Introduction
Most in the field of otorhinolaryngology will recognise the name of Gustav Killian (Figure 1). Many will recall that he described a dehiscence between the fibres of the inferior constrictor which can give rise to a pharyngeal pouch. Others will associate Killian with his eponymous incision and speculum, which still see regular use in septal surgery. Whilst such eponyms reflect much of Killian's contribution to medical science, his most important work does not bear his name, and perhaps because of this his true influence on today's practice is often overlooked. Certainly, few practising within the field of otorhinolaryngology at the turn of the twentieth century would not have heard of him. However, it was not the eponyms which we now recall that had made him famous. Rather, Killian's celebrity stemmed from his innovation in the direct visualisation and instrumentation of the tracheobronchial tree.

Fig. 1 Gustav Killian, 1860–1921.
In 1897, Killian had been the first to perform bronchoscopy.Reference Kollofrath 1 A commonplace procedure now, at the time it marked a sea-change in medical practice and established the foundations for many techniques on which we now depend.
The first bronchoscopy
The importance of Killian's innovation is best conveyed by describing the events which led up to its first application.Reference Zöllner 2
The evening of 30 March 1897 represented a turning point in Killian's academic and professional life. That evening, a 63-year-old farm worker from the Black Forest was brought to Killian's hospital in Freiberg distressed, having aspirated a pork bone whilst eating soup. The patient's condition rapidly deteriorated, with severe dyspnoea and intractable coughing giving way to worsening haemoptysis. At that time, an aspirated foreign body carried a grim prognosis, and the only means of treatment was by blind removal via a tracheostomy. This was what was initially proposed for the patient. At the time, a tracheostomy was in itself considered by many surgeons to be a highly dangerous procedure, and the attending surgeon felt the case to be hopeless. Thankfully for the patient, the young professor of laryngology in Freiberg had been waiting for just such a case.
Killian had first realised the potential for direct bronchoscopy some two years previously, whilst attending an annual meeting of the laryngologists of South Germany. There, he had watched a presentation by Kirstein describing his new technique of direct laryngoscopy.Reference Kirstein 3 In the preceding decades, laryngology as a speciality had rapidly burgeoned, following the popularisation of indirect laryngoscopy by the likes of Garcia, Türck and Czermek in the 1850s. However, the speciality was still severely limited by the technology of the time. Direct inspection of the larynx had remained impossible until the introduction of cocaine anaesthesia in 1884. Kirstein himself commented that whilst he was able to observe the trachea through the vocal folds, he was reluctant to proceed any further, fearful as he was of the rhythmic protrusion of the aorta visible through the anterior tracheal wall.Reference Kirstein 3
However, Kirstein's lecture provided an impetus for Killian, who was also aware of the work of Pieniazek of Krakow, who had reported successful examination of the trachea via a tracheostomy, using an aural speculum.Reference Pieniazek 4 And so Killian returned to Freiberg and began experimenting with the currently available oesophagoscopes, convinced that direct trans-glottic visualisation of the trachea and bronchus would be possible. His first experiments were performed on tracheostomy patients. By using cocaine and narrow lumen oesophagoscopes, he was able to intubate the trachea via a tracheostomy. He noted that the bronchi, rather than being stiff and rigid as conventionally believed, were actually quite elastic and distensible.Reference Killian 5 His first cautious attempts at direct bronchoscopy were practised on cadavers, before he enlisted the help of a recently retired hospital janitor. The janitor was reported as being a willing test subject, although whether his enthusiasm was kindled by Killian's modest fee or as a side effect of the cocaine anaesthesia remains unclear.Reference Zöllner 2 , Reference Meirelles and Neves-Pinto 6 Again, Killian found that he was able to enter the cocainised trachea and bronchi of an awake individual with remarkable ease and with ‘no bleeding whatsoever’. Killian commented in his journal ‘I think I have made an important discovery’.Reference Killian 7
This observation was clearly prophetic, but Killian still had to make a practical demonstration of his technique. The evening of 30 March 1897 provided just such an opportunity.
One can only imagine the drama of that night. The patient, dyspnoeic and distressed, was prepared with cocaine and made to lie on the operating table, his head extended. Using a Rosenheim oesophagoscope illuminated by an electric lamp, Killian successfully entered the trachea. There, he found a slimy mass filling the right main bronchus. Several attempts were made at withdrawing the pork bone, but the lumen of the oesophagoscope was too small. Finally, Killian grasped the foreign body and with a final effort withdrew it with the tube.Reference Kollofrath 1
To the astonishment of many, the patient made a full recovery. Buoyed by his success, Killian went on to remove two further foreign bodies over the course of the next year.
In 1898, he presented his findings at the meeting of South German laryngologists.Reference Killian 5 Bronchoscopy is such a commonplace procedure today that it is easy to underestimate the importance of the breakthrough which Killian had achieved. Hans Killian, Gustav's son, recalls his father's journal entry on the matter:Reference Killian 7
One has to be witness when a patient who feels himself doomed to death can be saved by the simple procedure of introducing a tube with the help of a little cocaine. One must have had the experience of seeing a child that at 4 pm aspirated a stone, and that, after the stone has been bronchoscopically removed at 6 pm, may happily return home at 8. Even if bronchoscopy were ten times more difficult as it really is, we would have to perform it just for having these results.
A review of patients treated for foreign body aspiration in Killian's clinic over a 10-year period listed 703 cases. In all but 12, the foreign body was successfully removed and the patient recovered.Reference Brunings, Albrecht and Kullner 8 One has only to contrast this 98 per cent success rate with the grim prognosis for patients prior to Killian's innovation to recognise the true magnitude of his discovery.
Killian's life
Compared to the celebrity he achieved in later life, Killian's early years were modest. The youngest son of a schoolteacher, he was born in 1860 in the German town of Mainz. Although not impoverished, Killian's early life was blighted by the still-present menace of cholera. His mother died before he was five and three of his siblings later succumbed, leaving Gustav's father to raise his remaining two sons alone. The years following his mother's death were difficult. His father fell out of employment and sought consolation in alcohol. However, despite their austere beginnings, both Gustav and his elder brother Johann reached adulthood and succeeded in gaining scholarships to study medicine.
Killian moved first to Strasbourg, followed by periods studying in Freiberg, Berlin and finally Heidelberg, where, in 1884, he passed his final examinations and became engaged to a young woman from an eminent local family. Unfortunately, Killian had little money with which to start family life. Lacking a substantial inheritance, he had to rely on his own ambition and hard work to build a career for himself. Initially, Killian sought to advance himself as a general surgeon. He moved to Frankfurt, where he worked as a resident surgeon. After a year, the position of head surgeon became available. Still aged only 26, he entered into fierce competition with Ludwig Rehn, a surgeon 11 years his senior, who would eventually gain fame as a pioneer of open-heart surgery. Unfortunately, Killian lost out to Rehn, not surprisingly perhaps given the latter's seniority. Killian, however, was dejected by his failure. He abandoned general surgery and moved to Berlin to join his brother and, like him, pursue a career in otolaryngology.Reference Dundas-Grant 9
In Berlin, his brother introduced him to Professors Hartmann and Fränkel, and within a year he had established himself as a rising star and innovator within the faculty. During this time, he invented a new galvano-caustic device for removing lesions from the larynx, and experimented with new forms of hearing aids.Reference Stasche 10 However, the ever-pressing need to establish a profitable practice continued to dog Killian, and he cut short his time studying in Berlin. He moved to Mannheim where he established his own clinic, a move which he hoped would provide the means to support his young wife.
Later that year, fate dealt Killian a lucky hand. The death of Professor Wilhelm Hack as a result of a tricycle accident in 1887 made vacant the post of head of the nose and throat clinic at Freiberg Medical School. 11 Killian, having established a name for himself in Berlin, was successful in securing that position. In Freiberg, he published his professorial thesis concerning the development of the pharyngeal tonsil and its function.Reference Killian 12 His theory that the tonsils were immune organs proved somewhat controversial, with many of his peers continuing to assert that the tonsils played a role in digestion or haematopoesis. 13 Despite his detractors, Killian successfully defended his thesis, and he was granted the chair of laryngology and rhinology in 1888.
Killian's arrival in Freiberg represented the start of his most productive period in terms of research and innovation. It was whilst in Freiberg that he popularised his operation to correct nasal septal deformity by submucous dissection, and he introduced a radical new operation for frontal sinusitis.Reference Killian 14 , Reference Killian 15 His most important work, however, focused on the development of novel means of visualising the larynx and trachea, and it was these innovations which were to catapult him into the international spotlight.
The aftermath of the first bronchoscopy
The new method of direct bronchoscopy was greeted with huge enthusiasm, and Killian's clinic in Freiberg became a Mecca for laryngologists from around the world. Killian's son recalls 20 bronchoscopy courses being organised in 1 year, attracting over 400 delegates.Reference Killian 16
In 1907, Killian travelled to America at the invitation of the American Triological Society. His tour took him to New York, Washington (where he was introduced to Theodore Roosevelt), Pittsburg (where he met Chevalier Jackson), and on to Montreal and Chicago.Reference Killian 7 He not only lectured but also gave practical demonstrations of his techniques. It was during this tour that he presented his description of the pharyngeal dehiscence which now bears his name.Reference Killian 17 On his departure, he was awarded a gold medal by the American Society of Laryngology.
Such was his eminence that, when Fränkel retired from his post as professor of laryngology in Berlin in 1911, he nominated Killian as his successor. Others, most notably the professor of otology, Passow, wanted to exclude Killian and amalgamate the specialties into a single chair of otorhinolaryngology under Passow's authority. Killian's supporters argued that his tremendous achievements were deserving of a separate chair. Killian enjoyed the support of Sir Felix Semon, who had advised on the care of both Kaiser Freidrich's laryngeal malignancy and Kaiser Wilhelm's ear disease, and as such had a degree of influence at the German Imperial Court.Reference Rohl 18 According to Zöllner, a timely intervention from Semon was crucial in securing the position for Killian.Reference Zöllner 2 With his election to the chair in Berlin, Killian had now reached the zenith of his career.
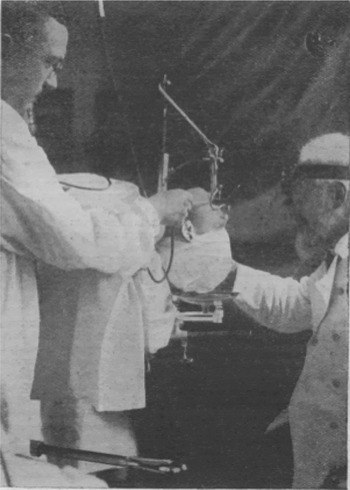
Killian continued to innovate. In 1914, he visited London at the invitation of Felix Semon, where he delivered the second-ever Semon Lecture (the first to be held at the Royal Society of Medicine), describing the novel technique of suspension laryngoscopy (Figure 2). 19 , Reference Killian 20 This new technique allowed a superior view of the larynx and freed both hands for operating. The importance of this innovation is easily seen in today's operating theatre, as it paved the way for modern microlaryngoscopic surgery. The lecture was well received. However, with the outbreak of the Great War, it was to be the last Semon lecture until 1921.

Fig. 2 Killian demonstrating his novel technique of suspension laryngoscopy, circa 1914. Reprinted with permission from Br Med J 1914;1:1181.Reference Killian 20
The outbreak of war across Europe severely curtailed Killian's travels, and his practice became increasingly dominated by the management of laryngeal and facial trauma.Reference Killian and Voss 21 His youngest son was a pilot on the Western Front, and this may have underpinned the devotion with which Killian attended the wounded. A tragic and ironic twist saw his son suffer terrible facial injuries during a plane crash. Killian hurried to the military hospital and personally operated on him, but sadly could do nothing to treat the meningitis which proved fatal to his son.Reference Zöllner 2
Despite the tragedy that had befallen him, Killian remained his cheerful and energetic self. His students called him the ‘semper ridens’ (‘always smiling’), and amongst his peers he was well regarded for his boyish enthusiasm and famous hospitality: the Black Forest trout served at his home in Freiberg even drew special mention in his obituary.Reference Dundas-Grant 9
-
• Gustav Killian was a prolific surgical innovator
-
• The true breadth and importance of his work is now often overlooked
-
• In 1897, he became the first person to perform a bronchoscopy
-
• This feat led to international acclaim and further innovations, many with modern applications
In 1921, Killian's contribution to the medical field was rewarded with two nominations for the Nobel Prize in medicine. Unfortunately, only a month after this nomination he fell ill and a rapid decline followed. He died from gastric cancer on 24 February 1921.
Killian's students Albrecht, Brünings and Seiffert all took professorships at notable German institutions and helped guide the further development of Killian's ideas, leading to further advances in instrumentation and technique which still influence our practice today. Bronchoscopy, endotracheal intubation and microlaryngoscopy are all everyday events in our working lives, and all can trace their origins to the pioneering spirit of this remarkable man.
We hope that readers will agree that there was indeed far more to Gustav Killian than just his eponymous dehiscence.
Acknowledgement
The authors would like to express their thanks to Miss A Savage BA(Hons) for her assistance with the translation of German manuscripts.