Introduction
Branchial cleft cysts occur because of a failure of involution of the second branchial cleft at the end of the sixth or seventh week of embryogenesis.Reference Glosser, Pires and Feinberg1 The typical branchial cyst presents as a lateral cystic neck lump anterior to the sternocleidomastoid, at the junction between this muscle's upper and middle third. However, there is a lack of consensus on the appropriate management of adult cystic neck lumps due to a dearth of high quality evidence.
Differentiating benign from malignant cystic neck lumps can be challenging for the head and neck surgeon. This is evidenced from several reports of suspected branchial cysts treated with surgical excision only to be reported as cystic neck metastasis on final histology.Reference Glosser, Pires and Feinberg1, Reference Stanley2
Fine needle aspiration cytology (FNAC) is a well-utilised and useful initial tool in the management of neck lumps.Reference Stanley2, Reference Chang3 Fine needle aspiration cytology can correctly identify branchial cysts (Figure 1). However, the results of FNAC alone may be reported as equivocal (Figure 2), which is misleading as well-differentiated squamous cell carcinoma (SCC) (Figure 3) can mimic branchial cleft cysts cytologically and a definitive diagnosis is only made on final histology. Unfortunately, by this time, the patient may have been subjected to an incorrect procedure, which could potentially compromise the prognosis in patients with metastatic neck disease. Hence, FNAC is not ideal to establish a diagnosis of branchial cyst.
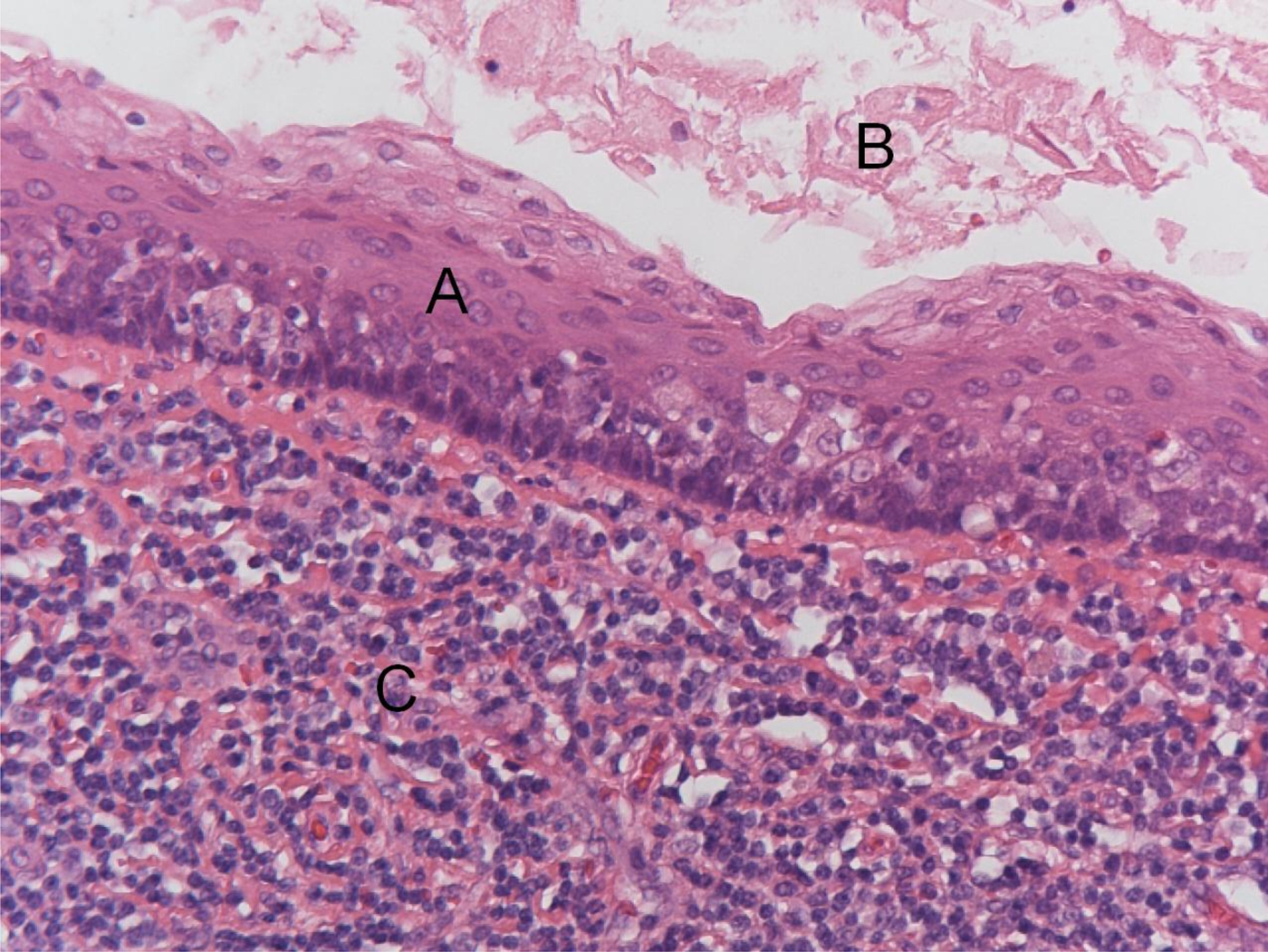
Fig. 1 Branchial cleft cyst – unequivocal fine needle aspiration cytology result. Field shows a cyst lined with normal benign squamous epithelium (A) that is filled with keratinous debris (B) and surrounded by lymphoid tissue (C). (H&E; ×200)
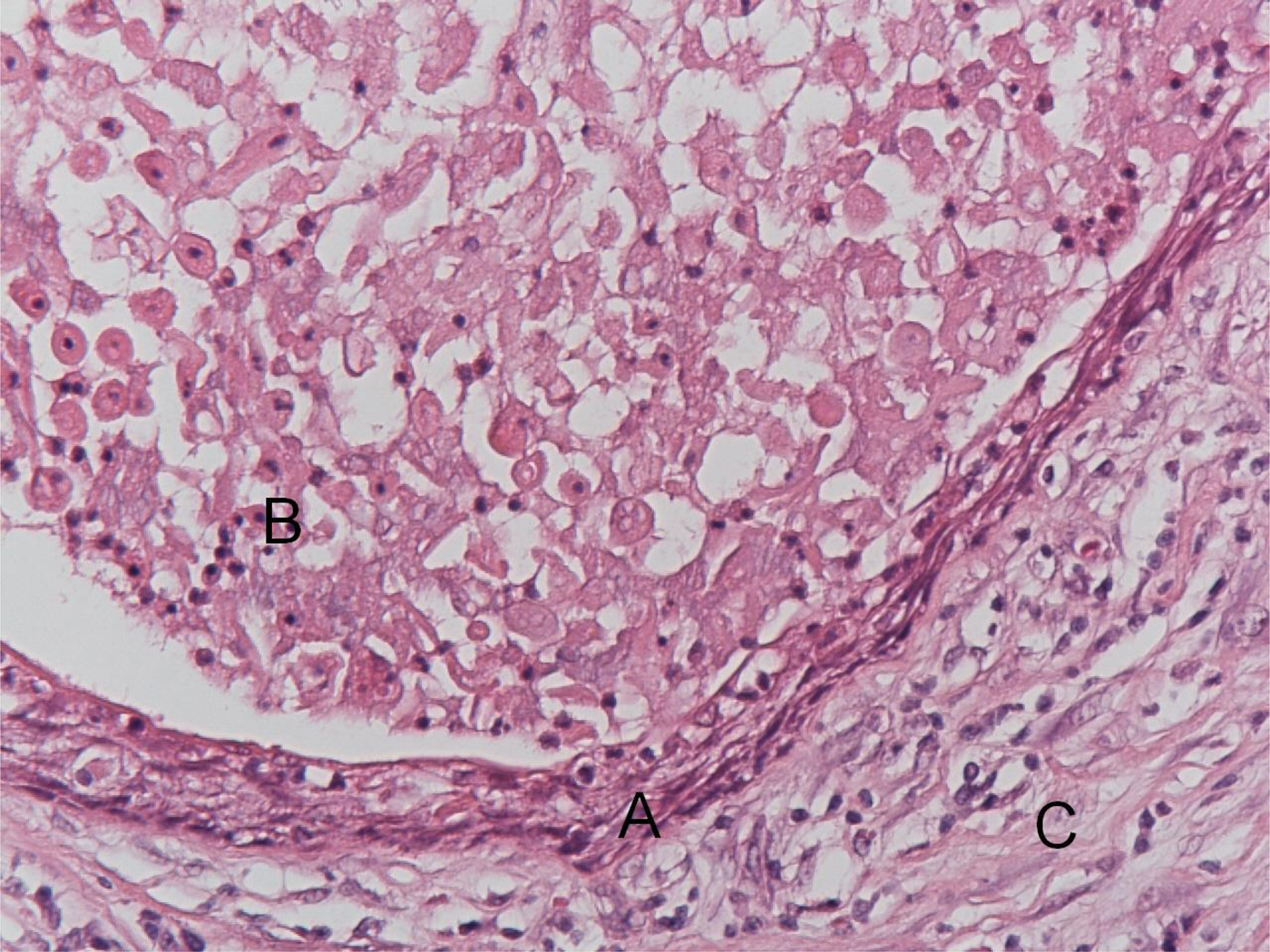
Fig. 2 Branchial cleft cyst – equivocal fine needle aspiration cytology result. Field shows: a cyst lined with squamous epithelium atypical in appearance (A), keratinous debris containing some squamous cells (B) and surrounding chronically inflamed stromal tissue (C). (H&E; ×200)
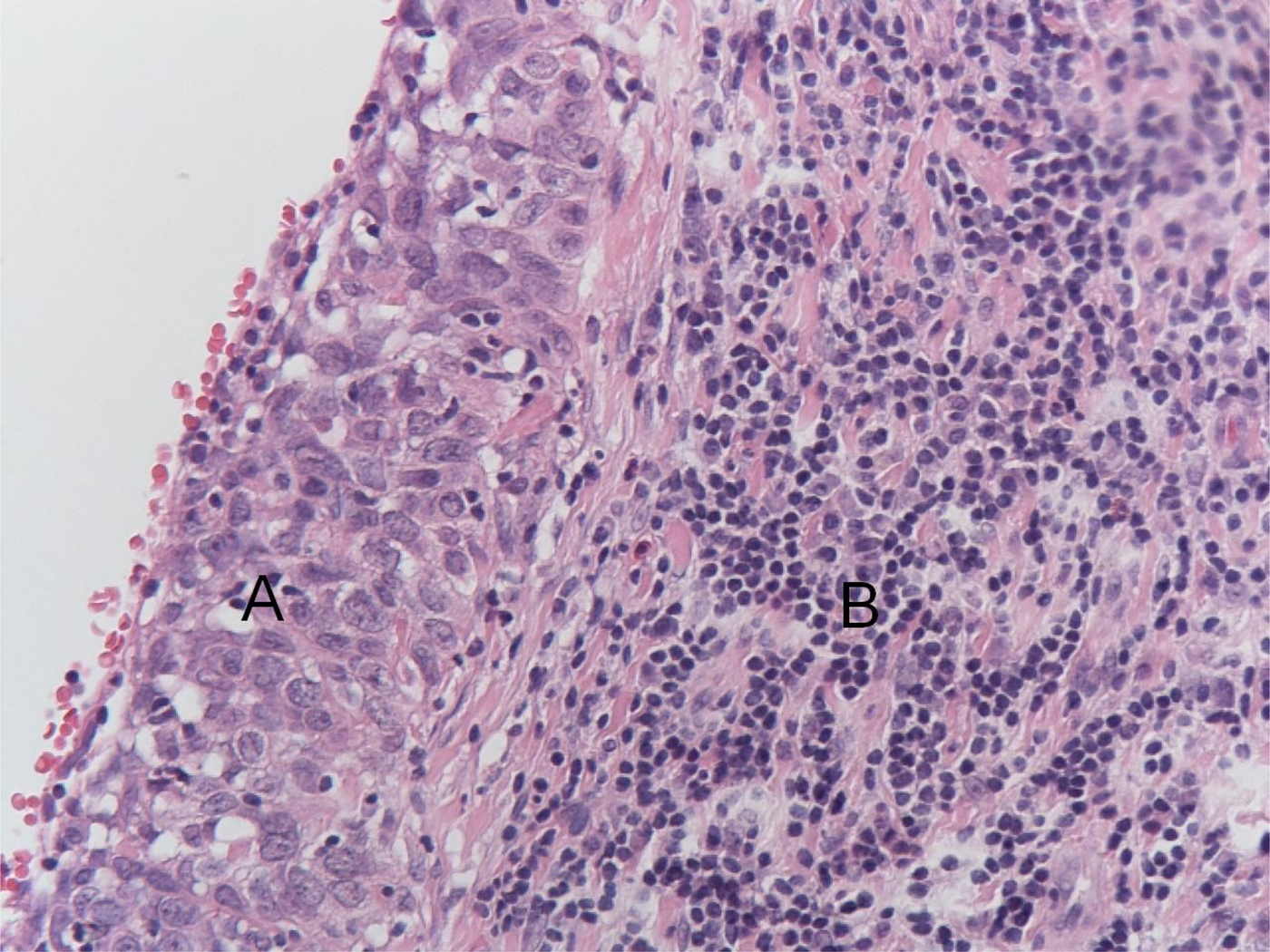
Fig. 3 Squamous cell carcinoma (SCC) – unequivocal fine needle aspiration cytology result. Field shows a cyst lined with frankly abnormal squamous epithelium (A) surrounded by lymphoid tissue (B) where cystic degeneration of SCC metastases has occurred. (H&E; ×200)
Frozen section analysis seems to be an under-utilised technique in this area. Frozen section can often assist the surgeon intra-operatively and aid appropriate management. Correct intra-operative diagnosis also means that patients undergo fewer invasive procedures. Studies have shown frozen section to have good a correlation with final histology; frozen section complements FNAC with regard to the diagnosis and management of thyroid and salivary gland lesions.Reference Mulcahy, Cohen, Anderson, Ditamasso and Schmidt4–Reference Mahe, Ara, Bishara, Kurian, Tauqir and Ursani6
On a background of such literature, this study aimed to report our experience of FNAC and frozen section analysis in the management of lateral cystic neck lumps. Specifically, we analysed the correlation between FNAC and frozen section with formal histology in patients with a clinical diagnosis of branchial cyst.
Materials and methods
A retrospective analysis was conducted of all patients diagnosed with branchial cyst on FNAC or formal histology between 2003 and 2012 at the Department of Otolaryngology, Southern General Hospital, Glasgow (Scotland, UK).
Patient demographics, FNAC, frozen section and formal histology data were reviewed. The correlation between pathology reports was analysed, and the sensitivity and specificity for FNAC and frozen section analysis in the diagnosis of branchial cyst were calculated.
Results
Sixty-eight cases were initially identified, of which 38 were excluded in light of unavailable clinical data and/or a diagnosis other than branchial cyst. Therefore, a total of 30 cases were eligible for analysis. Table I outlines the demographics and pathological diagnoses made via each modality in each case.
Table I Demographic characteristics and pathological diagnoses
*Non-smoker. FNAC = fine needle aspiration cytology; M = Male; F = Female; SCC = squamous cell carcinoma
Patient ages ranged from 19 to 86 years old, with a mean age of 41.9 years. There were 22 males (73.3 per cent) and 8 females (26.7 per cent).
Formal histology reports were available for all cases. On formal histology, a diagnosis of branchial cleft cyst was made in 25 cases (83.3 per cent), Warthin's tumour in 2 cases (6.7 per cent), reactive lymph node in 2 cases (6.7 per cent) and metastatic SCC in 1 case (3.3 per cent).
The FNAC reports were available for 28 cases (93.3 per cent). On FNAC, a diagnosis of branchial cleft cyst was suggested in 26 cases (92.9 per cent); the findings were inconclusive in 1 case (3.6 per cent) and raised suspicion of metastatic SCC in 1 case (3.6 per cent).
Frozen section reports were available for eight cases (26.7 per cent). On frozen section, a diagnosis of branchial cleft cyst was made in seven cases (87.5 per cent) and Warthin's tumour in one case (12.5 per cent).
The results for both FNAC and formal histology were available for 28 cases. Twenty-one (80.8 per cent) of 26 cases that had an FNAC diagnosis of branchial cleft cyst also had a formal histology diagnosis of branchial cleft cyst. Two cases had a final diagnosis of Warthin's tumour. In a further two cases, reactive lymphadenopathy was the final diagnosis.
We would like to highlight two cases in our series. Case 19, with an FNAC diagnosis of branchial cleft cyst, had a diagnosis of metastatic SCC on formal histology. The FNAC findings for the other case (case 30) suggested metastatic SCC, whereas the formal histology revealed a branchial cleft cyst.
In our series, the overall sensitivity of FNAC for detecting branchial cleft cysts was 75 per cent. There were no true negative reports; therefore, the specificity could not be calculated. All seven cases that had a frozen section diagnosis of branchial cleft cysts had formal histology confirming the same. In the other case for which frozen section data were available, a diagnosis of Warthin's tumour was confirmed on final histology. Thus, the sensitivity of frozen section for detecting branchial cysts was 100 per cent.
Discussion
The historical dilemma surrounding the diagnosis of adult cystic lateral neck lumps remains. In clinical practice, differentiating branchial cleft cysts from cystic metastatic SCC is paramount for optimal management and a successful outcome for patients.
The most common cause of a cystic neck swelling in younger patients (those aged less than 40 years) is a branchial cyst.Reference Pietarinen-Runtti, Apajalahti, Robinson, Passador-Santos, Leivo and Mäkitie7 In a review of 121 patients with lateral neck cysts, nearly 10 per cent of all patients had a malignant deposit identified within the cyst. This figure rose to 23.5 per cent if patients were over 40 years old.Reference Cinberg, Silver, Molnar and Vogl8
The results from our case series differ from those reported in the literature. Fourteen patients aged over 40 years had branchial cleft cysts, compared with only 11 patients aged less than 40 years. However, in those aged less than 40 years, 11 of 13 benign swellings were indeed branchial cysts. The mean age of patients with branchial cleft cysts was 40.6 years. This is a higher mean age than previously reported and shows that branchial cysts can present at a later age. Nevertheless, we recommend that any patient aged over 40 years who presents with a lateral neck lump is investigated as having a metastatic node until proven otherwise. Notably, one patient from our cohort who had a final diagnosis of SCC was only 34 years old. As human papillomavirus (HPV) is widely recognised as being a distinct aetiological factor in head and neck SCC, it is likely that clinicians will encounter more patients of a different demographic profile, including young, non-smoking adults.
Cystic metastatic neck lumps are usually considered the hallmark of HPV related SCC with an oropharyngeal primary lesion.Reference Goldenberg, Begum, Westra, Khan, Sciubba and Pai9 Theories explaining the pathogenesis of cysts in nodal metastasis include: pseudocystic change resulting from spontaneous degradation of keratin and cellular debris, within a carcinomatous lymph node deposit; and the occurrence of a true cyst lined by neoplastic epithelium in the central portion of a lymph node, with lymphoid elements occupying the periphery.
The existence of carcinoma within a branchial cyst (primary branchiogenic carcinoma) has been disputed. Although there have been reports of primary branchiogenic carcinoma, many cases do not fulfil the original criteria described by Martin et al. in 1950.Reference Martin, Morfit and Ehrlich10 In fact, some authors actually challenge the original criteria itself, encouraging clinicians to abandon the term branchiogenic carcinoma as a differential diagnosis of cystic metastatic SCC.Reference Wolff, Rankow and Fliegel11, Reference Raghavan and Bradley12 It must be noted that if there exists a true diagnosis of primary branchiogenic carcinoma, at best its incidence is very rare.
Fine needle aspiration cytology is a relatively simple technique with proven utility in the diagnosis of solid head and neck lesions, with low false positive and false negative rates. However, its efficacy in the diagnosis of cystic neck lesions is suboptimal because of hypocellular aspirate.Reference Sheahan, O'Leary, Lee and Fitzgibbon13, Reference Rapidis, Faratzis, Lagogiannis and Koutsoubi14 The sensitivity of FNAC in the diagnosis of cystic nodal metastasis is reported to be between 33 and 50 per cent, which makes it an unacceptable tool to rely on. We report 75 per cent sensitivity with FNAC in diagnosing branchial cysts.
More recently, DNA analysis using flow cytometry to evaluate cell aneuploidy in FNAC samples has been evaluated as a method to help distinguish branchial cysts from metastatic SCC.Reference Nordemar, Tani, Hogmo, Jangard, Auer and Munck-Wikland15 However, more evidence is required before this technique becomes common practice.
Intra-operative frozen section tissue examination is a well-utilised technique for tumours within the head and neck. However, the literature on the role of frozen section examination in the management of suspected branchial cysts is scarce. In our series, we report a 100 per cent sensitivity of frozen section in identifying branchial cysts.
Our data also show that FNAC is much less reliable in the diagnosis of branchial cleft cysts than frozen section, with sensitivities of 75 per cent and 100 per cent, respectively. The FNAC findings did not correlate with formal histology in two cases. In one case, the FNAC gave a false positive result for branchial cleft cyst where formal histology revealed a metastatic SCC. In the other, FNAC gave a false positive result for SCC where formal histology revealed a branchial cleft cyst. In both cases, frozen section examination was not performed and the patients received suboptimal treatment. In the first case, the patient required further surgery, which also meant a delay in definitive treatment. In the second case, the patient underwent an unnecessary neck dissection. Along with patient anxiety and distress, these cases highlight medico-legal implications that a clinician could encounter. It is possible that frozen section analysis of the specimen in each case may have prevented these adverse events.
One possible explanation for the under-utilisation of frozen section in the management of such patients could be the potential discordance between frozen section results and final pathology. The literature reports discordance rates between 1.4 and 12.9 per cent.Reference Teichmann, Rost, Thieme and Petersen16–Reference White and Trotter18 Reasons for such errors include diagnostic misinterpretation, tissue samples that are not representative of underlying pathology, or technical issues such as uneven staining. We did not observe this in any of our patients, and recommend close liaison with a specialist head and neck pathologist both pre- and intra-operatively to minimise such errors.
Because of the lack of consensus on the management of lateral cystic neck lumps in patients aged over 40 years, treatment approaches vary. The recommended treatment for branchial cysts is surgical excision because of their propensity to enlarge and become infected. However, the management of cystic metastatic SCC is contentious. It is agreed that the clinical investigation must include a thorough examination of the head and neck, followed by FNAC and appropriate cross-sectional imaging, as recommended by the head and neck national guidelines in both Britain and the USA.19, 20 Fine needle aspiration cytology suggesting a malignant lesion warrants a panendoscopy and biopsy of suspicious areas, including unilateral or bilateral tonsillectomy, with the aim of locating the primary tumour.
• Management of adult lateral cystic neck lumps can pose diagnostic challenges, as well-differentiated squamous cell carcinoma (SCC) can mimic branchial cleft cysts
• Fine needle aspiration cytology is often used in neck lump management, but findings can be misleading in human papillomavirus associated cystic neck metastasis cases
• Adults subjected to excision of a suspected branchial cyst should undergo intra-operative frozen section analysis regardless of clinical suspicion of malignancy
• Confirmation of SCC intra-operatively should necessitate neck dissection and this should be discussed with the patient pre-operatively
Earlier reports concur with the use of intra-operative frozen section in the management of cystic neck lumps.Reference Andrews, Gidding and Su21 If the specimen is found to contain carcinoma, the surgeon should proceed with a formal neck dissection, and, in this regard, appropriate pre-operative counselling with the patient is important. Post-operative radiotherapy in such patients depends on the final histology and the decision of the local head and neck multidisciplinary team.
Conclusion
We recommend that adult patients subjected to surgical excision of a suspected branchial cyst undergo intra-operative frozen section analysis regardless of clinical suspicion for malignancy. Just one quarter of cases in our series had frozen section analysis performed. This part of management is crucial to ensure patients are offered the right management within the right time frame. It also avoids unnecessary patient anxiety and distress due to mismanagement, and may prevent litigation. In addition, for those patients where FNAC suggests malignancy, appropriate measures should be taken to locate a primary tumour prior to definitive treatment.






