-tonsillectomy pain can be severe and patients are discharged home with strong analgesics
-
• Cyclooxygenase-2 inhibitors (e.g. celecoxib) are newer, selective, non-steroidal anti-inflammatory drugs
-
• These have good analgesic properties, with minimal side effects (e.g. platelet dysfunction and gastrointestinal bleeding)
-
• Paracetamol, Endone and celecoxib did not provide better post-tonsillectomy analgesia than paracetamol and Endone alone
-
• Celecoxib did not reduce total Endone intake, or post-tonsillectomy pain duration or severity
-
• Celecoxib treatment resulted in significantly more vomiting
As our study was only conducted in the adult population, age may be a highly significant factor in the variability in reported secondary haemorrhage rates following tonsillectomy.Reference Mattos, Robison, Greenberg and Yellon 37 , Reference Walker and Gillies 38 We believe that factors such as inadequate analgesia, age of the study population, the under-reported ‘true’ post-tonsillectomy haemorrhage rate, and the ‘Hawthorne’ effect of being watched (wherein individuals modify or improve their behaviour in response to their awareness of being observed)Reference Blakley 33 contributed to the post-tonsillectomy haemorrhage rates reported in this study. Nevertheless, we found no significant difference in the re-admission rates between patients supplied with celecoxib (15 per cent) and those given placebo (10 per cent).
Conclusion
This study demonstrated that celecoxib usage did not reduce the need for narcotic analgesia post-tonsillectomy and was associated with an increased risk of vomiting.
Acknowledgements
We would like to thank: Dr Ashley Webb (anaesthetist); Dr Vicky Tobin, Dr Alexandra Rizzitelli and Ms Katrina Smith (research co-ordinators); Mr Ben Leung (pharmacy manager); Mdm Teresa Hennig (research pharmacist); Prof Bob Spychal and Ms Ebony Dejager (Department of Surgery); Mdms Lisa Waugh, Lesley Doyle, Lyndal Hogan and Leah Parsons (Waiting List Office); Mdms Janet Seitz, Marion Steele and Heather Walker (librarians); and the nurses in Medicentre, Elective Surgical Ward, Surgical Short Stay Unit, 4 G South, Surgical Services Suite, Theatre and Recovery. This study was fully funded by the Department of Surgery, Frankston Hospital.














