Introduction
Tumours of the parotid gland are uncommon, with benign and malignant tumours comprising around 3 per cent of all head and neck tumours.Reference Speight and Barrett1 Resection of the facial nerve in conjunction with removal of the tumour is sometimes required, leading to significant morbidity and impaired quality of life (QoL).Reference Thielker, Grosheva, Ihrler, Wittig and Guntinas-Lichius2 In addition to facial nerve dysfunction, many patients suffer xerostomia, sensory impairment and hearing loss.Reference Erkan, Yavuz, Ozer, Ozer and Ozluoglu3
For over a decade, we have advocated for immediate reconstruction of the facial nerve after radical parotidectomy to improve facial aesthetics, function and to protect the eye. The reconstruction for this group of patients involves restoring contour, midface reanimation and facilitating eye closure with upper lid weighting and lower lid support.Reference Ch'ng, Ashford, Gao, McGuinness and Clark4 Both static and dynamic reanimation procedures are offered, depending on the age, comorbidity and prognosis of the patient.Reference Ch'ng, Ashford, Gao, McGuinness and Clark4,Reference Hasmat, Lovell, Suaning, Low and Clark5 Rapid healing to facilitate adjuvant therapy and sufficient long-term tissue volume are other important components in the treatment algorithm because most patients will receive either radiotherapy alone or concurrent chemoradiotherapy.Reference Hasmat, Lovell, Suaning, Low and Clark5
The negative impact of facial nerve palsy on the patient's QoL is well documented;Reference Leong and Lesser6,Reference Fu, Bundy and Sadiq7 however, there are limited data on QoL for patients who have undergone this operation with primary facial nerve reanimation procedures. Furthermore, patients undergoing radical parotidectomy have a unique combination of functional and aesthetic problems, and there are no specific QoL measures available for this group of patients. We often assume that objective improvement in function after reconstructive surgery should result in improved QoL. The purpose of this study was to ascertain the QoL of patients undergoing radical parotidectomy who underwent primary facial reanimation, while using patients who underwent limited superficial parotidectomy with preservation of the facial nerve (limited superficial parotidectomy) as a control group.
Materials and methods
Study design
Ethical approval for this study was obtained from Sydney Local Health District Ethics Committee (protocol number: X10-0261). The Sydney Head and Neck Cancer Institute database (at Chris O'Brien Lifehouse and Royal Prince Alfred Hospitals, Sydney, Australia) showed 1683 patients who underwent parotidectomy between 1995 and 2015. Of this group, we identified 52 patients, half of whom underwent radical parotidectomy with primary facial nerve reanimation (radical parotidectomy) and half of whom underwent limited superficial parotidectomy with preservation of facial nerve (limited superficial parotidectomy). These patients were age and sex matched. Patients were initially contacted by telephone to inform them of the study, and questionnaires were subsequently sent to patients through the post. A follow-up telephone call was made four weeks later; if no response was received, another follow-up letter was sent.
All patients who underwent radical parotidectomy received primary dynamic facial nerve reanimation procedures as well as lower lid reconstruction procedures, with most receiving upper lid loading. Age, gender, complications, pathological features and treatment details were recorded.
Outcome measures
Patients were asked to complete two questionnaires to measure their QoL: the validated University of Washington Quality of Life Questionnaire and the Parotidectomy Specific Quality of Life outcomes questionnaire.
The University of Washington Quality of Life QuestionnaireReference Hassan and Weymuller8 is a self-administered questionnaire that focuses on 12 domains (pain, appearance, activity, recreation, swallowing, chewing, speech, shoulder function, taste, saliva, mood and anxiety), based on the patient's experience over the last 7 days. The ‘importance rating’ asks the patient to rate which domain has been most important to them during the preceding seven days. There are also three global questions at the end, asking about how patients feel, their health-related QoL and their overall QoL. The scoring for the University of Washington Quality of Life Questionnaire is scored in a range of 0–100, where 100 is the best QoL the patient experiences. This allows for domain-specific QoL scoring, with specific QoL scoring compared with the patient's pre-cancer life, health and overall sense of wellbeing.
The Parotidectomy Specific Quality of Life was designed and developed in our institution,Reference Lee9 specifically to determine the QoL following parotidectomy, and it has two parts. The first measures the severity of symptoms, and the second measures the degree of interference of symptoms with normal functioning. The first part has 12 domains, with 40 questions to be scored from 0 (no problems) to 10 (worst imaginable), with special emphasis on symptoms related to parotid surgery, neck dissection, hearing and facial nerve dysfunction. The second part measures interference with physical, mental and social activities through 12 questions scored from 0 to 10. Therefore, the highest possible score is 520 (Appendix 1).
Statistical analysis
Data were analysed using SPSS® statistical software (version 15.0). Non-parametric data were analysed using the Mann–Whitney U test. For the importance rating, Fisher's exact test was used to determine statistical significance. Differences that were associated with a chance of probability of 0.05 or less were considered statistically significant.
Results
Demographic and treatment characteristics
Of the 52 patients, 29 (56 per cent) completed and returned the questionnaires. Of these patients, 14 patients received limited superficial parotidectomy with preservation of the facial nerve (limited superficial parotidectomy), and 15 received radical parotidectomy. Median follow up in the cohort was 7.3 years (range, 2–19.2 years), with the follow up in both groups being comparable. Clinical characteristics of both cohorts are shown in Table 1. The mean age was 69 years, and there was a minor female predominance (55 per cent). Notably, all patients undergoing radical parotidectomy had malignant tumours and received adjuvant radiotherapy, with or without chemotherapy compared with 57 per cent in the limited superficial parotidectomy group.
Table 1. Clinical characteristics of the cohorts in the radical parotidectomy and limited superficial parotidectomy groups

*n = 14; †n = 15; ‡p < 0.05 was considered statistically significant. SD = standard deviation
Primary facial nerve reanimation procedures
All patients who had radical parotidectomy (n = 15) also underwent reconstruction with primary facial reanimation procedures, as shown in Table 2. Of these, 12 (80 per cent) were dynamic procedures. The driver nerves used were facial nerve (42 per cent), masseteric nerve (33 per cent) or both (25 per cent). Nerve grafting was performed in 8 patients (53 per cent), gold weight insertion was performed in 10 patients (67 per cent) and lower lid reconstruction was performed in 12 patients (80 per cent).
Quality of life measurement
University of Washington Quality of Life Questionnaire
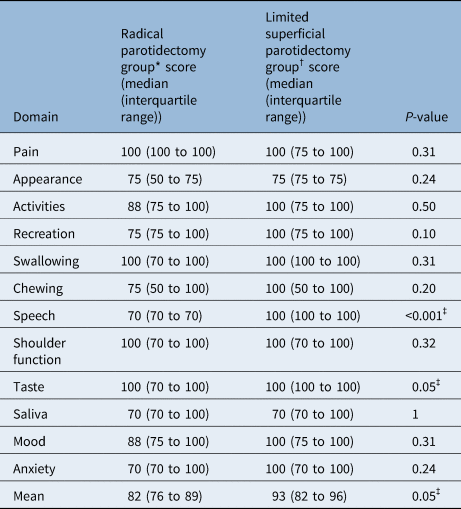
As a baseline comparison, it is important to note that all radical parotidectomy patients had adjuvant radiotherapy with or without chemotherapy; however, only 57 per cent of limited superficial parotidectomy patients had any adjuvant therapy. When comparing the two groups, those undergoing limited superficial parotidectomy with preservation of facial nerve (limited superficial parotidectomy) and radical parotidectomy, similar outcomes were noted in both groups with the University of Washington Quality of Life Questionnaire scale in most domains (Table 3), including the domains of pain, appearance, activities, recreation, swallowing, chewing, shoulder function, saliva, mood and anxiety scores. However, patients who underwent radical parotidectomy had clinically and statistically significantly worse speech scores (p < 0.001) as well as reduced taste scores (p = 0.05). The second component of the University of Washington Quality of Life Questionnaire score takes into account the symptoms that impact the patients the most in the last 7 days (Table 4). In this aspect, a higher proportion of patients undergoing radical parotidectomy reported concerns related to chewing (p = 0.04) and speech (p = 0.006) when compared with the limited superficial parotidectomy group.
Table 3. University of Washington Quality of Life Questionnaire scores in the radical parotidectomy and limited superficial parotidectomy groups

*n = 15; †n = 14; ‡p < 0.05 was considered statistically significant
Table 4. University of Washington Quality of Life Questionnaire importance rating for symptoms in the last seven days between the radical parotidectomy and limited superficial parotidectomy groups

*n = 15; †n = 14; ‡p < 0.05 was considered statistically significant
Parotidectomy Specific Quality of Life Questionnaire
Patients were also assessed using the Parotidectomy Specific Quality of Life Questionnaire with symptoms scores. Again, we noted similar outcomes between the two groups in the overall severity of symptom scores (median overall scores 150 vs 199 for the limited superficial parotidectomy and radical parotidectomy groups, respectively; p = 0.23). Patients within the radical parotidectomy group reported worse speech outcomes (median score 0 vs 7 for the limited superficial parotidectomy and radical parotidectomy groups, respectively; p = 0.003). In addition, the radical parotidectomy group was also found to have significantly higher levels of dissatisfaction with their appearance (median score 4 vs 11 for the limited superficial parotidectomy and radical parotidectomy groups, respectively; p = 0.04), and significantly more eye symptoms (median score 0 vs 11 for the limited superficial parotidectomy and radical parotidectomy groups, respectively; p = 0.009). The second component of the Parotidectomy Specific Quality of Life score looks at interference to QoL. Patients who underwent radical parotidectomy reported significantly higher interference to their interpersonal relationships (median score 0 vs 1 for the limited superficial parotidectomy and radical parotidectomy groups, respectively; p = 0.04), as well as eating (median 0 vs 2 for the limited superficial parotidectomy and radical parotidectomy groups, respectively; p = 0.02) and talking (median 0 vs 2 for the limited superficial parotidectomy and radical parotidectomy groups, respectively; p = 0.04). Overall, patients who underwent radical parotidectomy reported high interference to their QoL (median 0 vs 14 for the limited superficial parotidectomy and radical parotidectomy groups, respectively; p = 0.05) (Table 5).
Table 5. Parotidectomy Specific Quality of Life measures in the radical parotidectomy and limited superficial parotidectomy groups

*n = 15; †n = 14; ‡p < 0.05 was considered statistically significant
Discussion
In this study, we investigated the QoL of 15 patients undergoing radical parotidectomy who received immediate reconstruction of the facial nerve, compared to 14 patients who underwent partial superficial parotidectomy, with preservation of the facial nerve. Although there were differences noted in some of the domains, it is reassuring to note that patients undergoing radical parotidectomy with immediate facial nerve reconstruction could achieve comparable outcomes in the QoL measures in most domains measured. This was in spite of the higher incidence of adjuvant therapy administration in the radical parotidectomy group. Areas that showed consistent issues in both the QoL scoring systems were speech, chewing or swallowing, and eye symptoms.
The University of Washington Quality of Life Questionnaire is a validated self-administered scale measuring health-related quality life specifically for head and neck cancer. This is more of a general scale and does not have much specificity for patients undergoing parotidectomy with facial nerve dysfunction. The University of Washington Quality of Life Questionnaire did not report worse outcomes among patients undergoing radical parotidectomy with immediate facial nerve reconstruction in the domains of recreation, activities, appearance, mood or anxiety. This suggests that immediate reconstruction of the facial nerve or parotidectomy defect could provide near normality in the day-to-day functioning of patients undergoing radical parotidectomy procedures.
However, the University of Washington Quality of Life Questionnaire score did show a worsening of overall QoL amongst patients within the radical parotidectomy group. Although this could be interpreted as a consequence of the radical parotidectomy, we argue that this is more likely the effect of more aggressive treatment from malignant diagnosis with significantly greater number of concurrent neck dissection procedures and a higher rate of adjuvant treatment (see Table 1). This would also explain the higher rate of complaints regarding the changes to taste because dysgeusia is a common side effect with administration of radiotherapy to the head and neck region.Reference Irune, Dwivedi, Nutting and Harrington10
The Parotidectomy Specific Quality of Life Questionnaire score was specifically developed to identify the subtle symptoms that are specific to patients undergoing parotid surgical procedures, as well as exploring the impact of facial nerve dysfunction. This specific questionnaire was able to identify issues relating to eye symptoms, in addition to the similar findings of University of Washington Quality of Life Questionnaire in speech and swallowing. Again, it is reassuring to note comparable quality of life outcomes between patients undergoing radical parotidectomy with immediate facial nerve reconstruction and limited superficial parotidectomy, particularly in the domains of enjoyment of life, social activities, general activities and work activities. This corroborates the idea that there are better outcomes with immediate facial nerve reconstruction in patients undergoing radical parotidectomy.
A discrepancy was noted between the two scores in the domain of appearance, with the Parotidectomy Specific Quality of Life Questionnaire detecting a significant difference not seen in University of Washington Quality of Life Questionnaire. When this domain was investigated in detail, we noted that the University of Washington Quality of Life Questionnaire asked questions relating to facial symmetry. The Parotidectomy Specific Quality of Life Questionnaire had four components in this domain with the first three components related to symmetry (concerns about the shape of one's face or neck, concerns about the appearance of one's face or neck and concerns about uneven or mismatched hair on one's face or head). In these three questions related to static function, there were no differences detected between the two groups. The last question related to dynamic facial movement (embarrassment about one's appearance when smiling or speaking in front of other people), where we noted a significant difference in this sub-score (0.0 vs 3.0; p = 0.033), which resulted in significant differences in the overall score for this domain. In this radical parotidectomy cohort, 80 per cent had dynamic facial nerve reconstruction, with most of these dynamic reconstructions driven by the masseteric nerve, which does not provide spontaneous smile within the adult population.Reference Hontanilla, Marre and Cabello11 These factors are likely to result in the differences noted.
Interestingly, in spite of aggressive reconstruction of the peri-ocular area with upper lid loading and lower eyelid tightening, eye symptoms still remained significantly worse among patients undergoing radical parotidectomy and static eye reconstruction. Patients with a non-functioning facial nerve have ongoing problems with lagophthalmos,Reference Irune, Dwivedi, Nutting and Harrington10 no spontaneous blinkingReference Hontanilla, Marre and Cabello11 and inadequate tear drainage.Reference Vásquez and Medel12 None of these functions are restorable with lid loading or static procedures. With this in mind, our group is developing an implantable device in place of an upper lid load (bionic lid implant for natural closure) that aids in spontaneous eye closure following facial nerve palsy.Reference Biglioli13 This device is currently in its early phase of animal testing.
Speech and swallowing concerns post-radical parotidectomy with immediate reconstruction are also noted in both the QoL questionnaires, in spite of early dynamic and static reanimation. All patients within the radical parotidectomy group received adjuvant radiotherapy, which could cause further fibrosis, trismus and dysphagia that might contribute to the speech and swallowing difficulties. In addition, prior to this study, all patients with facial nerve reconstruction in our institution underwent rehabilitation with a dedicated facial physiotherapist, with no involvement of a speech pathologist. The concerns around speech and swallowing emphasise the importance of early input of the speech pathologist in the rehabilitation process of patients. Since obtaining these questionnaire results, we have engaged early rehabilitation with the speech pathologist for these patients.
• Limited data are available on quality of life (QoL) for radical parotidectomy with facial reanimation patients
• This study compared QoL for radical parotidectomy with facial reanimation patients and limited superficial parotidectomy patients
• This study used the University of Washington Quality of Life and the Parotidectomy Specific Quality of Life questionnaires
• The Parotidectomy Specific Quality of Life Questionnaire helped detect subtle issues over the University of Washington Quality of Life Questionnaire
• Radical parotidectomy and limited superficial parotidectomy patients had comparable QoL scores
• Future reconstructive efforts need to be focused on these specific issues to improve QoL in these patients
Although this study has provided good insight into the outcomes of patients with radical parotidectomy who received immediate facial nerve reconstruction, it is limited by the small sample size precluding the ability for multivariable analyses. There is also a significant imbalance between groups with regards to the number of patients with concurrent neck dissection and adjuvant treatment (radiotherapy with or without chemotherapy) that could account for some of the differences in the findings, as discussed earlier. Ideally, the radical parotidectomy patients should have been matched with superficial parotidectomy patients who all received adjuvant therapy; however, this is an uncommon clinical scenario, and the sample size was too low to make this comparison. Lastly, it is a retrospective study with cross-sectional QoL data collection over a long time period; therefore, the confounders for the results could not be controlled.
Conclusion
Patients who underwent radical parotidectomy with immediate reconstruction of the facial nerve and parotidectomy site achieved comparable overall QoL to those patients with facial nerve preserving parotidectomy. When compared with the University of Washington Quality of Life Questionnaire tool, the Parotidectomy Specific Quality of Life Questionnaire was able to better determine subtle QoL complaints relating to parotidectomy procedures and facial nerve disorders. The eye symptoms and oral and swallowing functions continue to be problematic despite attempts at immediate reconstruction of the facial nerve or parotidectomy defect. Further rehabilitation, reconstructive and management efforts are required to improve function in these patients.
Competing interests
None declared
Appendix 1. Quality of Life after Radical Parotidectomy – Patient Self-Reported Questionnaire
Part 1 – Severity:
The following questions ask about symptoms and complications that are common after treatment for conditions such as yours. Using the 0-10 scale provided, please rate how severe your symptoms have been at their WORST over the past week by circling the corresponding number. Please circle zero if you have not had the symptom.
-
1 Concern about the shape of your face or neck.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
2 Concern about the appearance of your face or neck.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
3 Concern about uneven or mismatched hair on your face or head.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
4 Embarrassment about your appearance when smiling or speaking in front of other people.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
5 Trouble keeping food and drink in your mouth.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
6 Trouble with dribbling when eating and drinking.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
7 Dry mouth.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
8 Mouth so dry that it makes eating hard.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
9 Food tastes different or less strong than it did before treatment.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
10 Difficulty opening your mouth wide enough to eat larger foods.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
11 Difficulty opening your mouth wide enough to eat certain foods or to brush your teeth.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
12 Tightness in your jaw when opening your mouth.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
13 Pain when chewing foods.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
14 Pain in or around the site of your operation.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
15 Pain that you feel is due to your treatment.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
16 Tenderness to touch at or around the site of your operation.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
17 Aching pain in or around the site of your operation.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
18 Shooting pain in or around the site of your operation.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
19 Tingling or pins-and-needles at or around the site of your operation.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
20 Numbness or reduced feeling at or around the site of your operation or your ear.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
21 Worry or anxiety about your cancer coming back.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
22 Worry or anxiety about needing to have further surgery.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
23 Worry or anxiety about needing to have further radiation therapy.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
24 Stiffness or tightness in your neck.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
25 Difficulty moving or turning your head.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
26 Weakness in your shoulder.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
27 Difficulty moving your shoulder
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
28 Difficulty using your shoulder
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
29 Difficulty with your hearing on the side of your treatment.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
30 Difficulty hearing things when at a party or shopping centre.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
31 Loss of hearing that you think is due to your treatment.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
32 Repeated infections in your ear on the side of treatment.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
33 Dryness, grittiness or pain in one or both eyes.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
34 Dryness of your eye causing discomfort.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
35 Difficulty closing your eye or keeping it closed.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
36 Reddening of your cheek on the side of treatment that appears when you are eating.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
37 Excessive sweating of your cheek on the side of treatment that appears when you are eating.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
38 Difficulty pronouncing some words and sounds properly.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
39 Problems with speaking that you think were caused by your treatment.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
40 Difficulty being understood by others due to problems with your speech.
-
No problems │ 0 1 2 3 4 5 6 7 8 9 10 │ Worst imaginable
-
Part 2 – Interference:
-
Symptoms frequently interfere with how we feel and function. How much have your symptoms interfered with the following in the past week?
-
1 Mood?
-
Did not interfere │ 0 1 2 3 4 5 6 7 8 9 10 │ Interfered completely
-
2 Relations with other people?
-
Did not interfere │ 0 1 2 3 4 5 6 7 8 9 10 │ Interfered completely
-
3 Enjoyment of life?
-
Did not interfere │ 0 1 2 3 4 5 6 7 8 9 10 │ Interfered completely
-
4 Social activities?
-
Did not interfere │ 0 1 2 3 4 5 6 7 8 9 10 │ Interfered completely
-
5 Self-confidence?
-
Did not interfere │ 0 1 2 3 4 5 6 7 8 9 10 │ Interfered completely
-
6 General activity?
-
Did not interfere │ 0 1 2 3 4 5 6 7 8 9 10 │ Interfered completely
-
7 Work (including work around the house)?
-
Did not interfere │ 0 1 2 3 4 5 6 7 8 9 10 │ Interfered completely
-
8 Eating meals?
-
Did not interfere │ 0 1 2 3 4 5 6 7 8 9 10 │ Interfered completely
-
9 Talking with other people or over the phone?
-
Did not interfere │ 0 1 2 3 4 5 6 7 8 9 10 │ Interfered completely
-
10 Sleeping (including trouble falling asleep and being woken up by symptoms)?
-
Did not interfere │ 0 1 2 3 4 5 6 7 8 9 10 │ Interfered completely
-
11 Driving?
-
Did not interfere │ 0 1 2 3 4 5 6 7 8 9 10 │ Interfered completely
-
12 Personal hygiene (such as showering, shaving, brushing hair, applying makeup)?
-
Did not interfere │ 0 1 2 3 4 5 6 7 8 9 10 │ Interfered completely
-
Thank you for your participation