Introduction
Deep neck abscesses are serious infections; they may progress rapidly, causing significant morbidity in children.Reference Baldassari, Howell, Amorn, Budacki, Choi and Pena1 Approximately 20 per cent of these abscesses occur in the parapharyngeal space,Reference Amar and Manoukian2 which can lead to severe and potentially fatal complications such as mediastinitis, internal jugular vein thrombosis and carotid artery rupture.Reference Baldassari, Howell, Amorn, Budacki, Choi and Pena1 To prevent these dangerous complications, early and adequate diagnosis followed by surgical intervention for drainage are mandatory.Reference Coulthard and Isaacs3, Reference Page, Bauer and Lieu4
Two types of surgical drainage for parapharyngeal abscesses have been reported: the external neck approach and the intraoral approach.Reference Amar and Manoukian2 The latter is advocated for disease located medial to great vessels, and includes a procedure in which a needle is inserted through the lateral pharyngeal wall followed by an incision in the overlying mucosa. However, it is sometimes difficult to identify the exact location of the abscess via computed tomography (CT) imaging. Recent studies have described the use of image-guided drainage to augment the intraoral approach.Reference Cable, Brenner, Bauman and Mair5
The parapharyngeal space has also been approached using the intraoral approach combined with tonsillectomy.Reference Platzer, Brenner, Thumfart, Gunkel, Thumfart, Platzer, Gunkel, Maurer and Brenner6 However, the utility of this technique for parapharyngeal abscesses in paediatric patients has not been investigated. We suspected that this procedure should be utilised more often, specifically in paediatric patients with a medial parapharyngeal abscess.
Case presentations
The review board of Tohoku University Hospital approved publication of the following case reports.
Case one
A 7-year-old girl was admitted to the paediatric ward of a general hospital because of a 5-day history of left neck swelling and torticollis. Her white blood cell count was 23 500 cells/mm3, with a C-reactive protein level of 6.47 mg/dl. Computed tomography revealed an abscess in the left parapharyngeal space. Despite a course of antibiotics for 4 days, the patient's symptoms persisted without improvement, and she was referred to our department.
An abscess with a diameter of 4 cm was located medial to the great vessels of the neck and in the upper part of the parapharyngeal space (Figure 1). We decided to perform drainage surgery via an intraoral approach combined with tonsillectomy. The patient underwent emergency surgery under general anaesthesia that same day. Intratracheal intubation was maintained for 1 post-operative day because of the possibility of pharyngeal oedema. An oral diet was started on post-operative day 3. She was discharged 12 days after the operation.
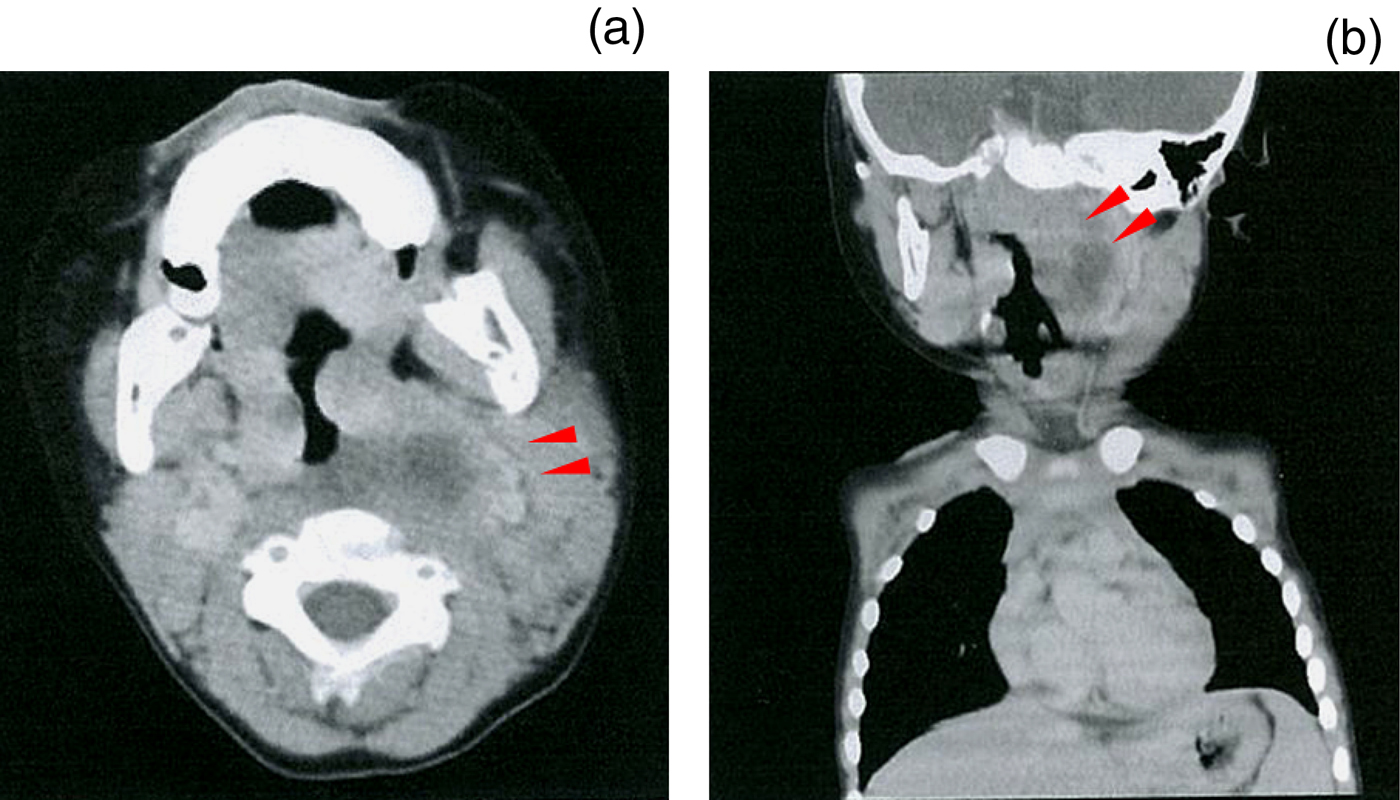
Fig. 1 (a) Pre-operative axial, enhanced computed tomography (CT) image of case one, demonstrating an abscess of the left parapharyngeal space (arrows). Note that the abscess is located medial to the internal carotid artery. (b) Coronal section of the enhanced CT scan. Note that the abscess (arrows) is close to the skull base.
Case two
A 2-year-old boy was admitted to the paediatric ward of a general hospital because of a 2-day history of left neck swelling and fever. His white blood cell count was 45 600 cells/mm3, with a C-reactive protein level of 13.6 mg/dl. Computed tomography revealed an abscess with a diameter of 3 cm in the left parapharyngeal space, and the patient was transferred to our hospital.
As the abscess was located medial to the great vessels of the neck and in the upper part of the parapharyngeal space (Figure 2), we decided to perform surgical drainage via the intraoral approach combined with tonsillectomy. The patient underwent surgery under general anaesthesia the next day. Intratracheal intubation was maintained for 3 post-operative days because of the possibility of pharyngeal oedema. An oral diet was started on post-operative day 4. The patient was discharged 7 days after the operation.

Fig. 2 (a) Pre-operative axial, enhanced computed tomography (CT) image of case two, demonstrating an abscess of the left parapharyngeal space (arrows). Note that the abscess is located medial to the internal carotid artery. (b) Coronal section of the enhanced CT scan. Note that the abscess (arrows) is close to the skull base.
Surgical procedure
In the above cases, we performed surgical drainage via the same intraoral approach. The whole procedure was carried out under surgical microscopy (Figure 3).

Fig. 3 (a) Schematic findings of the surgical procedure of intraoral drainage followed by ipsilateral tonsillectomy. Dotted lines indicate the extent of the abscess. (b) Microscopic view of the surgical procedure in case two, after draining of the parapharyngeal abscess (star).
First, a self-retaining mouth gag was inserted whilst the patient was under general anaesthesia, to aid tonsillectomy. We then performed tonsillectomy on the affected side. This was followed by blunt dissection in the muscularis of the tonsillar fossa. Specifically, a longitudinal 5 mm incision of the soft palate was made to expose the tonsillar fossa widely, giving access to the upper part of the parapharynx. The flaps of the layers of the muscularis were retracted laterally using catgut. Through blunt dissection of the connective tissue of the parapharyngeal space using curved Kelly forceps (Figure 3a), the presence of an enlarged lymph node with an abscess was confirmed. After confirming the presence of pus by needle puncture, we made a longitudinal incision in the abscess and performed further manual drainage (Figure 3b). Cervical compression specifically to the ipsilateral submandibular region was useful for evacuating the fluid from the abscess. Finally, we thoroughly cleaned the wound with saline and loosely sutured the opened tonsillar fossa so as not to prevent the pus from draining. After confirming there was no overt bleeding, the operation was completed.
A short video, available on The Journal of Laryngology & Otology website, demonstrates the surgical procedure performed for intraoral drainage followed by the ipsilateral tonsillectomy (Appendix 1).
Discussion
The intraoral approach with ipsilateral tonsillectomy is one operative procedure that can be used to access disease in the parapharyngeal space.Reference Platzer, Brenner, Thumfart, Gunkel, Thumfart, Platzer, Gunkel, Maurer and Brenner6 However, its use has rarely been described in paediatric cases of deep neck infection. The most frequent causes of a neck abscess are acute pharyngitis or cavities in adults, and lymphadenitis in children.Reference Sichel, Attal, Hocwald and Eliashar7, Reference Daya, Lo, Papsin, Zachariasova, Murray and Pirie8 In paediatric patients, a neck abscess is often contiguous with the pharyngeal cavity, because lymphadenitis of the parapharyngeal space progresses to a lymphatic abscess and neck abscess.
Intraoral drainage of a neck abscess may be more direct and more suitable in parapharyngeal abscess cases in which the abscess is located medial to the great vessels or close to the skull base.Reference Amar and Manoukian2, Reference Daya, Lo, Papsin, Zachariasova, Murray and Pirie8–Reference Hidaka, Ishida, Suzuki, Matsutani, Kobayashi and Takahashi10 In the former cases, an external approach requires a wider incision and increases the probability of damage to the carotid sheath. In the latter situation, it can be difficult to reach the abscess via an external approach, because the surrounding structure is shielded by the mandible.Reference Amar and Manoukian2, Reference Cable, Brenner, Bauman and Mair5
Cable et al. advocated an intraoral approach utilising image-guided technology, and stated that the intraoral approach without image guidance can be time-consuming, risky and frustrating, despite the use of CT data.Reference Cable, Brenner, Bauman and Mair5 However, intra-operative image-guided systems are expensive and may be available only in referral hospitals. In addition, surgical procedures for deep neck infections are usually performed as after-hours emergency procedures, without the support of radiologists.
Recently, we reported the usefulness of endoscopic drainage for abscesses located in the masticator space.Reference Hidaka, Ishida, Suzuki, Matsutani, Kobayashi and Takahashi10 In addition, Lee et al. reported on a transnasal endoscopic approach followed by adenoidectomy.Reference Lee, Lee and Chen11 This procedure would also be helpful for a parapharyngeal abscess near the skull base, which can alternatively be accessed through the extremely limited nasal space (even more limited in paediatric patients).
The intraoral approach combined with tonsillectomy, as described here, can help overcome these limitations. This procedure is performed under surgical microscopy to delineate structures deep to the musculature of the lateral pharyngeal wall. Although transluminal echography might also be useful, performing the procedure under surgical microscopy is advantageous because it enables one to record deep surgical structures more clearly, allowing one to share the findings with other medical staff. Other than obviating the need for skin incision, intraoral drainage for the treatment of a parapharyngeal abscess contributes to decreases in surgery time, length of post-operative antibiotics course and hospitalisation time, and a reduction in the use of anaesthesia when compared with an external approach.Reference Amar and Manoukian2
To our knowledge, no previous reports have addressed the use of surgical microscopy to aid access to the parapharyngeal space. The procedure reported herein, performed under surgical microscopy, was specifically helpful in accessing these challenging spaces.
Conclusion
Intraoral drainage combined with tonsillectomy in children with a parapharyngeal abscess resulted in a good post-operative course without complications. When compared with an external approach, intraoral drainage performed under surgical microscopy contributes to a reduced risk of complications, and enables the surgical findings to be shared with other medical staff. Furthermore, the post-operative wound is not visible. Therefore, intraoral drainage combined with tonsillectomy represents a good option for the management of paediatric parapharyngeal abscesses.
Acknowledgement
We thank Dr Yusuke Takata for the illustration shown in Figure 3a.
Appendix 1. Supplementary video material
A short video (complementary to Figure 3) demonstrating the surgical procedure performed for intraoral drainage followed by the ipsilateral tonsillectomy is available online at The Journal of Laryngology & Otology website, at http://youtu.be/M9WebXTJ2DY.





