Introduction
Demographic data recorded over the last few decades indicate an increase in life expectancy, partly due to advances in medical care. This increase, together with a decrease in the birth rate, has resulted in an ageing population, with a proportionately greater need for social and economic integration. These changes require modifications in society's approach to individual and collective health. In this context, hearing loss in the elderly, or presbyacusis, is becoming an increasingly frequent problem, requiring a more targeted approach and the development of new therapeutic alternatives.
Presbyacusis is loss of the ability to perceive or define sounds due to the ageing process.Reference Stedman1 It is the most common cause of hearing deficiency in adults, affecting approximately 31 per cent of individuals between 60 and 69 years of age.Reference Agrawal, Platz and Niparko2
Presbyacusis characteristically manifests as sensorineural hearing loss, developing insidiously and symmetrically in both ears and progressing with age, without the development of any other ear problems.Reference Schuknecht and Gacek3
Current treatment basically consists of hearing rehabilitation using personal hearing aids. Despite being a well established and widespread technology undergoing continual improvement, hearing aids still have low acceptance. In a notable cohort study, only 10 per cent of elderly individuals who could have benefited from hearing aids used them regularly.Reference Gates, Cooper, Kannel and Miller4 Another study found that only 14.6 per cent of elderly patients with some degree of hearing loss used hearing aids.Reference Popelka, Cruickshanks, Wiley, Tweed, Klein and Klein5 This proportion rose to 55 per cent in cases of severe hearing loss. Low adherence was related to financial, psychological and social issues.
Presbyacusis occurs due to cell ageing in conjunction with a series of cumulative factors such as noise exposure, systemic disease, drug treatment and genetic factors. Nevertheless, its exact aetiopathogenic mechanism has not yet been fully established.Reference Bared, Ouyang, Angeli, Du, Hoang and Yan6
The proposed aetiological theories attribute a central role to the action of free radicals. Moreover, studies have shown that free radicals are involved in several clinical conditions affecting the cochlea, such as ischaemia, noise-induced hearing loss and ageing.Reference Seidman7
Various antioxidants have been described in the literature as being beneficial for several clinical conditions, such as vitamin E for the control of arteriosclerosis and the treatment of sudden hearing loss, α-lipoic acid for diabetes, and ginkgo biloba for neurodegenerative disease.Reference Byers and Bowman8–Reference Mahadevan and Park11
Control of hearing damage associated with oxygen free radicals has been experimentally demonstrated in animal models. The use of antioxidants has been shown to correlate with improved responses in brainstem auditory evoked potentials and a reduction in mitochondrial DNA deletions, compared with a placebo.Reference Seidman7 In a canine model, dietary antioxidant supplements were associated with decreased auditory neuronal cell degeneration, compared with animals fed a typical diet.Reference Le and Keithley12
For some time now, alternatives to the usual rehabilitation with hearing aids have been sought, and positive results have recently been published. The effects on auditory processing of citalopram, a serotonin reuptake inhibitor, have recently been tested in patients with presbyacusis. In comparison to a placebo group, two out of three auditory processing tests demonstrated statistically significant improvement after treatment.Reference Cruz, Kasse, Sanchez, Barbosa and Barros13 Another study, assessing the effect of folic acid supplements on the auditory threshold of elderly individuals, found a significant difference between subjects receiving supplements versus placebo.Reference Durga, Verhoef, Anteunis, Schouten and Kok14 A further study tested the effects of antioxidants in 46 individuals with diagnosed presbyacusis who took a combination of rebamipide, vitamin C and α-lipoic acid for at least 8 weeks.Reference Takumida and Anniko15 Hearing improvement was detected, especially at low frequencies (i.e. 125, 250 and 500 Hz) and at 8000 Hz, while discrete improvement was detected at 1000, 2000 and 4000 Hz and general improvement was detected in the average threshold for these frequencies.Reference Takumida and Anniko15
The current study aimed to evaluate the effect of antioxidant treatment on the hearing threshold of patients with diagnosed presbyacusis, over a longer treatment period than that assessed by most previous studies. We also aimed to report any additional benefits or adverse events which arose during the study.
Materials and methods
This study was approved on 2 July 2010 by the ethics committee of our institution (protocol number CEP 0723/10). The trial was registered with the International Clinical Trials Registry Platform of the World Health Organization (see http://apps.who.int/trialsearch/trial.aspx?trialid=ACTRN12610000667011).
The initial sample group comprised 120 patients selected from patients treated at the Center for Auditory Deficiency, who agreed to participate in the study by signing an informed consent form. Selected individuals were 60 years of age or older and had a clinical and audiological diagnosis of presbyacusis. Patients with known allergies to any of the test substances, or contraindications to the use of the test substances, were excluded. We thus excluded patients with coagulopathy or diabetes, as well as those requiring anticoagulant therapy. We also excluded patients exhibiting other possible causes of hearing loss, such as long-lasting occupational noise exposure or a history of ear disease affecting hearing.
A detailed historical record (including comorbidity, previous hospitalisation, and current or previous medication) was collected from all participants, in order to control for the possible adverse effects of treatments and drug interactions.
Patients received medication for six months. After allocation to one of four treatment groups, they received one of the following treatments: ginkgo biloba (dry extract, 120 mg/day), α-lipoic acid (60 mg/day) plus vitamin C (600 mg/day), papaverine chlorhydrate (100 mg/day) plus vitamin E (400 mg/day), or placebo (starch pills).
Patient allocation to the treatment groups was randomised using a spreadsheet generated at a randomisation website (http://www.randomization.com). The four treatments were prepared by a pharmacist in vials identified with the letters A, B, C and D; neither the patients nor the researchers were aware of the contents of treatment vials, for the duration of the study.
The treatments were supplied to participants free of charge, and were financed by research funds from the Center for Auditory Deficiency. Treatment agents were distributed every two months, at the same time as participants underwent medical assessments and interviews focussing on possible adverse treatment effects and drug interactions.
Audiology evaluations were performed by an audiologist who was blinded both to the subject's treatment agent and to their results for previous examinations. Audiological evaluation included pure tone audiometry, impedance audiometry, and assessment of speech recognition threshold and percentage index of speech recognition. The initial audiological evaluation results were used as a baseline for assessment of subsequent treatment effects. Audiological evaluation was also performed after six months of treatment to assess the possible effects of therapy. The frequencies assessed were 250, 500, 1000, 2000, 3000, 4000, 6000 and 8000 Hz. Hearing improvement was defined as an increase of 10 dB or more at isolated and average frequencies; increases of less than 10 dB and decreases of 10 dB or less were rated as non-significant, and decreases of more than 10 dB were rated as deterioration in hearing.
The statistical analysis of all study data was initially descriptive. For quantitative (numerical) variables, some summary measures were calculated, such as the mean, median, range and standard deviation. Qualitative (categorised) variables were analysed by calculating absolute and relative frequencies (expressed as percentages).
The inferential analyses used to confirm or refute evidence emerging in the descriptive analysis were as follows.
Pearson's chi-square test, Fisher's exact test or its extension was used to study the association of profiles among the four treatment groups (i.e. ginkgo biloba, α-lipoic acid plus vitamin C, papaverine chlorhydrate plus vitamin E, and placebo) according to sex, schooling, occupation, smoking habits, alcohol habits, systemic arterial hypertension, dyslipidaemia, heart disease, hypothyroidism, osteoporosis, joint disease, benign prostatic hyperplasia, other comorbidities, hearing risk, otoscopy, completion of treatment, and reasons for not completing the study (the latter only for patients who did not complete treatment).
Variance analysis with fixed factors was used to compare the profiles of the four treatment groups according to age, number of medications and duration of hearing loss.
Variance analysis with repeated parametric measures was used to compare the profiles of the four treatment groups before and after treatment, for the frequencies 250, 2000, 6000 and 8000 Hz, expressed as scores.
Finally, variance analysis with repeated non-parametric measures was used to compare the profiles of the four treatment groups before and after treatment, for the frequencies 500, 1000, 3000 and 4000 Hz, the speech recognition threshold and the percentage index of speech recognition, expressed in degrees.
For all conclusions obtained through inferential analysis, the level of significance (α) was established at 5 per cent. Data were recorded in Excel for Windows 2010 spreadsheets to ensure proper information storage. Statistical analyses were performed using SPSS (version 19.0 for Windows) and R-Program (version 2.11.1) software.
Results
The study group comprised 120 individuals allocated randomly to four treatment groups: ginkgo biloba (120 mg), α-lipoic acid (60 mg) plus vitamin C (600 mg), papaverine chlorhydrate (100 mg) plus vitamin E (400 mg), and placebo. A total of 30 individuals were allocated to each group.
Notably, all four groups exhibited profiles that were statistically similar regarding sex (p = 0.574), age (p = 0.093), schooling (p = 0.299), occupation (p = 0.266), smoking habit (p = 0.974), alcohol habit (p = 0.339), complaints of tinnitus (p = 0.731) and number of medications used (p = 0.151) (Table I).
Table I Patient demographic and clinical data
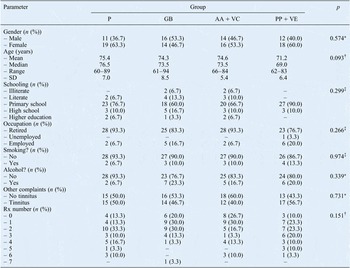
*Chi-square test; †analysis of variance with fixed factors; ‡Fisher's exact test or its extension. P = placebo; GB = ginkgo biloba; AA + VC = α-lipoic acid plus vitamin C; PP + VE = papaverine chlorhydrate plus vitamin E; SD = standard deviation; Rx number = number of medications
Information on other health and well-being issues was also recorded, as shown in Table II. All four treatment groups exhibited statistically similar profiles regarding the use of hearing aids (p = 0.749), systemic arterial hypertension (p = 0.618), dyslipidaemia (p = 0.923), heart disease (p = 0.615), hypothyroidism (p = 0.107), osteoporosis (p = 0.766), joint disease (p = 0.614), benign prostatic hyperplasia (p = 0.600), other comorbidities (p = 0.586), duration of hearing loss (p = 0.358), hearing risk (p = 0.339), and otoscopy alterations without effects on hearing (p > 0.999).
Table II Patient comorbidity and hearing data

*Fisher's exact test or its extension; †chi-square test; ‡analysis of variance with fixed factors. P = placebo; GB = ginkgo biloba; AA + VC = α-lipoic acid plus vitamin C; PP + VE = papaverine chlorhydrate plus vitamin E; pts = patients; HT = hypertension; BPH = benign prostatic hyperplasia; comorb = cormobidity; durn = duration; SD = standard deviation; bilat = bilateral; R = right
Participants also underwent audiometric testing (at 250, 500, 1000, 2000, 3000, 4000, 6000 and 8000 Hz) and assessment of speech recognition threshold and percentage index of speech recognition, before and six months after treatment.
Twenty-nine participants did not complete treatment. The percentage of these individuals in each treatment group was similar, and differences between groups were statistically insignificant (p = 0.247). Among these 29 participants, the reasons for failing to complete treatment were: withdrawal (n = 18), abdominal discomfort (n = 5), death (n = 1) and worsening comorbidity (n = 5); the distribution of these reasons was statistically similar among all four groups (p = 0.433).
Statistical analysis of audiometric results was performed on an intention-to-treat basis. Thus, baseline measures were also attributed as end-of-treatment measures in individuals who did not complete treatment.
For data analysis, we used the arithmetic means of results for the right and left sides, as we were not interested in comparing sides.
A summary of participants' audiological results is shown in Table III.
Table III Audiological data

Data represent hearing thresholds (dB) unless otherwise specified. *Mean of results at 500, 100, 2000 and 4000 Hz. P = placebo; GB = ginkgo biloba; AA + VC = α-lipoic acid plus vitamin C; PC + VE = papaverine chlorhydrate plus vitamin E; Med = median; Min = minimum; Max = maximum; SD = standard deviation; Pre = before treatment; Post = after 6 months of treatment; SRT = speech recognition threshold; PISR = percentage index of speech recognition
Inferential results showed no interaction effect between the treatment groups and between the two time points (i.e. before and after treatment), for any investigated measure. That is, results before and after treatment were not significantly different within any treatment group, and results between groups were not significantly different either before or after treatment.
Following treatment, the four treatment groups exhibited no statistically significant audiological differences at 250 Hz (p = 0.184), 2000 Hz (p = 0.190), 3000 Hz (p = 0.086), 4000 Hz (p = 0.180) or 6000 Hz (p = 0.059). However, significant differences were observed at 500 Hz (p = 0.001), 1000 Hz (p = 0.001) and 8000 Hz (p = 0.043), as well as for the speech recognition threshold (p = 0.008) and percentage index of speech recognition (p = 0.003) tests (Table IV).
Table IV Treatment group comparisons

SRT = speech recognition threshold; PISR = percentage index of speech recognition; P = placebo; GB = ginkgo biloba; AA + VC = α-lipoic acid plus vitamin C; PP + VE = papaverine chlorhydrate plus vitamin E
When comparing results before versus after treatment, we noticed an increased hearing threshold (i.e. the hearing threshold was smaller before treatment than afterwards) at 2000 Hz (p = 0.004) and 6000 Hz (p = 0.006). In the remaining data, there were no statistically significant changes over time.
It is worth noting that these conclusions were presented due to a lack of interaction between groups and time points.
Discussion
In recent years, there has been a large increase in the number of publications on the use of antioxidant agents in diverse areas of medicine. In the field of hearing, there have been reports on the use of antioxidants for several conditions: sudden hearing loss, ototoxicity, tinnitus, acute acoustic trauma and presbyacusis.Reference Takumida and Anniko15, Reference Haase, Prasad, Cole, Baggett-Strehlau and Wyatt16
Regarding presbyacusis, it is known that auditory alterations do not occur uniformly among people over time. This variability suggests that presbyacusis has multiple aetiologies and results from a complex integration of environmental and genetic factors, both at the cochlear and central levels. Such factors include environmental agents, for example noise and ototoxic substances, which cause mitochondrial damage and oxidation activity.Reference Liu and Yan17
Of the several structures related to auditory ageing, the stria vascularis of the cochlear duct seems to be one of the most important. Studies on cochlear physiology have indicated that the stria vascularis is the structure responsible for endocochlear potential generation and cochlear haemostasis.Reference Salt, Melichar and Thalmann18 Moreover, microvascular alterations observed in animals during the ageing process might also be related to degeneration in associated areas of the stria vascularis.Reference Gratton and Schulte19
Recent research has suggested a significant role for free radicals in the genesis of presbyacusis. Based on this, we decided to investigate whether the use of selected antioxidant agents, which act as antagonists to free radicals, would improve hearing thresholds in patients diagnosed with presbyacusis. This expected improvement in patients' hearing thresholds would result from controlling the damage caused by free radicals in the inner ear, more specifically in the stria vascularis, as well as from an increase in stria vascularis functioning.
The antioxidant agents used in this study were selected from available agents with the most consistent scientific evidence regarding hearing threshold improvement. A literature review showed that few studies exist on the effects of drugs used to treat presbyacusis; even fewer of these studies had a control group and a rigorous methodological design. Some studies indicated that a combination of different antioxidants was more effective than separate usage. Different antioxidant agents often have different modes of action. Some stabilise cell membranes (especially mitochondrial membranes), some remove oxygen free radicals and others act synergistically with other antioxidants.Reference Seidman7, Reference Heman-Ackah, Juhn, Huang and Wiedmann20 We used antioxidant agents either alone or in combination, to establish their efficacy as agents of hearing improvement.
The selected antioxidants were prepared following strict pharmacological standards. However, it is known that some substances, mainly phytotherapeutic agents such as ginkgo biloba, are difficult to standardise as regards bioavailability and bioequivalence criteria. Moreover, although safe doses of these substances have been well defined, the establishment of precise therapeutic doses (as required in the present study) still requires more research. Our study did not use standardised, commercial pharmaceutical products because the combinations required were not commercially available; moreover, the use of commercial preparations would have made blinding impossible for both patients and researchers.
Some participants did not complete all stages of the study. It is worth noting that the number of participants who did not complete the study was statistically similar in all four groups. Moreover, the reasons for loss to follow up were evenly distributed. We therefore conclude that, in this patient group and for this length of treatment, tolerance of the tested substances was adequate, with none causing clinically significant adverse effects.
During the selection stage, the presence of other possible causes of hearing loss (besides presbyacusis) was an exclusion criterion. We also excluded patients with diabetes mellitus and anticoagulant drug use. We included the latter criterion because the use of ginkgo biloba in patients already taking anticoagulants may aggravate haemorrhagic phenomena.Reference Bressler21 Similarly, α-lipoic acid may reduce blood glucose levels and thus affect glycaemic equilibrium, especially in users of hypoglycaemic agents.Reference Bilska and Wlodek10, Reference Singh and Jialal22 Other known participant comorbidities were researched in the literature to determine whether they could affect hearing thresholds. For example, it has been suggested that cardiovascular conditions are associated with audiometric alterations, mostly in the low frequencies.Reference Gates, Cobb, D'Agostino and Wolf23, Reference Friedland, Cederberg and Tarima24 In our patients, the distribution of investigated comorbidities was homogeneous among treatment groups, preventing any conclusions about associations between specific clinical conditions and hearing thresholds. This homogeneity also minimised the possible influence of comorbidities on the final study results.
• Free radicals are known to contribute to presbyacusis aetiology
• Several antioxidants (i.e. free radical antagonists) are known to be clinically beneficial
• This study evaluated the hearing effects of antioxidants in presbyacusis patients
• No statistically significant change was observed
A 2009 study by Takumida and Anniko investigated the use of α-lipoic acid, vitamin C and rebamipide in individuals with presbyacusis, and found hearing threshold improvements after treatment.Reference Takumida and Anniko15 However, this study differed from our own as regards length of follow up (which was approximately three months on average) and methodology. Our study used a longer follow-up period (six months). Even so, the length of treatment used in our study may have been too short, as presbyacusis is an insidious and slowly progressing condition.
Importantly, during our six-month follow-up period there were no apparent significant modifications in the placebo group. This finding may corroborate the idea that the slow progression of presbyacusis demands longer periods of experimental treatment, in order to enable a more accurate analysis of the potential effects of antioxidants on the natural progression of this disease.
The results of the current study did not show any statistically significant effects of antioxidant agents on the hearing threshold of the sample population, over the six-month study period.






