Introduction
Tonsillectomy is one of the most commonly performed procedures in ENT practice. The first tonsillectomy was described in 30 AD by Cornelius Celsus, a Roman surgeon, who used a hook to grasp the tonsil and then a fingernail to incise it.Reference Mathews, Lancaster, Sherman and Sullivan3 In the sixth century, a knife was used to remove the tonsil, a procedure known as dissection tonsillectomy, and this is still the most common method practised today. Various methods of tonsillectomy include guillotine, electrocautery, harmonic scalpel, radiofrequency ablation, laser, microdebrider and coblation techniques.
The debate regarding the best tonsillectomy technique continues to the present day. The National Prospective Tonsillectomy Audit showed that the relative risk of tonsillar haemorrhage, both primary and secondary, was reduced when ‘cold steel’ dissection was used.Reference Lowe, van der Meulen, Cromwell, Lewsey, Copley and Browne1, Reference Lowe and van der Meulen2 Morbidity, both intra- and post-operative, has always been a major concern, especially in terms of haemorrhage.
Materials and methods
The following description is based on work conducted at the department of otolaryngology, Poole Hospital National Health Service Foundation Trust.
For guillotine tonsillectomy, we used a Popper's haemostatic guillotine, Doyen mouth gag, Waugh forceps, McIndoe scissors, Boyle–Davis mouth gag, Jain tonsil ‘A’ frame,Reference Jain5 Jain insulated pillar retractor, bipolar diathermy and Yankauer sucker (Figure 1). A Popper's haemostatic guillotine has both crushing and cutting blades, which guide and pass across the fenestra of the guillotine (Figure 2).
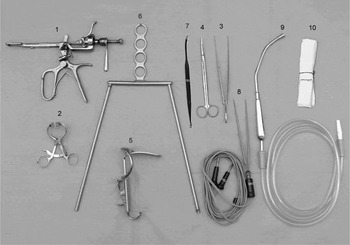
Fig. 1 Guillotine tonsillectomy instrument set. 1 = Popper's haemostatic guillotine; 2 = Doyen mouth gag; 3 = Waugh forceps; 4 = McIndoe scissors; 5 = Boyle–Davis mouth gag; 6 = Jain tonsil ‘A’ frame; 7 = Jain insulated pillar retractor; 8 = bipolar forceps; 9 = Yankauer sucker; 10 = tonsil swabs
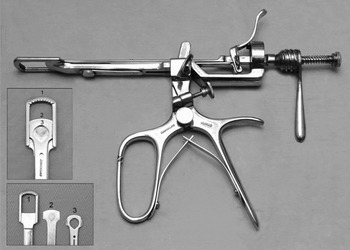
Fig. 2 Popper's haemostatic guillotine: 1 = Crushing blade; 2 = cutting blade; 3 = guillotine fenestra
Patients were laid in the Rose position (i.e. supine with neck hyperextended) under general anaesthesia (via endotracheal intubation or laryngeal mask). The mouth was kept open by engaging a Doyen gag on one side of the patient's mouth, to ensure that the tonsil and its surrounding tissue remained relaxed. This was so that the tonsils could be pushed through the guillotine fenestra with ease.
The guillotine was held in the right hand and inserted from the right side of the mouth when removing the left tonsil. The lower pole and the posterior border of the tonsil were engaged in the fenestra of the guillotine to draw the tonsil forward. The tonsil was pushed through the window of the guillotine with the left thumb over the anterior pillar (palatoglossal fold). At this stage, it was important to make sure that the whole tonsil had passed through the guillotine. The crushing fenestrated blade was then pushed down firmly. This dissected through the areolar tissue between the capsule of the tonsil and the superior constrictor muscle. This pressure was maintained and increased by rotating a screw applied to the crushing blade, thereby compressing and crushing the blood vessels supplying the tonsil. Clamping with the crushing blade was continued for at least two minutes. The cutting blade was then applied, by depressing a separate lever, and the tonsil removed. Occasionally, the tonsil remained thinly attached to the mucosa of the posterior pillar (palatopharyngeal fold), necessitating its careful dissection with scissors.
The right tonsil was removed in the same way by holding the guillotine in the left hand. The same technique was used in both children and adults.
After the procedure, the anterior and posterior pillars were often folded and temporarily adherent to one another, concealing bleeding points in between. Therefore, after the tonsil had been removed, a Boyle–Davis gag was inserted and suspended with the Jain tonsil ‘A’ frame,Reference Jain5 to enable better visualisation of the tonsillar fossae. The fossae were observed, once the pillars started to separate, in order to check for any tonsillar remnants, palatal trauma or bleeding points. Haemostasis was then achieved, if required, with bipolar diathermy forceps (8 W setting), by retracting the anterior pillar with the Jain insulated pillar retractor and drying any residual blood with tonsil swabs.
Tonsillectomy patients were not routinely followed up in our department. As such, care was taken at the time of surgery to check for tonsillar remnants and to note any palatal trauma, if present.
This summarises our ‘cold steel’ dissection technique; if needed, bipolar diathermy was used judiciously and sparingly, at a low power setting, only for haemostasis.
All patients who underwent day case tonsillectomy were contacted by the nursing staff on the following day, as per our standard unit protocol. Patients who stayed overnight were assessed in the morning on the ward round. Patients were advised to rest at home for two weeks post-operatively.
Results
We assessed retrospectively the notes of 168 patients who had undergone guillotine tonsillectomy for chronic or recurrent tonsillitis in our department between 2005 and 2007 inclusive. All operations were performed consecutively by the same surgeon (PKJ) on his routine operating list. The number of swabs used in each case, as documented in the notes, was recorded in order to estimate blood loss.
Of the 168 patients who underwent guillotine tonsillectomy, 52.4 per cent (n = 88) were under 16 years old and 47.6 per cent (80) were over 16 years old.
There was no measurable intra-operative bleeding in 13.1 per cent of cases (n = 22); therefore, no swabs, diathermy or suction were required in these cases. In 41.1 per cent (69) patients, bipolar diathermy (8 W) was used sparingly for haemostasis and less than two tonsil swabs were needed for haemostasis; no suction was used in these cases. Seventy-seven patients (45.8 per cent) required more than two tonsil swabs, and haemostasis was achieved with bipolar diathermy (8 W). No ties were required in any of the cases (Table I).
Table I Intra-operative haemorrhage during guillotine tonsillectomy, 2005–07

Pts = patients
Any complications encountered in this patient cohort should have presented locally to our hospital, as it was the only hospital serving ENT emergencies in the area.
There was one post-operative primary haemorrhage, which occurred in a 14-year-old girl who suffered with tonsillitis in the week prior to admission. She returned to theatre for haemostasis.
There were two cases of post-operative secondary haemorrhage. The first, a 34-year-old man, was readmitted five days post-operatively when he noticed blood on his pillow, and was subsequently managed conservatively on the ward. The second case was a 23-year-old man who was admitted five days post-operatively and required a return to theatre for haemostasis.
Thus, the primary haemorrhage rate was 0.6 per cent and the secondary haemorrhage rate 1.2 per cent (Table II).
Table II Post-operative haemorrhage after guillotine tonsillectomy, 2005–07

Pts = patients
Our study was limited by its retrospective nature. We were also unable to assess post-operative pain and return to normal activity.
Discussion
Guillotine tonsillectomy has been performed in various forms for over 100 years. A questionnaire study published in 2002 showed that 12.5 per cent of consultants still used this technique.Reference Mathews, Lancaster, Sherman and Sullivan3
The first instrument used for guillotine tonsillectomy was derived from the uvulotome, described in the Historiarum Anatomicarum Rariorum Centuriae of Thomas Bartholin.Reference Friedberg4 Since then, several modifications have been attempted by Physick, Mackenzie, Sluder and Popper. In the early twentieth century, guillotine dissection tonsillectomy became the standard treatment, but grew less popular in the latter half of that century due to persistent tonsillar remnants and excessive bleeding during and after the surgery.
Guillotine tonsillectomy was performed with ether inhalational anaesthesia without endotracheal intubation. Therefore, the whole procedure had to be quick and the second tonsil needed to be removed before the first started to bleed. The patients were then placed on their side and kept in the recovery room until natural haemostasis had occurred. A significant number of these patients subsequently returned to theatre still bleeding and required further haemostasis. Furthermore, due to the speed of the whole procedure there was a higher prevalence of tonsillar remnants and palatal trauma. We believe that the guillotine technique is now safer than in the past due to the advent of modern anaesthesia. As the airway is secure, the surgeon can better deal with bleeding, tonsillar remnants and palatal trauma at the time of surgery.
In order for the guillotine to be successful, loose areolar tissue is required between the tonsil and the constrictor muscle. Guillotine tonsillectomy is not possible in patients with severe fibrosis in the tonsillar fossae. Therefore, patients with small, fibrotic tonsils and a history of previous quinsy are not suitable for a guillotine procedure. Also, it is occasionally not possible to push very large tonsils through the guillotine fenestra completely.
In 1929, Popper described a series of tonsillectomies performed with his own haemostatic guillotine, with a reactionary haemorrhage rate of only 0.25 per cent.Reference McGuire6 In 1967, McGuire reported that careful and accurate use of the guillotine resulted in complete removal of the whole tonsil, leaving behind a clean, dissected tonsillar bed with minimal tissue trauma and intact faucial pillars.Reference McGuire6 In 1992, Roberts et al. confirmed guillotine tonsillectomy to be as effective as dissection tonsillectomy, with no higher incidence of post-operative haemorrhage.Reference Roberts, Jayaramachandran and Raine7
From our own experience, we too believe that guillotine tonsillectomy with Popper's guillotine is a safe and rewarding technique with less intra-operative bleeding and minimal post-operative morbidity. Proper training and expertise is required to make the best use of the guillotine method. Therefore, we advocate that present day ENT trainees, in addition to other techniques, should be exposed to this useful, simply mastered but neglected technique.
Acknowledgements
We would like to thank and acknowledge the help of our anaesthetist, Dr Roger Laishey, and also the ENT secretaries, day theatre and ward staff, admissions officers and medical photography department staff at Poole Hospital NHS Foundation Trust.






