Introduction
Despite tonsillectomy procedures being performed, in their truest form, as early as 1906 and the high frequency at which they are performed worldwide today, considerable controversy remains regarding which technique is best to use for optimum efficacy and lowest morbidity.Reference Moore1–Reference Albright, Duncan, Smerica and Edmonds3
Traditional tonsillectomy is defined as a procedure that completely removes the palatine tonsil including its capsule by dissecting the peritonsillar space between the tonsil capsule and the muscular wall.Reference Baugh, Archer, Mitchell, Rosenfeld, Amin and Burns4 Consequently, the underlying pharyngeal muscles, nerve endings and larger extracapsular blood vessels are left exposed and vulnerable to inflammation, infection and bleeding despite ligation or electrocautery.Reference Kim, Kwon, Lee and Yoon5,Reference Lee, Lee, Hong, Yu, Lee and Chun6 While the efficacy is apparent, especially where the indications significantly affect quality of life, the complications of traditional tonsillectomy, including throat pain, poor oral intake and dehydration, intra-operative and post-operative haemorrhage, and tonsil regrowth, are considerable concerns.Reference Kim, Kwon, Lee and Yoon5,Reference Hadjisymeou, Modayil, Dean, Jonas and Tweedie7
In an attempt to reduce the potential complications of traditional tonsillectomy, many different instruments and techniques have been used and novel technologies considered.Reference Elbadawey, Hegazy, Eltahan and Powell8 The concept of intracapsular tonsil dissection, described as early as the first century AD by Aulus Cornelius Celsus, was revisited by Koltai et al. in 2003.Reference Koltai, Solares, Koempel, Hirose, Abelson and Krakovitz9 The technique, also referred to as tonsillotomy, subtotal tonsillectomy and partial tonsillectomy, involves the removal of a variable volume of tonsil tissue while leaving the tonsil capsule intact.Reference Moore1,Reference Koltai, Solares, Koempel, Hirose, Abelson and Krakovitz9 Sparing the capsule prevents the exposure of the underlying pharyngeal musculature and protects the larger diameter blood vessels and nerve endings underlying the capsule, which acts as a biological dressing.Reference Lee, Lee, Hong, Yu, Lee and Chun6,Reference Amin and Lakhani10 Proponents of the technique cite equivocal outcomes in sleep-disordered breathing, with reduced morbidity including lowered rates of post-operative haemorrhage and pain as well as quicker return to normal diet and activity.Reference Hoey, Foden, Hadjisymeou Andreou, Noonan, Chowdhury and Greig11–Reference Walton, Ebner, Stewart and April14
An array of terms is used interchangeably when referring to the intracapsular tonsillectomy procedure, as outlined above. However, while the basic surgical principle of removing tonsil tissue and leaving the lateral fibrous capsule intact is common to all, vast differences exist with regard to the volume of tonsil tissue that is removed during intracapsular tonsillectomy procedures.Reference Blair, Booth and Baugh15 This in turn has contributed to the variability in efficacy and, more importantly, regrowth and recurrence rates, which remain considerable deterrents to the procedure gaining favour.Reference Rubinstein and Derkay16–Reference Celenk, Bayazıt, Yılmaz, Kemaloglu, Uygur and Ceylan18
Hoping to standardise the nomenclature, Windfuhr and Werner outlined two concepts in 2013 in relation to attempting to reduce the size of the tonsils using intracapsular dissection techniques.Reference Windfuhr and Werner19 The first was referred to as class 1 tonsillotomy, where the chosen instrument cuts through the tonsil tissue and removes only the protruding parts of the tonsil medial to the faucial pillars. The second is referred to as class 2 tonsillotomy: this is subtotal, intracapsular or partial tonsillectomy where removal of approximately 90 per cent of the tonsil from the medial to lateral side is aimed for with preservation of only a sliver of tonsil tissue as a protective layer along the inner surface of the capsule.Reference Windfuhr and Werner19
Since its recent resurrection, global interest and widespread publications have explored whether intracapsular tonsillectomy could represent the ideal surgical technique we have been searching for.Reference Albright, Duncan, Smerica and Edmonds3,Reference Kim, Kwon, Lee and Yoon5,Reference Amin and Lakhani10,Reference Walton, Ebner, Stewart and April14,Reference Sakki, Mäkinen, Roine and Nokso-koivisto20 Results pertaining to safety and efficacy of intracapsular tonsillectomy have been promising but have left a few areas of uncertainty and concern. Although there is mounting evidence for the use of intracapsular tonsillectomy in the management of sleep-disordered breathing in children, there is still a dearth of information and ongoing debate surrounding its use, specifically in recurrent infections as well as in adults.Reference Zhang, Zhong, David and Cervin12,Reference Wang, Fu, Feng, Guan and Yin13,Reference Blackshaw, Springford, Zhang, Wang, Venekamp and Schilder21
With this study, we aimed to evaluate whether a change in surgical technique, from extracapsular to intracapsular tonsillectomy (class 2) using Coblation™ and with a single surgeon has had an impact on the rate of post-operative haemorrhage amongst both children and adults, across all indications in a community-based ENT practice.
Materials and methods
Data collection
We retrospectively analysed the files of all patients who underwent tonsillectomy (extracapsular or intracapsular), irrespective of age, by a single ENT surgeon at a private healthcare facility between February 2013 and July 2019.
It is important to note that the two arms of the study did not run concurrently, and patients were not stratified in any way. At the onset of the study period, extracapsular tonsillectomy was performed in 379 consecutive cases between February 2013 and October 2016. Subsequently, on reviewing the literature pertaining to intracapsular tonsillectomy and its proposed benefits, this technique was adopted and performed in 351 consecutive patients between October 2016 and July 2019.
Data including age, gender, indication for surgery, and the occurrence of post-operative bleeding requiring admission or surgical intervention were collected and analysed. Patients were further stratified by age into 3 groups: 3 years old or younger, 3–18 years, and 18 years or older. The indications for surgery were classified as recurrent infection, sleep-disordered breathing, a combination of the two or other indications, which included tonsilloliths, halitosis, suspected malignancy or tonsillar asymmetry.
The study was approved for publication by the South African Medical Association's Research and Ethics Committee (3 September 2020).
Data analysis
SPSS® statistical software (2019) was used to calculate the descriptive and analytical results of the non-parametric data. The Mann–Whitney U test was used to compare age group stratification and either Pearson chi-square or Fisher's exact statistics, where appropriate, were used in all other analyses. Significance was set at a p-value of 0.05.
Surgical technique
Extracapsular tonsillectomy was performed following standardised techniques using CoblationTM technology. When intracapsular tonsillectomy was performed, the aim was removal of tonsil tissue as close to the capsule as possible. As outlined earlier, this has also been described as a class 2 or complete intracapsular tonsillectomy.Reference Albright, Duncan, Smerica and Edmonds3,Reference Windfuhr and Werner19
CoblationTM technology uses radiofrequency energy and saline to produce a plasma field at the end of a hand held wand; this divides the molecular bonds within tissues reducing them to low molecular weight gases and water that is then aspirated into the suction port at the end of the device wand.Reference Joshi and Carney22 Far less thermal damage is imparted to the surrounding tissues by CoblationTM when compared with other conventional devices used for performing tonsillectomy procedures because it uses relatively low temperatures of 60–70 degrees Celsius.Reference Joshi and Carney22
In the study, the EVac 90 Xtra HP wand (Smith and Nephew, Memphis, USA) was used to perform all procedures.
Results
In total, 730 patients were included in the study. The extracapsular tonsillectomy cohort included 379 patients and the intracapsular tonsillectomy cohort included 351 patients. All patients were followed up for at least 12 months post-operatively (range, 19–83 months).
Age analysis
There was no significant difference between the mean ages in the extracapsular tonsillectomy and intracapsular tonsillectomy groups. Further age comparisons are shown in Table 1.
Table 1. Age comparison analysis

Gender
Within the total study group population, 57.4 per cent were male (n = 419) and 42.6 per cent were female (n = 311). Males comprised 61.5 per cent (n = 233) of the extracapsular tonsillectomy group and 53.0 per cent (n = 186) of the intracapsular tonsillectomy group, and females made up 38.5 per cent (n = 146) and 47.0 per cent (n = 165) of the extracapsular tonsillectomy and intracapsular tonsillectomy groups, respectively.
Adenoidectomy
A concurrent adenoidectomy was performed in 73.7 per cent (n = 280) of extracapsular tonsillectomy group patients compared with 68.9 per cent (n = 243) in the intracapsular tonsillectomy group (p = 0.978).
Surgical indications
A significant increase in surgery performed for sleep-disordered breathing was found in the intracapsular tonsillectomy group over time (p = 0.029). Figures 1 and 2 illustrate the breakdown of surgical indications within the two groups studied.

Fig. 1. Indications for surgery for the extracapsular tonsillectomy cohort.
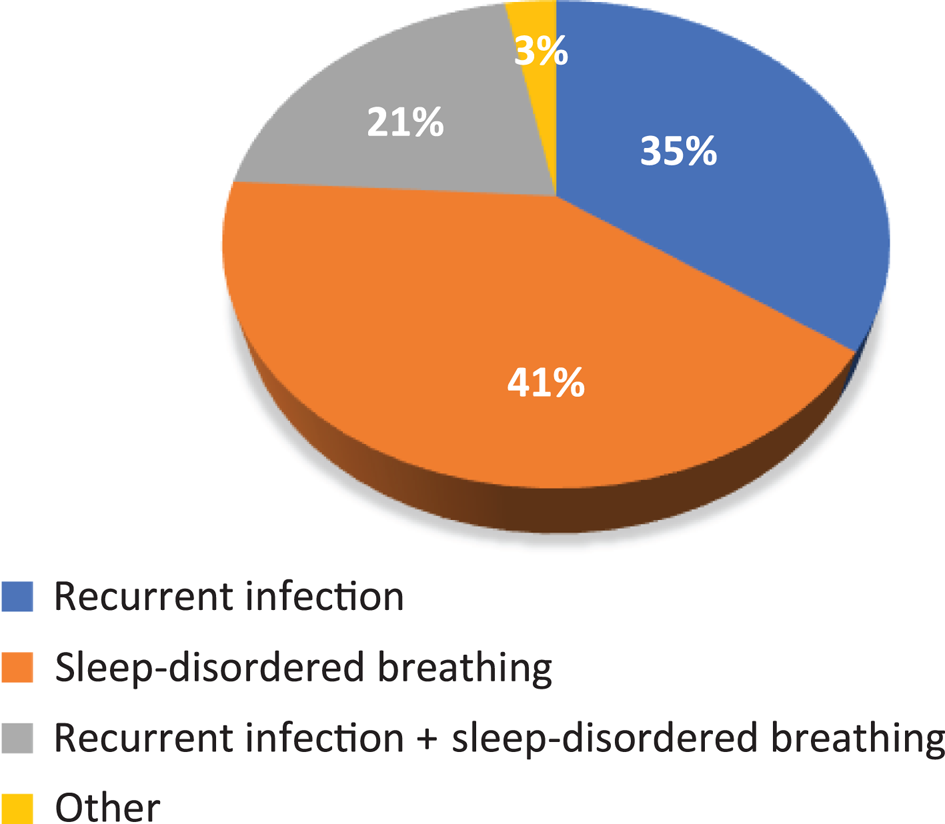
Fig. 2. Indications for surgery for the intracapsular tonsillectomy cohort.
Post-operative haemorrhage
Overall, a significant reduction in post-operative haemorrhage rate was observed when changing from the extracapsular (2.1 per cent; n = 8) to intracapsular (0.3 per cent; n = 1) technique (p = 0.025). We also noted age of 18 years or older to be an independent risk factor for post-operative haemorrhage (p = 0.01). Further analysis of post-operative haemorrhage by age and technique can be seen in Table 2.
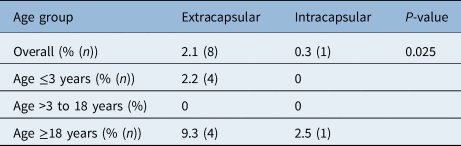
Table 2. Post-operative haemorrhage rates by age

We further evaluated characteristics of patients who experienced post-operative haemorrhage in an attempt to identify if any risk factors could be isolated. Male gender and the indication of recurrent infection appear to represent an increased risk for post-operative haemorrhage. However, because of small numbers, no significance could be drawn. The data pertaining to patients who experienced post-operative haemorrhage are presented in Table 3.
Table 3. Characteristics of patients experiencing post-operative haemorrhage

Revision surgery
One adult patient required revision surgery following a peritonsillar abscess developing six months after intracapsular tonsillectomy (0.28 per cent).
Discussion
Overall post-operative haemorrhage safety
Overall, we found CoblationTM intracapsular tonsillectomy to be safer than extracapsular tonsillectomy with regards to post-operative haemorrhage (0.28 vs 2.11 per cent; p = 0.025). This safety benefit was also evident in a recent study of similar design and technique to ours, which reported a 0 per cent bleeding rate using CoblationTM intracapsular tonsillectomy in 783 paediatric patients compared with 1.4 per cent using extracapsular tonsillectomy.Reference Albright, Duncan, Smerica and Edmonds3 If we excluded adults (patients 18 years or older) in our cohort, we also noted a 0 per cent bleeding rate amongst paediatric patients undergoing intracapsular tonsillectomy.
Attard and Carney, in their study of 608 paediatric patients, reported an 8.3 and 1.8 per cent post-operative haemorrhage rate for extracapsular tonsillectomy and intracapsular tonsillectomy, respectively.Reference Attard and Carney23 Using a modification of Stammberger's grading system, they also evaluated degrees of bleeding and found, in addition to higher rates, a significantly greater severity of bleeds in the extracapsular tonsillectomy group compared with the intracapsular tonsillectomy cohort.Reference Attard and Carney23
Similarly, Duarte et al. found that 88.2 per cent of all post-operative haemorrhage occurred in their extracapsular tonsillectomy group compared with only 11.8 per cent who had undergone intracapsular tonsillectomy.Reference Duarte, Liu and Shapiro24
The systematic review by Zhang et al. demonstrated a 79 per cent reduction in secondary haemorrhage occurring in intracapsular tonsillectomy vs extracapsular tonsillectomy.Reference Zhang, Zhong, David and Cervin12 The meta-analysis by Kim et al. showed a reduction in the risk of post-operative haemorrhage by 56 per cent compared with extracapsular tonsillectomy. Wang et al., in a meta-analysis, reported a risk ratio of secondary post-operative haemorrhage of 0.28, significantly favouring intracapsular tonsillectomy.Reference Kim, Kwon, Lee and Yoon5,Reference Wang, Fu, Feng, Guan and Yin13
Safety in the young paediatric subgroup
Historically, children younger than 36 months of age have been considered high risk for complications following traditional tonsillectomy, with authors citing increased rates of dehydration and airway complications necessitating overnight hospitalisation.Reference Bent, April, Ward, Sorin, Reilly and Weiss25 In response, the American Academy of Otolaryngology–Head and Neck Surgery's Paediatric Otolaryngology Committee recommended in 1996 that all children younger than three years of age undergo tonsillectomy with or without adenoidectomy in an appropriate overnight facility.Reference Bent, April, Ward, Sorin, Reilly and Weiss25 However, the need to hospitalise all young children undergoing adenotonsillectomy remains controversial.Reference Mitchell26 Furthermore, these risks may also influence paediatricians and surgeons to consider delaying the procedure until the child is older, in an attempt to reduce the dangers. In the scenario of sleep-disordered breathing, a delay in airway management could prove detrimental to the child's overall health and development.
In this study, both cohorts comprised a large number of patients 36 months of age or younger (extracapsular tonsillectomy, 42.7 per cent, n = 162; intracapsular tonsillectomy, 37.0 per cent, n = 130). In this subgroup of patients, intracapsular tonsillectomy emerged as a safer alternative to extracapsular tonsillectomy (0 per cent intracapsular tonsillectomy vs 2.6 per cent extracapsular tonsillectomy) with regards to post-operative haemorrhage (p = 0.090).
The study by Bent et al. also demonstrated safety of intracapsular tonsillectomy in children less than 36 months old and challenged the need for overnight admission in their study.Reference Bent, April, Ward, Sorin, Reilly and Weiss25 They reported a post-operative haemorrhage rate of 0 per cent as well as the additional morbidity advantages of intracapsular tonsillectomy in this age group and demonstrated suitability of this previously presumed high-risk group for out-patient ambulatory surgery.Reference Bent, April, Ward, Sorin, Reilly and Weiss25
Safety in adults
In comparing patients younger and older than 18 years of age, there was a significantly higher risk of post-operative haemorrhage in patients over the age of 18, irrespective of technique (p = 0.01). In patients 18 years or older in the intracapsular tonsillectomy group, this rate was found to be 3 times lower when compared with the extracapsular tonsillectomy group (2.8 per cent intracapsular tonsillectomy vs 9.1 per cent extracapsular tonsillectomy). However, as with the subgroup aged three years or younger, no statistical significance could be reached, possibly because of the sample size.
A recent systematic review by Amin and Lakhani included 9 randomised, controlled trials encompassing 319 adults demonstrating a statistically significant reduction in the rate of secondary post-operative haemorrhage with intracapsular tonsillectomy and an almost 50 per cent risk reduction compared with the extracapsular tonsillectomy group. The authors recommended intracapsular tonsillectomy as a safer alternative to tonsillectomy in adults.Reference Amin and Lakhani10
Our study was able to demonstrate improved safety of intracapsular tonsillectomy in both paediatric and adult populations, unlike the vast majority of publications which feature paediatric populations only. We are, at this time, unaware of any other publication that has studied the safety of intracapsular tonsillectomy against extracapsular tonsillectomy in both adults and children using CoblationTM technology for both procedures, thereby facilitating direct comparison.
Indications
Indications for performing tonsillectomy procedures have also been fraught with controversy over the years. Current guidelines by The American Academy of Otolaryngology (updated in 2019) include recurrent throat infections, obstructive sleep-disordered breathing and other clinical scenarios where comorbid conditions may benefit from the procedure, such as hyperactivity, enuresis, growth retardation, asthma, and antibiotic allergy or intolerance.Reference Mitchell, Archer, Ishman, Rosenfeld, Coles and Finestone27
The use and efficacy of intracapsular tonsillectomy has been well established for the indication of sleep-disordered breathing in the paediatric population and more recently in the adult population.Reference Amin and Lakhani10–Reference Wang, Fu, Feng, Guan and Yin13
In this study, we included sleep-disordered breathing (22.69 per cent, extracapsular tonsillectomy; 40.74 per cent, intracapsular tonsillectomy), recurrent infections (44.06 per cent, extracapsular tonsillectomy; 35.33, per cent intracapsular tonsillectomy) and a combination of these (22.69 per cent, extracapsular tonsillectomy; 21.37 per cent, intracapsular tonsillectomy) as the major indications to undertake surgery.
As has been reported by other authors, we found an increase in surgical procedures performed for sleep-disordered breathing over time.Reference Sakki, Mäkinen, Roine and Nokso-koivisto20 This increase is perhaps attributable to an increased awareness around the entity of sleep-disordered breathing and its associated morbidity amongst our referring practitioners.Reference Sakki, Mäkinen, Roine and Nokso-koivisto20
With the numbers too low to draw any significant conclusion, we were unable to demonstrate any significance with regards to safety of either procedure within the stipulated indications. However, we believe that the overall low rate of post-operative haemorrhage in the intracapsular tonsillectomy group (n = 1, 0.28 per cent), where the surgery was performed for both infective and obstructive symptoms, implies that the procedure is safe irrespective of the underlying indication and may be undertaken in patients with obstructive as well as infective symptomatology.
A recent publication evaluating whether intracapsular tonsillectomy could also be considered for recurrent infection in addition to sleep-disordered breathing demonstrated that CoblationTM intracapsular tonsillectomy was a safe and effective technique for both indications in the paediatric population, in addition to lowered mean overall T14 questionnaire and infective scores over a 13-month post-operative follow-up period.Reference Varadharajan, Caton, Faulkner and Khemani28 In their prospective study of 500 paediatric patients, Hoey and Foden also reported symptomatic improvements with intracapsular tonsillectomy for both obstructive and infective domains that were equivocal to figures published for extracapsular tonsillectomy.Reference Hoey, Foden, Hadjisymeou Andreou, Noonan, Chowdhury and Greig11
• Post-operative haemorrhage is a significant complication of traditional extracapsular tonsillectomy
• Intracapsular tonsillectomy has recently been revisited in an attempt to reduce complications
• This study compared post-operative haemorrhage rate between extracapsular and intracapsular tonsillectomy procedures
• A significant reduction in post-operative haemorrhage rate was observed when changing from extracapsular to intracapsular tonsillectomy
• This study has demonstrated CoblationTM intracapsular tonsillectomy to be a safe and effective surgery for all ages and indications
With regards to adults, a prospective randomised, controlled trial found extracapsular tonsillectomy and intracapsular tonsillectomy to be equally effective in reducing disease symptoms amongst patients with recurrent or chronic tonsillitis.Reference Bender, Blassnigg, Bechthold, Kral, Riccabona and Steinbichler29
Addressing criticisms
Much of the apprehension surrounding intracapsular tonsillectomy stems from concerns regarding infection in the tonsil remnant and its regrowth potential with consequent recurrence of sleep-disordered breathing, necessitating revision surgery or completion of extracapsular tonsillectomy.Reference Wang, Fu, Feng, Guan and Yin13
Difficulty in the interpretation of published results surrounding these negative outcomes again lies in the heterogeneity of procedures performed under the broad umbrella of intracapsular tonsillectomy (tonsillotomy or class 1 procedure vs intracapsular tonsillectomy class 2 procedure) as well as the extensive range of instrumentation used.Reference Windfuhr and Werner19 As a result of the disparity, published revision rates range between 0.7 per cent to 11.9 per cent.Reference Hoey, Foden, Hadjisymeou Andreou, Noonan, Chowdhury and Greig11,Reference Celenk, Bayazıt, Yılmaz, Kemaloglu, Uygur and Ceylan18,Reference Attard and Carney23,Reference Sorin, Bent, April and Ward30,Reference Eviatar, Kessler, Shlamkovitch, Vaiman, Zilber and Gavriel31
Meta-analyses by Kim et al. and Gorman et al. as well as the systematic review by Walton et al. found no difference in the recurrence of obstructive symptoms between intracapsular tonsillectomy and extracapsular tonsillectomy groups.Reference Kim, Kwon, Lee and Yoon5,Reference Walton, Ebner, Stewart and April14,Reference Gorman, Ogston and Hussain32 Post-operative recurrent tonsillitis and pharyngitis were also not found to be any greater when using intracapsular tonsillectomy.Reference Kim, Kwon, Lee and Yoon5,Reference Walton, Ebner, Stewart and April14
We also believe that the distinction between regrowth and symptom recurrence is crucial. With a follow up period of 19 to 50 months in the intracapsular tonsillectomy group, only one revision surgery (completion tonsillectomy) was performed six months after intracapsular tonsillectomy because of the formation of a small abscess that was likely a result of obstructed Weber glands in the superior tonsillar pillar.Reference Klug, Rusan, Fuursted and Ovesen33
We attribute our low revision rate (0.28 per cent) to the intracapsular complete technique as well as comprehensive communication and education around regrowth for both our patients and referring practitioners. The importance thereof is seen in the large study by Hultcrantz et al. encompassing 24 000 patients, where 38 per cent of patients undergoing intracapsular tonsillectomy returned to snoring in 6 years. However, none of the parents regarded this to be problematic, and no revision surgery was therefore necessary.Reference Hultcrantz, Ericsson, Hemlin, Hessén-Söderman, Roos and Sunnergren34
Cost implications
Modifications of surgical technique or instrumentation that reduce rates of complications have knock on effects on resources, quality of life, patient care and ultimately cost effectiveness of the procedure. Unscheduled visits to the surgeon, readmission for observation and, in worst case scenarios, return to the operating theatre for haemorrhage control not only adds to increased financial burden but also adds socioeconomic and health resource burdens that impact the patient and, in the case of a minor, the caregiver as well.Reference Stucken, Grunstein, Modi, Waldman and Ward35
When comparing cost effectiveness, studies have found intracapsular tonsillectomy to be more favourable than extracapsular tonsillectomy because of shorter operating and recovery room times, lower recontact and readmission rates, reduction in secondary bleeding and the need for repeated operating theatre visits as well as a decrease in the number of days off work for the carer.Reference Zhang, Zhong, David and Cervin12,Reference Stucken, Grunstein, Modi, Waldman and Ward35,Reference Baik and Brietzke36 These financial, social and resource benefits would however need to be balanced against the cost of the device wand and revision surgery rates.
The South African context
South Africa has an interesting and somewhat unique healthcare system comprising a private sector, where patients pay monthly premiums to visit independently owned facilities, and a public sector, which caters for a large proportion of the population in government owned and run facilities. Significant disparity in patient numbers and available resources exists between the two sectors. According to the General Household Survey by Statistics South Africa for 2018, less than 17 per cent of the population are able to afford private healthcare, leaving approximately 45 million people (82 per cent of the population) dependent on public healthcare.Reference Africa37
Conventionally, extracapsular tonsillectomy has been practised and taught to training ENT surgeons almost exclusively within the public sector. The complications associated with this technique, as highlighted above, prove worrisome in this community of patients, given the great distances patients travel in order to seek medical and surgical care and the financial and economic restrictions to being able to travel back to the healthcare facility should an emergency such as post-operative haemorrhage arise.
This study incorporates data that directly compares intracapsular and extracapsular tonsillectomy techniques for safety, specifically with regards to post-operative haemorrhage. Furthermore, we were able to quantify and compare these rates for both the paediatric and adult population encompassing all surgical indications.
We believe that evolution of traditional tonsillectomy techniques in the public sector could be driven by evidence from the private sector, ultimately leading to safer and improved practice and care of our patients within the global healthcare system, both in private and public domains.
Conclusion
This study has demonstrated CoblationTM intracapsular tonsillectomy to be a safe and effective surgical procedure in both adults and children across all indications, with a low risk of bleeding and revision surgery.
Competing interests
None declared