Introduction
Inferior turbinate hypertrophy is a frequent cause of nasal airway obstruction. One of the commonest non-infectious causes of inferior turbinate hypertrophy is compensatory hypertrophy due to long-standing nasal septum deviation, persistent allergic rhinitis or idiopathic rhinitis.Reference Lai and Corey 1 , Reference Li, Powell, Riley, Troell and Guilleminault 2 Recent studies have provided evidence that inferior turbinate hypertrophy is more often due to conchal bone hypertrophy than mucosal hypertrophy.Reference Berger, Hammel, Berger, Avraham and Ophir 3 , Reference Rohrich, Krueger, Adams and Marple 4 None of the studies on compensatory inferior turbinate hypertrophy have compared patients with traumatic and congenital septal deviations.
We hypothesised that the aetiology of the septal deviation (congenital or traumatic) altered its duration and thus influenced the degree of turbinate mucosal hypertrophy and conchal bone development which occurred in reaction.
Based on this hypothesis, we compared mucosal and bony measurements in patients with congenital and traumatic nasal septum deviation and compensatory inferior turbinate hypertrophy.
Materials and methods
The hospital's institutional review board approved the procedure described in this study.
We included in the study patients who had a confirmed diagnosis of severe anterior septal deviation and who were expected to undergo septoplasty. We confirmed the presence of nasal septum deviation initially detected via endoscopy, using computed tomography (CT) scanning of the sinuses.
We excluded patients with allergic rhinitis, nonallergic rhinitis with eosinophilia, acute and chronic sinusitis, nasal polyposis, antrochoanal polyps, and those who had recently used systemic or topical decongestants or nasal steroids. We also excluded any patient with a history of previous nasal surgery, with an uncertain trauma history, with trauma suffered before the age of 17 years (as such trauma may affect bone development), and without severe anterior septal deviation confirmed by CT. In the traumatic group, we excluded any patient with similar complaints before their trauma. All the patients in the traumatic group had septal cartilage fracture visible at operation.
Severe, unilateral, anterior nasal septum deviation was observed in all patients, using a nasal endoscope and speculum.
We took pre-operative CT scans of the paranasal sinuses using continuous scanning from anterior to posterior and using 3 mm slices in the coronal plane. All measurements were obtained at the level of the anterior osteomeatal unit, which includes the ethmoid bulla, uncinate process, primary ostium of the maxillary sinus, infundibulum and middle meatus. To facilitate the measurement process, three vertical lines were superimposed on the CT scans: a median line extending from the crista galli to the anterior nasal spine; and, parallel to this, two lateral lines running through the point at which the base of the inferior turbinate abuts the maxillary sinus, bilaterally. The six measurements defined in Table I and illustrated in Figures 1, 2 and 3 were measured for both the concave and convex sides of the nasal septum, for all CT scans.
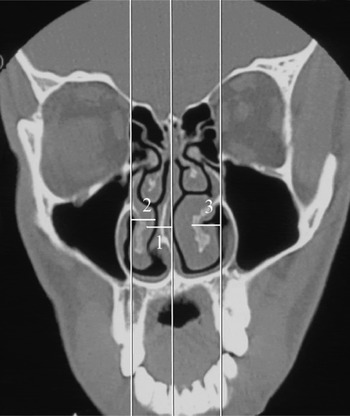
Fig. 1 Coronal computed tomography section through the anterior portion of the inferior turbinate, showing the first, second and third measurements.

Fig. 2 Coronal computed tomography section through the anterior portion of the inferior turbinate, showing the fourth measurement.
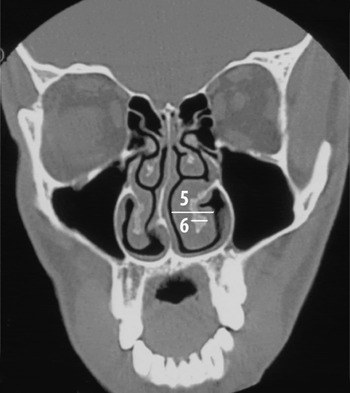
Fig. 3 Coronal computed tomography section through the anterior portion of the inferior turbinate, showing the fifth and sixth measurements.
Table I Measurements used

*Line from crista galli to anterior nasal spine. †Line running parallel to median line and crossing the point where the inferior turbinate origin abuts the maxillary sinus. ‡Including the conchal bone and medial and lateral mucosa. Msmt = measurement
Statistical studies
We performed statistical analyses using the Number Cruncher Statistical System 2007 and the Power Analysis and Sample Size 2008 statistical software programs (Kaysville, Utah, USA). Statistical significance was determined using Student's t-test and the Mann–Whitney U test. A p value of less than 0.05 was considered significant.
Results
The study enrolled a total of 64 patients.
Fourteen patients were subsequently excluded from the study (10 patients from the traumatic group and four from the congenital group), for the following reasons. Seven patients from the traumatic group and three from the congenital group had septal deviation endoscopically but did not show a severe anterior septal defect on sinus CT. Three patients from the traumatic group had insufficient information about their trauma history. One patient from the congenital group sustained a fracture of the septum during surgery.
The study included the remaining 50 evaluable patients (Figure 4). The congenital septal deviation group consisted of 25 patients (19 men and six women) between 18 and 47 years of age (mean age, 27 years). In this group, left- and right-sided septal deviation was found in 11 and 14 patients, respectively. The traumatic sepal deviation group consisted of 25 patients (18 men and seven women) aged between 18 and 54 years (mean age, 30 years). In this group, left- and right-sided septal deviation was found in 12 and 13 patients, respectively. Table II shows mean values for the six measurements recorded, for both concave and convex sides, in both groups.

Fig. 4 Flowchart showing the patient selection process.
Table II Measurements by group

*p < 0.01, Student t-test. Msmt = measurement; SD = standard deviation; grp = group
Table III shows the difference in measurements between the concave and convex sides, for the two groups. When the concave–convex measurement differences of the congenital and traumatic groups were compared, statistically significant differences between the groups were noted for the first, third and fourth measurements.
Table III Difference in concave vs convex side measurements, by group

*p < 0.05; † p < 0.01; Mann-Whitney U test.
Discussion
Hypertrophy of the inferior turbinates results in increased nasal airway resistance and contributes to symptoms of nasal obstruction.Reference Egeli, Demirci, Yazici and Harputluoglu 5 , Reference Berger, Gass and Ophir 6 Turbinate enlargement can occur congenitally, or secondarily to conditions such as vasomotor rhinitis, allergic rhinitis or chronic hypertrophic rhinitis.Reference Pollock and Rohrich 7 , Reference Courtiss, Goldwyn and O'Brien 8 Three variations are encountered: bony, soft tissue and mixed hypertrophy. It is generally believed that most inferior turbinate enlargement is due to mucosal hypertrophy; however, in patients with septal deviation, enlargement of the contralateral inferior turbinate involves both mucosal and bony elements.Reference Hilberg, Grymer, Pedersen and Elbrønd 9 In patients with anterior septal deviations, contralateral compensatory inferior turbinate hypertrophy is commonly observed. Correction of the septal deviation narrows the nasal cavity on the contralateral side; therefore, if compensatory turbinate hypertrophy on that side goes untreated, nasal obstruction may persist. For this reason, septoplasty is commonly performed together with turbinectomy.
Septal deviation occurs either congenitally or due to trauma later in life. A cartilaginous nasal capsule surrounds the nasal cavity and is continuous with the cartilage of the nasal septum. Three preturbinates (inferior, middle and superior) appear within the nasal cavity at eight weeks' gestation.Reference Bingham, Wang, Hawke and Kwok 10 Anterior cartilage deviation occurs more commonly in newborns delivered vaginally than in those delivered via caesarean section. Combined septal deformity involves all septal components, and includes compensatory turbinate hypertrophy opposite the side of the deviation.Reference Neskey, Eloy and Casiano 11 During pregnancy, the fetus is subject to various torsions and pressures. Depending on the severity and location of these pressures, local deformities may develop, including anterior septal deviation. Posterior deformities of the septum have a genetic component or may be related to maxillary complex development, whereas anterior deformities are usually caused by extrinsic forces.Reference Grymer, Pallisgaard and Melsen 12 Nasal septal deviation is often associated with unilateral concha bullosa, which occupies the expansive space of the contralateral nasal cavity. Compensatory inferior turbinate hypertrophy can also coexist with congenital nasal septal deviation.
The literature reports various surgical techniques for the treatment of turbinate hypertrophy, including total or partial turbinectomy, turbinoplasty, submucous resection, cryosurgery, laser-assisted turbinectomy, injection of corticosteroids or sclerogenic substances, submucosal diathermy, and radiofrequency reduction.Reference Gupta, Mercurio and Bielamowicz 13 , Reference Rakover and Rosen 14
Despite this wide range of techniques, indications for turbinectomy remain unclear. When choosing a turbinectomy technique, the bony and mucosal parts of the turbinate should be considered separately. Few studies of the use of turbinectomy to treat septal deviation and contralateral inferior turbinate hypertrophy have discussed the indications for the various types of turbinectomy (e.g. submucosal resection or partial or complete conchal resection).Reference Egeli, Demirci, Yazici and Harputluoglu 5 , Reference Berger, Gass and Ophir 6 , Reference Fairbanks, Kaliner, Cummings, Fredrickson, Harker, Krause, Richardson and Schuller 15 , Reference Jun, Kim, Kim, Cho, Park and Yoon 16
Fairbanks and Kaliner describe both mucosal and bony enlargement in cases of compensatory inferior turbinate hypertrophy.Reference Fairbanks, Kaliner, Cummings, Fredrickson, Harker, Krause, Richardson and Schuller 15
Berger et al. studied specimens from 19 patients undergoing nasal surgery for septal deviation and contralateral inferior turbinate hypertrophy, compared with 10 inferior turbinates removed at autopsy and used as controls.Reference Berger, Hammel, Berger, Avraham and Ophir 3 They found that inferior turbinate hypertrophy was caused by conchal bone hypertrophy rather than medial and lateral mucosal hypertrophy. However, these study findings were limited by difficulty in determining mucosal hypertrophy in postmortem specimens.
Egeli et al. found that compensatory turbinate hypertrophy was due to both conchal bone enlargement and medial and lateral mucosal hypertrophy.Reference Egeli, Demirci, Yazici and Harputluoglu 5
Jun et al. found thicker conchal bone, greater medial and lateral mucosal depth, and a greater inferior turbinate projection angle, comparing inferior turbinates on the concave versus convex sides of patients with nasal septal deviation.Reference Jun, Kim, Kim, Cho, Park and Yoon 16 However, data were insufficient to determine whether these compensatory bony and mucosal changes differed in patients with traumatic versus congenital septal deviation.
In the current study, we attempted to determine whether compensatory inferior turbinate hypertrophy differed in these two patient groups. We believed that this data, not previously available, would assist otolaryngologists in choosing the best type of turbinectomy with which to treat compensatory inferior turbinate hypertrophy due to either congenital or traumatic nasal septal deviation.
We found that the shortest mean distances (± standard deviation) from the median line to the medial border of the conchal bone on the concave and convex sides were respectively 6.94 ± 1.53 and 8.86 ± 1.37 mm in the traumatic group and 6.33 ± 1.23 and 9.21 ± 1.40 mm in the congenital group. Similarly, the shortest distance from the medial border of the conchal bone to the lateral nasal line on the concave and convex sides were respectively 7.84 ± 2.14 and 6.28 ± 2.08 mm in the traumatic group and 7.95 ± 1.44 and 4.90 ± 1.35 mm in the congenital group.
-
• Nasal septum deviation commonly causes contralateral compensatory inferior turbinate hypertrophy
-
• Septal deviation may be traumatic or congenital in origin
-
• In the latter, the conchal bone has more effect on nasal patency
-
• Findings support turbinate bone resection at the time of septoplasty in congenital cases
The projection angle of the inferior turbinate on the concave side was 4° wider than on the convex side in the traumatic group, and 18° wider in the congenital group. This finding indicates that the hypertrophic inferior turbinate bone occupies a significantly larger space within the nasal cavity in the congenital group, compared with the traumatic group.
We found no statistically significant differences between the traumatic and congenital cases as regards differences between the second and fifth measurements on the convex versus concave sides. These findings suggest that traumatic septal deviations occurring later in life cause compensatory changes involving only the turbinate mucosa.
Kim et al. found a significant reduction in the mucosal thickness of compensatory inferior turbinate hypertrophy, one year after septoplasty.Reference Kim, Park, Kim, Kang, Park and Han 17 Considering that the turbinate bone does not occupy as much space in the nasal cavity of patients with traumatic septal deviation (compared with congenital cases), post-operative reduction of mucosal hypertrophy following septoplasty eliminates the need for turbinate intervention. However, in patients with congenital septal deviation we consider it essential to remove the hypertrophic inferior turbinate bone at the time of septoplasty. On the other hand, outfracture of the inferior turbinate reduces the projection angle of the compensatory hypertrophic inferior turbinate and improves nasal patency when performed together with surgical reduction of the medial and inferior mucosal volumes of the hypertrophic inferior turbinate.
Conclusion
In the present study of patients with unilateral nasal septum deviation and contralateral compensatory inferior turbinate hypertrophy, those with congenital septal deviation showed a marked influence of the conchal bone on nasal patency. These findings support excision of the inferior turbinate bone at the time of septoplasty, when treating patients with congenital septal deviation and compensatory inferior turbinate hypertrophy. In patients with traumatic septal deviation and contralateral inferior turbinate hypertrophy, mucosal changes are more prevalent than bony changes; therefore, bone resection may be unnecessary in these cases.









