Introduction
Endoscopic skull base surgery represents a rapidly growing field with ever-evolving methodologies. The indications for expanded endoscopic transnasal approaches continue to increase, with major and more complex skull base defects needing to be repaired. These expanded endoscopic approaches are a good option for selected patients with anterior skull base tumours because they allow for a complete tumour resection and decrease comorbidities and post-operative complications related to open surgery. These expanded approaches have necessarily led to the need for increasingly complex cranial base reconstruction to prevent cerebrospinal fluid (CSF) leakage, neurovascular damage and meningitis.Reference Tabaee, Schwartz, Anand, Anand and Schwartz1
The endoscopic approach presents several advantages when compared to open surgery. It obviates the need for brain retraction, provides a direct corridor to the pathology that does not cross any cranial nerves or vascular structures, decreases hospital admission time, and potentially improves quality of life for patients compared with the transcranial or endonasal microscopic approaches.Reference Cavallo, de Divitiis, Aydin, Messina, Esposito and Iaconetta2,Reference Dehdashti, Ganna, Witterick and Gentili3 The lack of craniofacial incisions, the minor rate of post-operative hydrocephaly and the possibility of performing an orbital decompression in the same approach are other advantages related to the endoscopic approach.
The success of this procedure depends on the correct selection of patients, advances in endoscopic imaging technologies, new surgical instrumentation and development of multi-specialty, four-handed techniques. Multiple techniques including the use of synthetic materials, dermal and mucosal grafts, cartilage, bone, fat and fascia grafts, local, regional and free flaps, and fibrin glue have classically been used in a number of layered combinations and have been successful in considerably reducing the rate of post-operative CSF leak.Reference Cappabianca, Cavallo, Mariniello, de Divitiis, Romero and de Divitiis4–Reference Nyquist, Anand, Singh and Schwartz10 Nevertheless, success rates depend on the surgical technique, surgeon's experience, defect size and tumour type, and most case series often include pituitary adenomas, which are generally extra-arachnoidal tumours with a lower rate of post-operative CSF leak rate.
In our experience, the use of the gasket seal technique was a leap forward that permitted expanded endoscopic skull base surgical procedures with fewer complications, especially CSF leakage. Furthermore, the development of several pedicled endonasal mucoperiosteal flapsReference Hadad, Bassagasteguy, Carrau, Mataza, Kassam and Snyderman6,Reference Fortes, Carrau, Snyderman, Prevedello, Vescan and Mintz11,Reference Rivera-Serrano, Bassagaisteguy, Hadad, Carrau, Kelly and Prevedello12 and their combination with the gasket seal technique enabled us to close larger skull base defects without increasing the rate of post-operative complications.
The aim of this study was to report our experience in the management and reconstruction of anterior skull base defects after using the endoscopic transsphenoidal approach for pituitary tumours where the sellar diaphragm was opened and significant intra-operative CSF leakage occurred. We describe the results obtained with our favourite technique, the gasket seal method combined with a mucosal pedicled endonasal flap, which reduces the rate of complications, especially the rate of post-operative CSF leakage.
Materials and methods
We reviewed a prospectively acquired database of all endonasal endoscopic surgical procedures performed at Son Espases University Hospital between January 2013 and December 2018.
All patients were diagnosed with pituitary tumours using magnetic resonance imaging and computed tomography and had symptoms that had not improved with medical treatment. We only included cases where the sellar diaphragm was opened during surgery and where there was a significant intra-operative CSF leak.
In all cases, according to the skull base unit protocol, the reconstruction of the skull base defect was performed by combining the gasket seal technique using an autologous fascia lata graft (Figure 1) with a pedicled mucosal endonasal flap. Initially, the favourite option was to use a nasoseptal mucosal flap with reconstruction of the donor site using a contralateral reverse rotation flap to decrease the post-operative morbidity and crust formation.Reference Hadad, Bassagasteguy, Carrau, Mataza, Kassam and Snyderman6,Reference Kasemsiri, Carrau, Otto, Tang, Prevedello and Muto13 An alternative would be to use a posterior pedicled lateral nasal wall flap vascularised by the sphenopalatine artery, which includes the nasal inferolateral wall with the mucoperiosteal portion of the inferior turbinate. For the last seven patients, we created a middle turbinate mucosal flap based on its inferior insertion.

Fig. 1. Gasket seal technique. Intra-operative photographs showing: a) anterior skull base defect is created; b) inlay fascia lata graft; c) onlay fascia lata graft; and d) vomer graft is observed in the centre of the reconstruction.
The characteristics of each patient, histopathology of the tumours, length of hospital stay, rate of post-operative CSF leaks, and repair-related complications, such as intracranial infections, nasal bleeding, revision surgery and hydrocephalus, were analysed. Finally, patients were classified into three groups according to the endonasal mucosal flap used to reinforce the gasket seal closure. The surgical time was compared between the three groups. The student's t-test was used, and the statistical significance was defined as p < 0.05.
Surgical technique
After the skull base defect had been created, the first step was to eliminate any dead space using autologous fat graft, degenerate cellulose or bovine cellulose. This prevented CSF from pooling over the closure. As suggested by other authors, if we have opened sufficiently widely into the third ventricle, we can often skip this step to prevent the possibility that the graft will dislodge into the ventricular system and obstruct the aqueduct of Sylvius.
As a second step, an autologous fascia lata graft was harvested and placed into a vancomycin solution until used to repair the defect. A piece of fascia lata graft, larger than the defect, was placed as an inlay graft at the subdural level to seal the defect. Another piece of fascia lata was placed as an onlay graft at the extradural level, centred over the defect. The fascia lata graft was fashioned in the same shape as the cranial base defect but with an additional 2 cm of diameter in order to extend 1 cm beyond the edge of the cranial base defect circumferentially.
Third, a piece of rigid material, such as vomer, was fashioned to be roughly the size of the bone defect, and this rigid graft was centred over the fascia lata graft so that there was at least 1 cm of fascia lata graft extending circumferentially around the rigid graft.
Fourth, the rigid graft was gently countersunk into the bone defect, which draws the fascia lata graft into the defect. The central portion of the fascia lata graft was intracranial, whereas the edges remained in the sinus cavity, similar to a cauliflower leaf. The fascia lata, which was circumferentially wedged between the bony edge of the cranial defect and the graft, created a watertight gasket seal (Figure 2).

Fig. 2. Schematic view of the three layer gasket seal technique.
Fifth, we covered the gasket seal with the endonasal mucosal flap harvested at the beginning of the surgery, and fibrin glue is dripped around the edges and over the top of the reconstruction. We do not routinely check the hermeticity of the reconstruction with fluorescein. Two Merocel® nasal packs were used for each nasal fossa, and both were protected with latex finger clots and antibiotic ointment to avoid avulsion of the flap during the nasal packing removal. The nasal packing was maintained for 5 days. During this period, we prescribed: total bed rest, in a supine position with the upper body and the head elevated to 30°; anticoagulant prophylaxis with low molecular weight heparin and compression stockings at lower extremities; a fibre-rich diet; laxatives; and antibiotic prophylaxis of 1 g amoxycillin-clavulanate every 8 hours. We did not routinely place a lumbar drain. Patients were seen by the ENT specialist for nasal hygiene on day 15 and at 6, 10 and 18 weeks, post-operatively.
Results
A total of 28 patients were included in the study: 17 of them were female (60.7 per cent), and 11 were male (39.3 per cent). The age at surgery ranged between 36 and 72 years, with a mean age of 53 years. All lesions had a significant intracranial extension, and surgery resulted in a large cranial base defect with a significant CSF leak. Reconstruction was performed in all cases with a combination of the gasket seal technique and pedicled mucosal endonasal flap. The nasoseptal flap, the mucoperiosteal lateral wall flap and the middle turbinate mucosal flap were used for nasal reconstruction in 13, 8 and 7 patients, respectively (Figure 3). Even though all the patients had Tissucol® (fibrin glue) placed over the mucoperiosteal endonasal flap, Tissucol was not put between it and the gasket seal as this would prevent the flap from adhering to the skull base. The anatomopathological analysis showed 18 cases of pituitary adenoma, 4 Rathke cysts, 3 fibrous meningiomas, 2 craniopharyngioma and 1 anaplastic pleomorphic xanthoastrocytoma (Figure 4). The length of hospital stay ranged between 6 and 20 days with a mean of 7.7 days.

Fig. 3. The three types of endonasal flaps used in this study. GS = gasket seal; MT = middle turbinate flap; NS = nasoseptal flap; LW = lateral wall flap
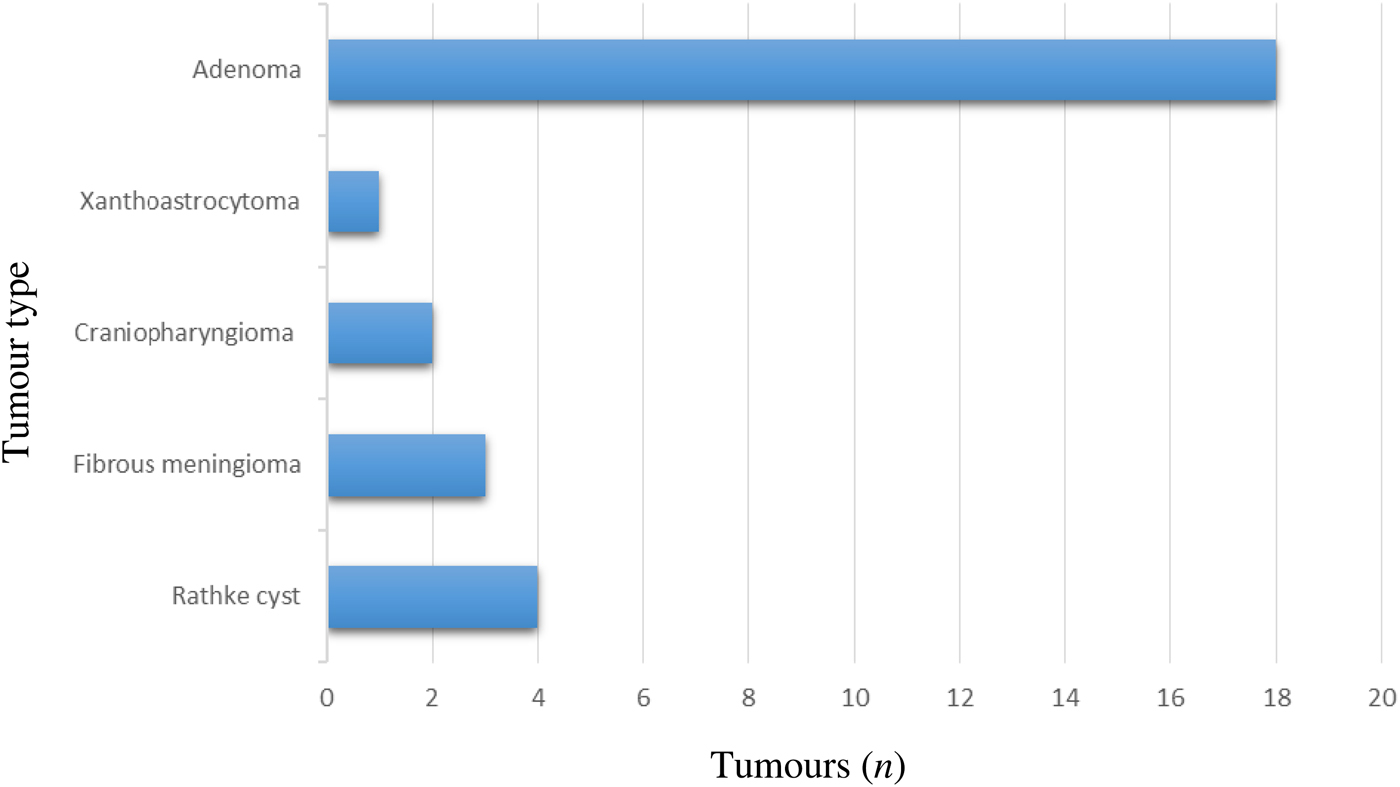
Fig. 4. Graph showing the histological tumour types in this study.
After a mean follow-up period of 24 months, there was only one case (3.57 per cent) of post-operative CSF leakage from the site of the gasket seal closure after nasal packing removal, confirmed by the beta trace protein test. The patient was diagnosed with pituitary craniopharyngioma and needed a second surgery where a contralateral Hadad flap was used to reinforce the reconstruction. No cases of intracranial infection, hydrocephalus or nasal bleeding were observed.
The average surgical time for gasket seal closure was 28 minutes and was 17 minutes for fascia lata harvesting. With respect to the three different endonasal flaps, the average surgical time was 27, 42 and 12 minutes for nasoseptal (group A), inferolateral wall (group B) and middle turbinate (group C) flaps, respectively.
There was a statistically significant difference between group C and groups A and B (student's t-test, p < 0.05). In groups A and B, a periodic nasal hygiene procedure to remove crusts was needed for a period of at least 10 weeks. On the other hand, faster healing of nasal mucosa was observed in group C, with disappearance of crusts by week six of follow-up. Finally, no patient had a lumbar drain left in place either pre-operatively or because of an inadequate closure.
Discussion
Previously, reconstruction of extended skull base defects after endonasal skull base surgery has been a challenge for ENT surgeons. The relatively high risk of post-operative CSF leak (50 per cent in some series studies) has been the primary limitation of endonasal cranial base surgical approaches.Reference Dehdashti, Ganna, Witterick and Gentili3,Reference Kitano and Taneda7 In recent years, specific attention has been paid to this problem, and advances in reconstructive techniques have led to dramatic improvements in the rates of post-operative CSF leak to such an extent that the goal of having only 5 per cent of patients with CSF leaks is now achievable in most experienced groups.
The risk of post-operative CSF leak appears to be related to factors such as the presence of intra-operative CSF leak, history of previous transsphenoidal surgery, lesion size, lesion type and extent of the transsphenoidal approach. Post-operative CSF leak after transsphenoidal surgery can have secondary consequences such as tension pneumocephalus and meningitis. In addition, CSF leaks result in significant financial costs for individuals and society through greater length of stay in the hospital and working time lost.Reference Grotenhuis14
With respect to the extended transsphenoidal approach, a correlation has been observed between the degree of intra-operative leak and the risk of post-operative leak. Esposito et al.Reference Esposito, Dusick, Fatemi and Kelly15 reported that large diaphragmatic or dural defects, which are associated with extended transsphenoidal approaches, had a post-operative leak rate of 12 per cent compared with 1.6 per cent for smaller intra-operative leaks. These larger leaks had a 3.4 per cent rate of bacterial meningitis compared with only 0.16 per cent for smaller leaks.
In the study published by Shiley et al.,Reference Shiley, Limonadi, Delashaw, Barnwell, Andersen and Hwang16 the presence of intra-operative leaks correlated with a 12.7 per cent rate of post-operative leak compared with 2.7 per cent when no intra-operative leak was present. In another study, post-operative CSF leak occurred in 4 per cent of cases with an intra-operative leak compared with only 0.7 per cent of cases where no leak was observed.Reference Esposito, Dusick, Fatemi and Kelly15 Hence, for large, extended transsphenoidal approaches such as those described in this article, the risk of CSF leak and meningitis would appear to be quite high.
Regarding lesion type, Esposito et al.Reference Esposito, Dusick, Fatemi and Kelly15 reported that the rate of repair failure is highest for meningiomas (21 per cent) compared with craniopharyngiomas (3 per cent) and pituitary adenomas (2 per cent). Long operative time is also associated with post-operative CSF leak, as shown by Tabaee et al.Reference Tabaee, Anand, Brown, Lin and Schwartz17
It seems obvious that, for tumours with a large intradural component, which often includes an intraventricular opening, the risk of post-operative CSF leak is high, and a single layer closure technique cannot be sufficient. In these cases, a more complex, multilayer method has to be used.
Several authors have described different mechanisms to close large defects in the anterior cranial base. In a study with 105 patients, Couldwell et al.,Reference Couldwell, Weiss, Rabb, Liu, Apfelbaum and Fukushima18 reported a CSF leak rate of 6 per cent after extended transsphenoidal approaches. Closures involved the packing of fat graft into the intracranial cavity, followed by placement of fascia lata or absorbable plate, and finally fat packing of the sphenoid sinus. Kitano and TanedaReference Kitano and Taneda7 presented their experience with extended transsphenoidal surgical procedures. Closure consisted of either a sutured fascia lata graft, which had a 30 per cent post-operative CSF leak rate, or a double-layer sutured graft of polytetrafluoroethylene and fascia lata, which had a 9 per cent post-operative CSF leak rate. Kassam et al.Reference Kassam, Carrau, Snyderman, Gardner and Mintz19 and Snyderman et al.Reference Snyderman, Kassam, Carrau and Mintz20 have also described a multilayer closure technique. The latter study used DuraGen® as an inlay and acellular dermis as an onlay, followed by fat, fibrin glue and a balloon stent. In a study by Hadad et al., a vascularised nasoseptal flap was used, which reduced the risk of CSF leaks to 5 per cent.Reference Hadad, Bassagasteguy, Carrau, Mataza, Kassam and Snyderman6 de Divitiis et al.Reference de Divitiis, Cavallo, Cappabianca and Esposito21 reported their experience with the extended endonasal endoscopic transsphenoidal approach. The closure technique, briefly described in their series study, includes the use of multiple onlay layers of dural substitute or mucoperichondrium patches and, in some cases, a Fogarty balloon to hold their construct in place. In their series of 20 patients, they reported a CSF leak rate of 5 per cent. ZanationReference Zanation, Carrau, Snyderman, Germanwala, Gardner and Prevedello22 et al. have reported similar results with a success rate of 94.3 per cent in their series of 70 patients with intra-operative high-flow CSF leak. They used a nasoseptal flap combined with a dural substitute preferentially placed as an inlay graft to cover the exposed intracranial structures reconstructing the arachnoid.
A recent systematic review by Soudry et al. showed better outcomes with vascularised repairs especially in the setting of high-flow CSF leak; leak rates of 82 and 94 per cent were found with free graft/synthetic materials and vascularised repairs, respectively.Reference Soudry, Turner, Nayak and Hwang23 Mucocele formation, prolonged skull base crusting and donor-site complication, specifically septal perforation secondary to nasoseptal flap harvest, are the principal complications observed with reconstruction with a nasoseptal flap. However, using a nasoseptal flap is typically the first reconstructive option because of its versatility and excellent success rate (96 per cent) that can be achieved after surgeons have overcome the learning curve.Reference Patel, Stadler, Synderman, Carrau, Kassam and Germanwala24
In our experience, when we began to use the gasket seal technique to repair intra-operative high-flow CSF leak defects, we observed a significant improvement in post-operative CSF leakage and meningitis rates. We always prefer autologous materials, with both inlay and onlay fascia lata graft and a vomer graft, which is used for the mechanical seal of the defect. Furthermore, donor-site morbidity related to the fascia lata harvesting is very low.
The philosophy behind the gasket seal technique is to provide an autologous graft that is placed in direct contact with the patient's dura and held firmly in place to facilitate vascularisation or fibrosis to ensure a long-term seal. The graft must be held rigidly in place, which is why we used a buttress. A buttress also avoids the need for an inflated intranasal balloon with its inherent risks of overinflation, local infection, sinusitis and post-operative distress to the patient. With respect to the original description of the gasket seal technique, our modification is that we prefer to use two fascia lata grafts, the first in direct contact with the dura (inlay) and the second at extradural level (onlay), and together with the vomer graft these form a three-layer gasket seal closure. However, if the buttress falls away from the skull base, the gasket seal fails.
For this reason, when a large anterior skull base defect has been created, with a significant intra-operative high-flow CSF leak, we combine the gasket seal technique with an endonasal mucosal flap to reinforce the closure. We consider that the rigid buttress shields the mucosal flap from CSF pulsations, which may allow the flap to heal more readily. The results published by Haddad et al. motivated us to combine both methods to increase efficacy and to provide a long-term vascular supply and to facilitate mucosal ingrowth.Reference Hadad, Bassagasteguy, Carrau, Mataza, Kassam and Snyderman6
More recently, Garcia-Navarro et al,Reference Garcia-Navarro, Anand, Theodore and Schwartz25 published a rate of post-operative CSF leak in a series of 46 patients. They observed a post-operative CSF leak rate of 5.2 per cent, with the gasket seal technique alone, and a rate of 4.7 per cent when combined with a nasoseptal flap. Even though the authors saw no statistically significant differences, they concluded that the vascularised flap leads to more rapid epithelialisation of the sphenoid sinus, which increases the long-term security of the closure and increases functionality of the sphenoid mucosa. Likewise, in other studies, the vascularised flap reduces the incidence of CSF leak, adding additional security to the closure.Reference Kassam, Carrau, Snyderman, Gardner and Mintz19,Reference Di Maio, Cavallo, Esposito, Stagno, Corriero and Cappabianca26 MascarenhasReference Mascarenhas, Moshel, Bayad, Szentirmai, Salek and Leng27 et al. identified 122 patients who underwent 126 surgical procedures using the transplanum transtuberculum approach, and the CSF leak rates varied with the technique from 11 per cent (fat graft only) to 4.2 per cent (gasket seal only) to 1.8 per cent (fat plus nasoseptal flap) to 0 per cent (gasket plus nasoseptal flap). Hu et al.Reference Hu, Gu, Zhang, Xie, Yu and Sun28 observed no CSF leak and no intracranial infections with the combination of a gasket seal closure and a nasoseptal flap multilayer reconstruction technique for anterior skull base defects with an intra-operative high-flow CSF leak.
These results are similar to the results we obtained when combining the two techniques.
We consider that the vascularised endonasal flaps represent a new advancement in the reconstruction of large anterior skull base defects because they promote a rapid and complete cicatrisation and decrease the rate of post-operative complications. We always reconstructed the pedicled nasoseptal flap donor site with a contralateral reverse rotation flap as described by Kasemsiri et al.Reference Kasemsiri, Carrau, Otto, Tang, Prevedello and Muto13 in order to avoid the morbidity related to the nasoseptal flap and crust formation. Despite this, we observed better results in terms of surgical time and mucosa healing in group C where a middle turbinate mucosal flap was used. This may be because the nasoseptal flap and inferolateral wall flap are formed from the entire mucosa of the nasal septum and the mucosa of inferolateral nasal wall, including the inferior turbinate and the nasal floor, respectively. In both cases, crusting of the mucosa harvest site was common and can require debridement until a complete mucosa resurfacing is obtained. On the other hand, the use of the middle turbinate mucosal flap leaves the septum and lateral wall intact, so the mucosa healing time is much faster, comparable with that of a routine endoscopic sinonasal surgery. For this reason, using a middle turbinate mucosa flap is our favoured option for reinforcing the gasket seal closure when an intra-operative high-flow CSF leak is observed. Furthermore, it has become the workhorse for endoscopic reconstruction of small anterior skull base defects with no intra-operative CSF leak.
• Post-operative cerebrospinal fluid leaks are the most common complication of large anterior skull base defects
• A multilayer closure technique is the best option for reconstruction
• A gasket seal closure is the ‘gold standard’ technique
• Nasoseptal, inferior lateral and middle turbinate flaps can be used in combination with the gasket seal technique
• Use of the middle turbinate flap is associated with less surgical time and faster mucosa healing
• Using this combined method of reconstruction, a post-operative cerebrospinal fluid leak rate of less than 4 per cent can be achieved
As suggested by Leng et al.,Reference Leng, Brown, Anand and Schwartz8 we prefer to avoid a Foley balloon in the nasopharynx for several reasons: it is uncomfortable for patients, interferes with normal sinus drainage and can lead to gagging, with possible mucus aspiration. Additionally, we believe that if a gasket seal closure is performed correctly, the Foley balloon brings no benefits; indeed, the inflation of the balloon can dislodge the closure and possibly increase intradural pressure and neurovascular compression.
Conclusion
The gasket seal technique is a very effective and simple method to repair large anterior skull base defects with an intra-operative CSF leak. The use of an endonasal mucosal flap to reinforce the gasket seal closure adds security and may potentially improve the surgical results in terms of post-operative complications. The middle turbinate mucosal flap is a very good option due to the lack of significant morbidity.
Competing interests
None declared






