Introduction
Cochlear implantation is a well-known treatment for severe to profound deafness, for which various surgical techniques have been described. Posterior tympanotomy, which entails opening a window to the middle ear from the mastoid between the facial nerve and chorda tympani with round window membrane insertion was utilised for this study.
High-resolution computed tomography (CT) of temporal bones, with its superior bone resolution and multiple reformates, is of paramount importance for pre-operative surgical planning. Over many years, various individual parameters on CT scans have been studied and attempts have been made to correlate them with intra-operative findings. But no comprehensive scoring system has yet been developed that facilitates a cochlear implantation surgeon to objectively predict the difficulties that might be faced during surgery while performing cochlear implantation via the posterior tympanotomy approach.
This study intended to fill this lacuna by providing a structured checklist-based scoring system that can be utilised to predict intra-operative difficulties and ease of electrode insertion by pre-operative evaluation of certain specific attributes in high-resolution CT of temporal bones.
The aims of this study were fourfold: (1) to investigate the accuracy and internal validity of the proposed scoring system; (2) to establish correlation between the proposed scoring system and intra-operative difficulties; (3) to determine a cut-off score above which a surgeon can be certain of a difficult surgery; and (4) to provide surgeons and radiologists with a structured checklist for pre-operative analysis and reporting, with relation to each key surgical step.
Materials and methods
Patient selection
This prospective, double blinded study was performed from January 2017 to January 2020 at a tertiary care hospital. A total of 55 patients with severe to profound hearing loss and fulfilling criteria for cochlear implantation were selected; out of these patients, 3 had to be excluded as cochleostomy was needed. All patients underwent pre-operative radiological assessment. Computed tomography scans for the temporal bone were obtained with a slice thickness of 0.6 mm, acquired at 120 kVp, 250 mA, with an imaging matrix of 512 × 512 and viewed in standard bone window setting (window width–4000; window length–700).
Inclusion criteria consisted of: age within 5 years; fulfilling audiological criteria of having bilateral severe to profound hearing loss not benefitting from hearing aid use; psychological criteria of Intelligence Quotient of more than 80 on the Stanford Binet Intelligence Scale; and without history of developmental delays, mental retardation or abnormal psychological behaviour. All patients had normal inner ear anatomy and vestibulocochlear nerve (on magnetic resonance imaging). Patients who had undergone revision surgery, alternative techniques of implantation (Veria, endoscopic, subtotal petrosectomy and so on) and who had medical and surgical contraindications for surgery were excluded from the study.
Approval of the Institutional Ethics Committee was obtained. Consent to store patient data and utilise it for research without disclosing the patient's identity was taken from their guardians.
Surgery
All surgical procedures were performed under general anaesthesia by the same surgical team. Post-aural skin incision was placed, soft tissue flap was elevated and cortical mastoidectomy was performed. The facial recess was identified and posterior tympanotomy was performed. The round window niche was identified in the middle-ear cavity and the anterosuperior part of niche was drilled to identify the membrane completely. Electrodes were inserted after reflecting the membrane. The receiver-stimulator of the implant was fixed with 1-0 polypropylene suture over the temporo-parietal region of cortical bone of the skull.
Study parameters and result analysis
Six parameters that are most likely to determine difficulty of surgery, according to existing literature as well as our experience and knowledge, were analysed to prepare the Cochlear Implantation Radiological Assessment Score (CIRAS). Each parameter was concerned with the key steps of surgery and has been scored either as 1 (favourable anatomy) or 2 (unfavourable anatomy), thereby having a maximum possible score of 12 and minimum possible score of 6 (Table 1).
Table 1. Cochlear Implantation Radiological Assessment Score (CIRAS)

*Total score = 12; †sigmoid sinus position is determined by posterior extension of a line joining the crus commune to the posterior semicircular canal axis (the most protruding portion of sigmoid sinus lies anterior or posterior to this line).Reference Mandour, Tomoum, Zayat, Hamad and Amer1 ‡Round window niche visibility is determined by whether the external auditory canal line and prediction line are parallel or not. Parallel lines entail easy visibility whereas intersecting lines entail poor visibility. The external auditory canal line is the line between the bony cartilaginous junction of posterior external auditory canal wall and tympanic annulus, and the prediction line is the line between posterior margin of round window niche and anterolateral part of facial nerve.Reference Mandour, Khalifa, Khalifa and Tomoum2 **Round window membrane accessibility is determined by whether axis of basal turn of cochlea and axis of internal carotid artery are parallel or not. Parallel lines indicate easy accessibility and intersecting lines indicate poor accessibility.Reference Alam-Eldeen, Rashad and Ali3
Image analysis (group A)
The CT images of each patient were assessed in coronal and axial planes by a team comprising a radiologist and an ENT surgeon. CIRAS was then calculated and utilised to predict the ease of surgery pre-operatively.
Intra-operative findings analysis (group B)
All the surgical procedures were video recorded, and the recordings were later played in front of a panel of three expert ENT surgeons (including the primary surgeon), who then reached a consensus on whether the surgery was easy or difficult.
Groups A and B were blinded to each other's work. Statistical analysis was performed by an independent investigator. Results were analysed vis-à-vis time taken for key steps of surgery (cortical mastoidectomy, posterior tympanotomy, round window niche visualisation and round window membrane electrode insertion), need for any extra instrumentation (thinning the facial nerve canal, drilling the mastoid tip, anterior transposition of posterior canal wall and extended facial recess approach) and whether the surgery was easy or difficult according to the opinion of the panel of three ENT surgeons.
For establishing correlation, Pearson's coefficient for parametric variables and Spearman's coefficient for non-parametric variables were utilised. Receiver operating characteristic analysis was performed and Youden's index was calculated to determine the cut-off Score. Area under the curve was measured to determine the inherent validity of CIRAS.
Receiver operating characteristic curve is a plot that depicts the trade-off between the sensitivity and 1-specificity across a series of cut-off points. It is useful for selecting an optimal cut-off point for a test and for comparing the accuracy of diagnostic tests. Youden's index (J statistic) is used to determine the optimal threshold because it reflects the intention to maximise the correct classification rate and is easy to calculate. Area under the receiver operating characteristic curve is considered as an effective measure of inherent validity of a diagnostic test. It is a reflection of how good the test is: the greater the area under the curve, the better the test. A perfect test will have an area under the curve of 1.0, whereas a completely useless test (one whose curve falls on the diagonal line) has an area under the curve of 0.5. For the area under the curve: more than 0.9 = excellent accuracy, 0.8–0.9 = good accuracy, 0.7–0.8 = fair accuracy and 0.6–0.7 = poor accuracy.
Statistical analysis was performed with help of SPSS® statistical analysis software (version 23) and MedCalc® statistics analysis software (version 19.4.1). Computed tomography images were analysed with the help of Horos™ medical images viewer (Figure 1).
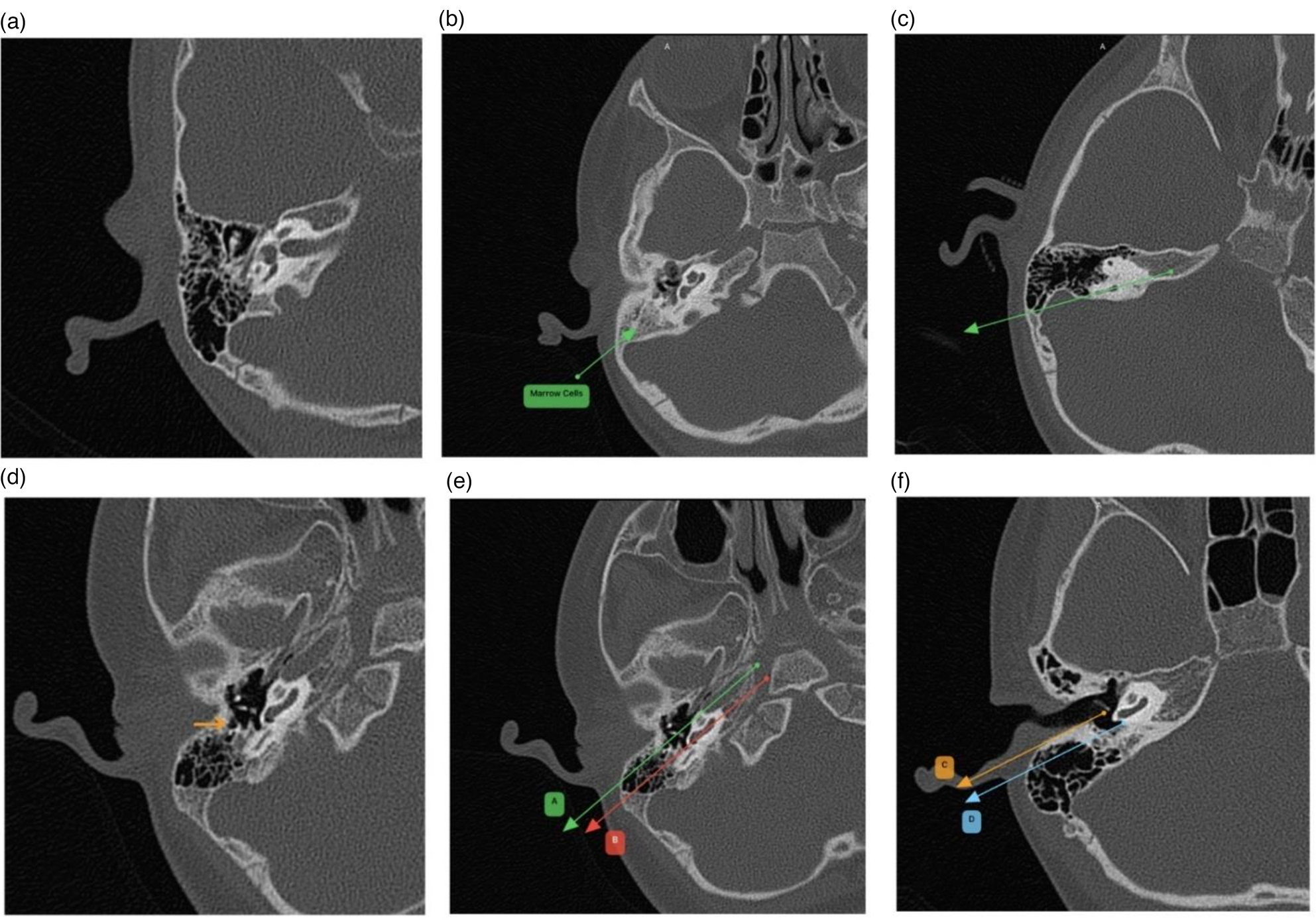
Fig. 1. High-resolution computed tomography images showing: (a) pneumatic mastoid, (b) marrow cells, (c) anteposed sigmoid sinus, (d) facial recess (sentinel) cell and (e) easy accessibility of round window membrane (lines A (line along axis of internal carotid artery) and B (line along basal turn of cochlea) are parallel). (f) Easy visibility of round window niche (lines C (external auditory canal line) and D (prediction line) are parallel).
Results
Numerical and categorical data were obtained. Data were summarised as mean ± standard deviation (SD) for numerical variables and count and percentages for categorical variables. Shapiro–Wilk test was performed to check the data for normality.
The mean age of patients was 38 months with a range of 12–60 months. The male to female ratio was 7:6. There was no statistically significant difference in results between the two genders (p > 0.05).
Amongst 52 patients, 46 (88.4 per cent) had a pneumatic mastoid and 6 (11.6 per cent) had a sclerotic mastoid. Marrow cells were found in 17 (32.7 per cent) patients. Furthermore, 15 (28.8 per cent) patients had an anteriorly lying sigmoid sinus, and it was normally positioned in the other 37 (71.2 per cent) patients. In 33 (63.5 per cent) patients, sentinel cell was present. The round window niche was easily visible in 31 (59.7 per cent) patients and was difficult to visualise in 21 (40.3 per cent) patients. The round window membrane could be easily accessed in 32 (61.5 per cent) patients and the other 20 (38.5 per cent) patients required extra manoeuvres before electrode insertion.
The mean (± SD) time taken from the start of bone drilling to electrode insertion was 105.2 (±12.8) minutes with a range of 92–134 minutes. Mean time for surgery in patients with CIRAS less than or equal to 8 was 98.16 (± 5.06) minutes, whereas for CIRAS of more than 8, it was 122.73 (± 8.51) minutes. This difference was statistically significant (p < 0.05).
By testing for correlation, Pearson's correlation coefficient between CIRAS and the time taken for surgery was found to be 0.899, which signifies strong positive correlation and is statistically significant (p < 0.001) (Figure 2).

Fig. 2. (a) Line diagram between Cochlear Implantation Radiological Assessment Score (CIRAS) and mean time taken for surgery, which increases drastically after a score of 8. (b) Box plot with median of time taken during surgery with each value of Cochlear Implantation Radiological Assessment Score (CIRAS).
The receiver operating characteristic analysis showed area under the curve was 0.828 with 95 per cent confidence interval of 0.697 to 0.918 and significance level (area = 0.5) of p < 0.0001 which implies CIRAS has good accuracy and is a valid scoring system to successfully predict the difficulty of surgery. The associated criterion for Youden's index (J = 0.4953) was a CIRAS value more than 8 with a specificity of 93.10 per cent, meaning that for a pre-operative value more than 8 on CIRAS, the surgery is highly likely (93.10 per cent chance) to be difficult (Figure 3).

Fig. 3. Receiver operating characteristic curve area under the curve signifying good accuracy. Area under the curve (AUC) = 0.828.
Regarding the need for extra instrumentation, 11 (21.1 per cent) patients required skeletonisation of the facial nerve canal, 5 (9.6 per cent) patients needed extended facial recess approach, anterior wall transposition needed to be performed in 5 (9.6 per cent) cases, and drilling the mastoid tip was performed in 6 (11.5 per cent) cases to adequately visualise the round window niche and increase the working space in the middle ear, especially in cases with posteriorly rotated cochlea. Moderate positive correlation was found between CIRAS and the need for extra instrumentation with Spearman's rho being 0.577, which is statistically significant with p-value of less than 0.001.
Discussion
Cochlear implantation via posterior tympanotomy remains one of the most accepted approaches worldwide. This is the era of ‘soft’ electrode insertion to preserve residual hearing.Reference Friedland and Runge-Samuelson4 Round window insertion is distinctly advantageous over cochleostomy because the former is more physiological and leads to lesser damage to the inner ear.Reference Adunka, Gstoettner, Hambek, Unkelbach, Radeloff and Kiefer5 Though cochleostomy is technically less challenging to perform than round window insertion, a surgeon should always strive for round window insertion because it is performed antero-inferiorly along the basal turn,Reference Adunka and Buchman6 which is easier to visualise and access. Cochleostomy should be reserved for difficult cases, where round window insertion is not feasible.
The key surgical steps are cortical mastoidectomy, posterior tympanotomy, round window niche identification and round window insertion. Each step can be complicated not only by elements inherent to that step but also faulty surgical technique during the previous steps. The most important factor that ensures a successful cochlear implantation is the optical axis. This is the straight line axis along which the surgeon visualises the round window niche and subsequently performs round window insertion. CIRAS has been developed on this principle of visual axis, addressing specific parameters that determine difficulty in carrying out these steps (Figure 4).

Fig. 4. Optical axis for cochlear implantation. SS = sigmoid sinus; Fn = facial nerve; Ct = chorda tympani; RWM = round window membrane; At = apical turn of cochlea; Mt = middle turn; Bt = basal turn; Cn = cochlear nerve
CIRAS is an objective, simple yet structured radiological scoring system to predict the operative difficulty while performing cochlear implantation via posterior tympanotomy. The score is comprehensive and easy to administer, thereby obviating the need for an expensive workstation and software. It is intended to be utilised by ENT surgeons before proceeding to surgery, using high resolution CT images of patients pre-approved for cochlear implantation to predict the ease of surgery.
Since pre-operative analysis of high-resolution CT of temporal bone is essential to chart out the surgical roadmap, numerous studies have tried to correlate radiological findings with intra-operative findings by utilising different parameters like pneumatisation patterns, sigmoid sinus and middle cranial fossa dura levels, facial recess anatomy, variations of facial nerve course, Korner's septum, mastoid emissary vein and jugular bulb position.Reference Alam-Eldeen, Rashad and Ali3 Yet other studies have included certain specific parameters, such as measurement of distance between the short process of the incus and round window niche or distance between oval window and round window nicheReference Pendem, Rangasami, Arunachalam, Mohanarangam and Natarajan7 or measurement of facial recess dimensions,Reference Vaid, Vaid, Manikoth and Zope8 many of which require complex post-processing of CT images and employ high-end graphics workstations. Optimal visualisation along the optical axis as described above is influenced maximally by adequate posterior tympanotomy, in addition to other factors such as sigmoid sinus position and rotation of cochlea.
Facial recess (sentinel) cell
Prior knowledge of facial recess anatomy is an absolute requirement before performing posterior tympanotomy. Presence of facial recess cell(s) is a straightforward and reliable indicator of adequate space while performing posterior tympanotomy because drilling in this area will expose the superior part of facial recess and thereby guide the surgeon for its enlargement.Reference Park, Amoodi, Kuthubutheen, Chen, Nedzelski and Lin9 In our study, the cellularity was noted in axial sections and did not involve any complex calculations.
In some cases, the facial recess may be narrow and extra instrumentation may be required to achieve adequate exposure. Extended facial recess approach, facial nerve skeletonisation, anterior transposition of posterior canal wall, drilling until the mastoid tip and chorda tympani transposition are examples of such steps.Reference Dreisbach, Balkany and Seibert10,Reference Wang, Yang, Jiang and Zhang11
Round window niche visibility
The most crucial step of implantation via posterior tympanotomy is visualisation of the round window niche. Depending on the architecture of the facial recess and position of the cochlea itself, the round window niche may sometimes be difficult to locate intra-operatively. This in turn increases the operating time. If unanticipated, one may even mistake a hypotympanic cell to be the round window niche, leading to faulty insertion. Precise localisation of the niche and prior anticipated view through the posterior tympanotomy window can be accurately predicted with the help of following lines: first, the external auditory canal (EAC) line, which represents the inclination of posterior EAC wall and might obscure the view along the optical axis, and second, the prediction line, which indicates the location of the mastoid segment of facial nerve. It has been found that if these two lines are parallel then the round window niche is easily visible through the posterior tympanotomy window.Reference Kashio, Sakamoto, Karino, Kakigi, Iwasaki and Yamasoba12,Reference Elzayat, Mandour, Lotfy and Mahrous13
Round window membrane accessibility
In cases of posteriorly rotated cochlea and those with thick bony overhang, it might be difficult to locate the round window membrane despite the niche being visible after adequate posterior tympanotomy. In such cases, drilling of the tegmen, anterior and posterior pillars may be required. In order to predict the accessibility of the round window membrane, two lines, as described previously, are drawn on the axial CT. Alam-Eldeen et al. found that if these lines are parallel, the membrane is easily accessible and if they intersect, the accessibility is difficult.Reference Alam-Eldeen, Rashad and Ali3
Sigmoid sinus position
An anteriorly placed sigmoid sinus represents surgical restraints while performing posterior tympanotomy and accessing the round window. Our method to infer sigmoid sinus position is in conjunction with the method proposed by Sun et al.Reference Sun, Lee and Jang14 and further studied for cochlear implantation by Mandour et al.Reference Mandour, Tomoum, Zayat, Hamad and Amer1 Whereas Sun et al. did not correlate their radiological findings with intra-operative findings, Mandour et al. found significant correlation between the two. Both these studies have utilised two additional lines on high resolution CT and have graded the sigmoid sinus position. A major limitation is the confusion to classify the sigmoid sinus in cases where the three reference lines are overlapped. Furthermore, just the utilisation of posterior semi-circular canal line is enough to determine sigmoid sinus position for surgical purposes. This is simple as well as less time consuming.
Mastoid pneumatisation
Pneumatisation of mastoid has a direct implication on difficulty of cortical mastoidectomy and access to facial recess. Woolley et al. also reported increased operative time in cases with sclerosed mastoid because of limited approach to facial recess.Reference Woolley, Oser, Lusk and Bahadori15 Furthermore, in children with incomplete pneumatisation, the facial nerve is at risk of injury.Reference Vaid, Vaid, Manikoth and Zope8 Mastoid pneumatisation was noted on axial and coronal cuts in our study, whether pneumatic or sclerotic, and a score was given accordingly.
Marrow cells
Haematopoietic marrow cells are frequently present in the mastoid bone of children. These cells constitute potential sites of haemorrhage. It takes extra effort and instrumentation to control this bleeding which increases the operative time. It is important to manage this bleeding before proceeding to posterior tympanotomy and electrode insertion. Entry of blood via the round window may negatively impact inner ear homeostasis. In our study, marrow cells were noted to be either present or absent by analysing axial and coronal cuts.
Other checklists and scores have also been developed to predict surgical difficulty, but they have certain limitations like being too complicated, radiologist dependent, not specific for any approach of cochlear implantation, or requiring complex calculations and reformation of images in different planes. Therefore, it seems pertinent to universally incorporate a simple radiological assessment score, such as CIRAS, in pre-operative workup of the patient because the number of cochlear implantation surgical procedures is increasing exponentially worldwide. In the near future, it is set to become one of the most commonly performed otological procedures, even at lower tiers of healthcare.
There are certain limitations to this study. Factors associated with cortical mastoidectomy, posterior tympanotomy, round window niche visibility and round window membrane accessibility only have been considered. Other factors that could influence the electrode array insertion and the surgery altogether have been considered but have not been reported in our proposed checklist as those cases did not fulfil the inclusion criteria of our study. These cases were managed individually and were excluded from the study to avoid bias. Furthermore, the sample size consisted of 52 patients only, and this was not a randomised, controlled trial. These limitations should be addressed in subsequent studies (Figure 5).

Fig. 5. Intra-operative images showing: (a) easy visibility of round window niche, (b) difficult visibility of round window niche, (c) easy accessibility of round window membrane and (d) difficult accessibility of round window membrane.
Conclusion
The CIRAS is not only simple to use but also has internal validity and accuracy that have been established by sound receiver operating characteristic analysis. It will help the surgeon to mentally prepare himself before the surgery as well as arrange for necessary armamentarium and mentor guidance beforehand. Furthermore, it can aid the mentor's decision making to allocate difficult cases to surgeons of appropriate expertise. In addition, it also gives an estimate of extra time that might be required for difficult cases. Utilisation of this score during pre-operative workup will not only save valuable time but also prepare the surgeon for challenges that might be faced intra-operatively. Finally, CIRAS can be adapted universally as a standard reporting format by radiologists.
• Posterior tympanotomy with round window insertion is the most commonly used technique for cochlear implantation worldwide
• Surgical success and safety depend primarily on visibility and accessibility of round window niche and membrane
• High-resolution computed tomography of temporal bones provides an accurate surgical roadmap for cochlear implantation
• Intra-operative difficulty can be correctly anticipated by CIRAS
• CIRAS with its proven accuracy and internal validity, can predict a difficult surgery
• CIRAS can be used as a standard reporting and evaluation protocol
Competing interests
None declared








