Introduction
Thyroid eye disease is an autoimmune condition which causes an inflammatory infiltrate in the tissues of the orbit, with a particular predilection for the extra-ocular muscles.Reference Weetman1–Reference Perros and Kendall-Taylor4
Patients whose disease becomes inactive may be left with residual proptosis, lid retraction and strabismus. Although these features can cause functional impairment; they also result in marked cosmetic disfigurement. This appearance can be psychologically disabling, especially for young women, in whom this condition is common.Reference Weetman1 More than 50 per cent of patients with thyroid eye disease are aware that their eyes look abnormal.Reference Shorr, Nehaus and Bayliss5
Surgical decompression is a well recognised form of treatment for functional impairment caused by thyroid eye disease, particularly compressive optic neuropathy or extreme exposure keratopathy. However, its value for cosmesis has not been well documented. Only two previous studies have examined orbital decompression for cosmetic reasons.Reference Shepard, Levin and Terris6, Reference Asaria, Koay, Elston and Bates7 In both of these, patient numbers were small and patients' post-operative satisfaction with cosmesis was poorly documented.
The aim of this study was to evaluate a group of patients with thyroid eye disease who had undergone endoscopic orbital decompression primarily for dyscosmesis.
Materials and methods
A retrospective case review was performed of all patients who had undergone endoscopic orbital decompression for cosmesis in our departments during the period January 1996 to September 2002. A postal questionnaire was also sent to all the patients who had undergone the procedure, in order to assess their satisfaction. All patients with dysthyroid eye disease undergoing endoscopic orbital decompression were chosen for study. All patients were biochemically stable with regard to their hyperthyroidism at the time of surgery.
Pre- and post-operative assessment
Axial and coronal computed tomography scans were performed in all cases, as surgical planning ‘roadmap’ investigations. Pre- and post-operative ophthalmic assessment included visual acuity and fields, Hertel exophthalmometry measurements, documentation of extra-ocular movements, and slit-lamp examination. Patient photographs were taken before and after the operation to compare cosmetic appearances (Figure 1).
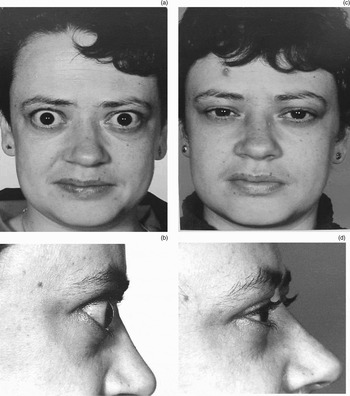
Fig. 1 Pre-operative (a and b) and post-operative (c and d) appearance of a patient who underwent endoscopic orbital decompression. This patient achieved reductions in proptosis of 4 mm (right eye) and 3 mm (left eye) following decompression. Subjective eye prominence scores reduced from 7 and 8 pre-operatively (right and left eyes, respectively) to 1 post-operatively (both eyes). (Published with patient's permission.)
Symptom scores were obtained by asking each patient to rate their eye prominence, on a linear analogue score of one (not prominent) to 10 (very prominent), both before and after surgery. Patients who had undergone bilateral decompressions were asked to consider each eye separately.
Surgical technique
Detailed accounts of endoscopic orbital decompression technique can be obtained elsewhere.Reference Metson, Dallow and Shore8–Reference Kennedy, Goodstein, Miller and Zinreich10 All operations were performed under general anaesthetic. Initially, an endoscopic spheno-ethmoidectomy was performed to expose the medial orbital wall and to define the bony landmarks for the optic nerve and internal carotid artery. The lamina papyracea was gently removed from the underlying periorbita. Access to the orbital floor was gained endonasally via a large middle meatal antrostomy, and the floor medial to the infra-orbital nerve was removed. On the rare occasion that further decompression seemed necessary, the lateral orbital floor was removed via a Caldwell–Luc approach, taking care to preserve the section of mid-floor overlying the infra-orbital nerve. Following sufficient orbital bone removal, the periorbita was opened widely, facilitating orbital fat prolapse into the space created.
Data analysis
Data were analysed using Microsoft Excel 2003 software (Microsoft, Redmond, Washington State, USA). The reduction of proptosis was computed as the difference between the pre- and post-operative exophthalmometry readings on the operated eye (i.e. post-operative reading minus pre-operative reading). The difference in subjective eye prominence scores was similarly computed (i.e. post-operative eye score minus pre-operative eye score). Summary statistics are presented as means±standard deviation (SD). Paired t-tests were used to compare differences between pre- and post-operative proptosis. A significance level of p < 0.05 was employed.
Results
Twenty orbits of 15 patients underwent endoscopic decompression. Patients comprised 13 women and two men; the mean age was 51 years (range 20–81 years). The primary indication for surgery in each case was cosmetic.
Proptosis reduction
All 15 patients were assessed pre- and post-operatively. Their duration of post-operative follow up ranged from two to 30 months (mean 13 months). The pre- and post-operative exophthalmometry measurements were 22.7±4.5 mm and 19.0±4.0 mm (mean±SD), respectively. Figure 2a shows the pre- and post-operative results for exophthalmometry. For all orbits, the mean±SD reduction in proptosis was 3.7±2.2 mm (t = 6.5, p < 0.001). One patient developed reactivation of her eye disease shortly after the operation. By the time of her follow-up appointment, eight months later, her exophthalmos had returned, and she therefore did not achieve a measured reduction in proptosis (orbit two, Figure 2a)

Fig. 2 Pre- and post-operative (a) exophthalmometry measurements and (b) visual analogue scores. Patients' orbits are numbered sequentially. (One patient who underwent bilateral decompression did not respond to the questionnaire; these results are therefore not shown.)
.
Complications of surgery
One patient developed acute sinusitis on the eighth post-operative day and was readmitted for treatment with intravenous antibiotics. In 13 of the 20 operations, patients were discharged within 24 hours of surgery. One patient developed post-operative rhinorrhoea, although the presence of cerebrospinal fluid was never confirmed as the discharge settled spontaneously within 48 hours. No patient experienced visual loss or infra-orbital hypoaesthesia.
Two patients complained of epiphora following surgery. In both cases, this only settled following secondary dacryocystorhinostomy (DCR) surgery.
Diplopia
One patient had pre-operative diplopia that resolved completely after decompression surgery. Seven patients had both pre- and post-operative diplopia. In each of these cases, patients reported no change in diplopia. Four patients developed new post-operative diplopia. Three of these had undergone bilateral decompressions. Two patients had diplopia that resolved following muscle surgery in one and botulinum toxin injection in the other. The remaining patient with new diplopia following unilateral decompression experienced resolution of this symptom 20 months after the operation, without intervention.
Patient satisfaction
Questionnaires were returned by 14 of the 15 patients (93 per cent response). Four of these patients had bilateral decompressions, raising the total number of decompression procedures to 18. For 16 of the endoscopic decompressions (89 per cent), patients reported that they were ‘satisfied’ with the appearance of their eye. Two patients responded that they were ‘not satisfied’ with the post-operative appearance. These patients had a reduction in proptosis of 1.0 and 4.0 mm in the relevant eye, respectively, (orbits six and eight, Figure 2b). In each case, patients reported an improvement in eye prominence score post-operatively. However, the proptosis reduction as calculated by exophthalmometry did not correlate significantly with the proptosis reduction as subjectively scored by patients (Pearson's r = 0.17; 95 per cent confidence intervals = −0.32 to 0.59; p = 0.50). All patients who returned the questionnaire stated that, in retrospect, they would still have chosen to have the operation.
Two patients had received orbital radiotherapy prior to decompression surgery. These patients achieved an average proptosis reduction of 5.0 mm.
Following decompression, five patients went on to have lid surgery for the same cosmetic indications.
Discussion
Thyroid eye disease predominantly affects young and middle-aged women. This group of patients are particularly conscious of the appearance of their eyes. Unlike traditional external decompression surgery, endoscopic decompression has the advantage of not leaving a facial scar and is therefore more cosmetically acceptable. All patients achieved a reduction of proptosis after the operation except one, who developed a reactivation of thyroid eye disease in the post-operative period. Most patients (89 per cent) were satisfied with the cosmetic appearance of their eye following endoscopic decompression surgery.
The surgical efficacy of endoscopic orbital decompression is recognised to be similar to that of external decompression, with a substantial degree of proptosis reduction being possible.Reference Shepard, Levin and Terris6, Reference Metson, Dallow and Shore8, Reference Kennedy, Goodstein, Miller and Zinreich10, Reference Lund, Larkin, Fells and Adams11 One study which directly compared the outcome of 21 external decompressions with that of 13 endoscopic decompressions found proptosis to be reduced by averages of 4.4 and 3.8 mm, respectively.Reference Lund, Larkin, Fells and Adams11 The mean reduction of proptosis in our study is similar to that reported by others using the endoscopic technique.Reference Lund, Larkin, Fells and Adams11–Reference Eloy, Trussart, Jouzdani, Collet, Rombaux and Bertrand13 Most studies have reported an average reduction ranging from 3–5 mm, although greater amounts of globe retraction are achievable.Reference Shepard, Levin and Terris6, Reference Metson, Dallow and Shore8, Reference Kennedy, Goodstein, Miller and Zinreich10 However, comparison of results (in terms of proptosis reduction) across studies may not be valid due to varying amounts of pre-operative exophthalmometry and heterogenous indications for surgery. In the present study, patients who needed decompression for visual reasons were specifically excluded. As the primary goal of surgery in our cases was to improve cosmesis, it would seem appropriate to grade success in terms of patient satisfaction rather than objective change in proptosis, post-operatively. Although there was a measured reduction of proptosis in 17 of the cases and a reduction in subjective eye prominence in all cases (Figure 2), in some instances the cosmetic improvement was not satisfactory despite objective surgical success. In this series, one patient in whom an objective reduction of 4.0 mm was achieved did not feel her eye to have improved significantly in terms of ‘eye prominence’.
No patient in our study experienced loss of vision, post-operative haemorrhage or infra-orbital hypoaesthesia. Reported complication rates for endoscopic orbital decompression are low; the procedure is generally accepted as safe.Reference Asaria, Koay, Elston and Bates7–Reference Lund, Larkin, Fells and Adams11 Two procedures (10 per cent of orbits) resulted in post-operative epiphora that was severe enough to warrant DCR surgery. Both cases occurred early in our series and may have related to overly aggressive decompression around the lacrimal sac. The onset of epiphora in both cases was delayed, occuring more than six months following endoscopic decompression.
Epiphora following decompression is well recognised.Reference Lund, Larkin, Fells and Adams11 Lund et al. reported two patients in their series who developed mild epiphora but did not need surgery. Between 2 and 16 per cent of patients have persistent epiphora following transantral-ethmoidal decompression.Reference Colvard, Waller, Neault and DeSanto14, Reference Seiff and Shorr15 This usually presents approximately 11 months after surgery. Damage to the tissues around the lower end of the duct and to the tissues surrounding the duct may result in a slow scarring process, leading to obstruction, hence the delayed presentation.Reference Colvard, Waller, Neault and DeSanto14
• Endoscopic orbital decompression is an effective procedure for improving cosmesis in patients with inactive thyroid eye disease and residual proptosis
• Twenty orbits of 15 patients who had undergone endoscopic decompression for dyscosmesis are reported
• After an average follow up of 13 months, the mean reduction in proptosis was 3.7 mm (range 1 to 8 mm)
• Most patients (89 per cent) were satisfied with the cosmetic appearance of their eye following endoscopic decompression surgery, and all patients reported a reduction in eye prominence
• Patients should be warned about the late post-operative complications of diplopia and epiphora
Four patients (three bilateral decompressions) developed new post-operative diplopia. New onset diplopia is more common in patients undergoing a greater reduction of proptosis or bilateral decompression.Reference Kennedy, Goodstein, Miller and Zinreich10, Reference McCord16 Abduction capacity has been noted to decline by an average of 1.5 mm following bilateral endoscopic orbital decompression. It has been reported to improve to 0.5 mm 156 days after surgery.Reference Neuberger, Nishino, Neuberger, Konen and Michael17 It is expected that patients will experience some diplopia in the immediate post-operative period, due to the retrograde movement of the globe medially and inferiorly. Vision returns to a pre-operative level a few months after surgery.Reference Metson, Dallow and Shore8, Reference Lund, Larkin, Fells and Adams11 In some cases, post-operative tissue oedema and inflammation may delay the resolution of diplopia. Extra-ocular muscle surgery generally should not be performed until after this time. Koay et al. reported one patient in their series who had post-operative diplopia that resolved three months after decompression.Reference Koay, Bates and Elston9
Conclusions
Endoscopic orbital decompression is an effective procedure for improving cosmesis in patients with inactive thyroid eye disease. Unlike other forms of decompression, the endoscopic procedure does not leave a facial scar. The results of the present study indicate that the complication rate is not insignificant, with 20 per cent of cases developing short or medium term diplopia, and 10 per cent developing late onset epiphora requiring DCR surgery. Generally, our patients were very satisfied with the improvement in eye cosmesis and reported a reduction in eye prominence following endoscopic decompression. Patients considering such a procedure should be warned about the possible risks of diplopia and epiphora.




