Introduction
There has been increased interest in the adoption of an intracapsular tonsillectomy technique in the UK in recent years. This has been prompted by large case series reporting low rates of complications and rapid recovery from surgery,Reference Hoey, Foden, Hadjisymeou Andreou, Noonan, Chowdhury and Greig1 and supported by recommendations of the ‘Ear, Nose and Throat Surgery: GIRFT [Getting it Right First Time] Programme National Specialty Report’.2 On the basis of data collected from ENT units across England, this latter report advises that where there is appropriate clinical expertise, training and resources, intracapsular tonsillectomy should be performed in the paediatric population for obstructive or infective symptoms.
Intracapsular tonsillectomy can also be called tonsillotomy. It differs from the traditional extracapsular tonsillectomy technique, as it partially removes the tonsil tissue from within the surrounding fibrous capsule. The capsule is left intact and avoids exposure of underlying constrictor muscles. The rationale for this technique is that the tonsil tissue has less innervation, resulting in reduced pain and smaller diameter vessels within it, with reduced bleeding risk.
Coblation is a technique of controlled ablation performed using bipolar radiofrequency energy under a conductive medium such as normal saline, which creates a plasma field. The plasma field breaks down tissues at relatively low temperatures (40–70°C) compared to traditional ‘hot’ techniques such as electrocautery (over 100°C).Reference Pynnonen, Brinkmeier, Thorne, Chong and Burton3 While other techniques for intracapsular tonsillectomy are available, the use of coblation is widespread and it is the authors’ preference for the surgical technique.
The adoption of a new surgical technique inevitably is accompanied by an educational need. This paper aims to outline the equipment preparation and surgical steps for intracapsular coblation tonsillectomy, including recognition of the tonsillar capsule. We also discuss how to avoid and deal with common complications. However, surgeons must still acquire competence by attending a structured, approved course before embarking on coblation techniques.
The article is based upon the experience of the senior author, who teaches on the international Smith & Nephew Coblation course, and has taught both consultant and registrar colleagues. The author has performed over 900 intracapsular coblation tonsillectomies, and uses the technique for both obstructive and infective symptoms.
Preparation
Patient position
Patient positioning is the same as for standard tonsillectomy. For the majority of cases, a reinforced laryngeal mask airway is used. Figure 1 demonstrates a reinforced laryngeal mask airway in situ with a Boyle–Davis mouth gag.

Fig. 1. Image of a left tonsil being medialised using a tonsil retractor. A reinforced laryngeal mask airway can be seen, along with a Boyle–Davis mouth gag.
Equipment checks
Wand
The Smith & Nephew Procise EZ View Coblation Wand (Watford, UK) is the authors’ preference because of its low-profile shaft, which improves surgical field visualisation and is particularly helpful in children with smaller anatomy. The wand can be used for both tonsillectomy and adenoidectomy.
Settings
Coblation level 7 is the default setting for the Procise EZ View Coblation Wand. We use setting 7 for the majority of the tonsillectomy. The setting can be increased to 9 in large tonsils where there is a requirement to quickly reduce tonsil tissue. The setting can be reduced to 5 when the Coblation wand is used near to the capsule. A setting below 5 should be avoided, as there is no coblation effect. The coagulation setting defaults to 3 and this is not adjusted.
Suction
The Coblation wand must be attached to suction. Smith & Nephew recommend having suction set at 250–350 mmHg and not running other suction tubes from the same cylinder.4
Irrigation
The Coblation wand must have a constant flow of saline for irrigation. One litre of 0.9 per cent normal saline is connected and it is unusual that any more is needed for a case. Flow rates can be adjusted using the roller clamp. Smith & Nephew recommend three drops per second.4 Too little flow will not allow coblation of tissue, and will cause charring and blockage of the wand.
Prior to the procedure, always check the irrigation by holding the Coblation wand against a sterile drape or gauze. There should be a flow of irrigation, effective suction, and yellow or orange glow, which indicates the presence of a plasma field.
Surgical steps
Basic principles
First, improve visualisation of the tonsil and tonsil fossa. This can be accomplished by the use of a pillar retractor to retract the anterior pillar and bring the tonsils into view (Figure 1), or by holding the posterior pillar with straight forceps (Figure 2). Pressure lateral to the anterior pillar with a blunt instrument may be used to medialise the tonsil, but care must be taken to avoid injury to the pillar and its covering mucosa.
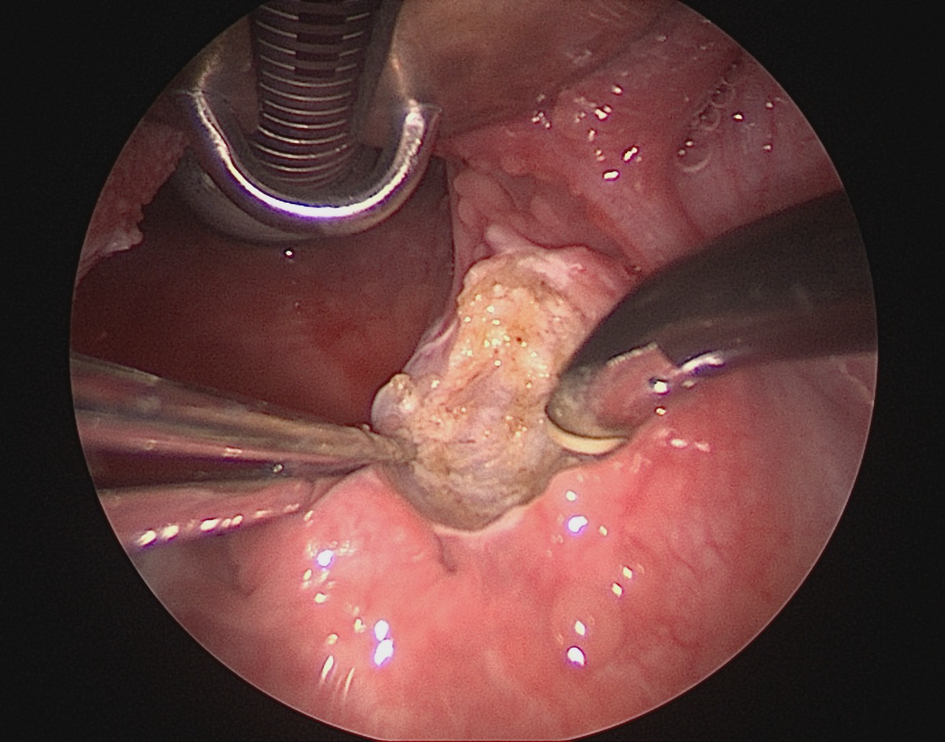
Fig. 2. Image of a right tonsil being medialised using straight, toothed forceps.
Second, the Coblation wand should be held so that it hovers over the surface of the tonsil tissue, using near-touch rather than contact. The technique has been likened to laser. Pressure applied to the tonsil with the wand face during coblation should be kept to a minimum, as it can lead to tunnelling into the tonsil tissue or blockage of the wand.
Third, tissue reduction using coblation is carried out in careful, controlled sweeping movements. This technique is often likened to the use of a drill during mastoid surgery.
Fourth, tissue reduction is carried out over a ‘broad front’, avoiding tunnelling into the tonsil tissue
Fifth, coblation should never be used unless the tip of the wand can be seen. The surrounding muscular tissues have very little resistance to coblation and significant damage can be caused to surrounding tissue.
Sixth, damage to the surrounding musculature is more likely to occur than a breach of the capsule, so particular care should be taken to avoid damage to the pillars and the area inferior to the inferior pole.
Seventh, bleeding during tonsillectomy may indicate either that tonsillar tissue remains (Figure 3) or the capsule has been breached. If the capsule has been breached, you will see the underlying muscle fibres.

Fig. 3. Image of left tonsil tissue after coblation. The small superior bleed likely represents remaining tonsillar tissue.
Eighth, tonsil capsule can be recognised by a change in texture and colour. The tonsillar capsule texture is smooth, while tonsil tissue is ‘fluffy’. The capsule has a grey-blue or sometimes brownish tinge.
Ninth, regarding when to stop, when the capsule has been identified it is important to examine the whole tonsil to make sure that the majority of the tonsil tissue has been removed. Tonsillar tissue can commonly be missed in the superior and inferior poles. In Figure 4, the superior half of the tonsillar fossa has been effectively cleared, while some tonsil tissue remains inferiorly. Following completion, wait a few minutes to ensure there is no delayed reactionary bleeding.

Fig. 4. Image of a left tonsillar fossa. Capsule is visible at the superior pole.
Technical difficulties
Right tonsil
For right-handed surgeons, holding the Coblation wand in the left hand for right-sided tonsillectomy may feel unnatural. By medialising the posterior pillar with straight, toothed forceps, you are able hold the tonsil wand in your right hand (Figure 2). It is important that, when doing this, the tonsillar fossa is also grasped with the forceps, to prevent avulsion of the pillar and exposure of muscle.
Upper pole
The upper pole of the tonsillar fossa is the most difficult area to visualise. It is often helpful to use the pillar retractor to expose this area.
Breach of capsule
The commonest indicator of a breached capsule is an area of bleeding. This is stopped by using the coagulation function. Further coblation in the area can result in significant penetration of the underlying muscle. Great care must be taken when removing tissue around the area, as lateral spread of coblation can cause further damage. Under these circumstances, leaving a small amount of tonsil tissue adjacent to the breach is often preferable.
Blocked wand
A blocked wand can be recognised by increased vapour in the operative field or loss of the suction effect. If there is visible debris on the wand face, wipe this away with damp gauze. This should be done gently, as the gauze fibres can snag the tip electrodes. If wiping is unsuccessful, take a small pot filled with saline and perform coblation with the wand face partly submerged in the saline. If this fails, the wand can be cleared using a retrograde flush. Using a 10 ml syringe of saline, disconnect the suction and flush the wand through the suction port while carrying out coblation on a setting of 9.
Competing interests
The senior author delivers educational activities for Smith & Nephew and receives honoraria for this. Neither author receives financial incentives from Smith & Nephew and do not declare any conflict of interest.






