Introduction
Frontal sinus cerebrospinal fluid (CSF) leaks have traditionally been repaired using an external approach with osteoplastic flaps and obliteration of the sinus. Endoscopic repair of frontal sinus CSF leaks are a challenge; the major limiting factors to this approach are CSF leaks at the superior or lateral extensions and within the posterior table of the frontal sinus. These are beyond the reach of current instrumentation.Reference Woodworth, Schlosser and Palmer1 It has generally been recommended that extradural techniques be used to repair frontal sinus defects, rather than transnasal endoscopy, in order to enable better access and thus a better repair.Reference Marshall, Jones and Robertson2 The modified Lothrop procedure, traditionally used for intractable sinus disease, widens access to the frontal sinus, thus reducing the need for extracranial and intracranial approaches with their associated morbidities. This case study highlights the fact that lateral frontal sinus CSF leaks can be repaired using the endoscopic modified Lothrop technique. To our knowledge, this approach has not previously been described in the repair of poorly accessible frontal sinus CSF leaks.
Case report
A 60-year-old man with a history of epileptic seizures, intermittent rises in intracranial pressure and sinusitis presented initially in 1997 with a spontaneous, left-sided CSF leak. He was found to have a small dehiscence in the posterior wall of the left fronto-ethmoidal recess. This was endoscopically repaired using mucosal flap, cartilage graft and fibrin glue.
The patient subsequently developed further spontaneous leaks from the same site in 2001 and 2005, requiring endoscopic revision repairs.
In 2006, the patient presented again with left-sided nasal rhinorrhoea, which was confirmed as a CSF leak by beta-transferrin testing. He was advised that the best treatment was an open approach to repair this fourth occurrence of CSF leak, in association with a lumbo-peritoneal shunt to control the intermittent rises in intracranial pressure. However, the patient rejected this in preference to an endoscopic repair, despite our explanation of the likelihood of recurrence. It was therefore decided to attempt an endoscopic repair, with conversion to an open approach if necessary. The patient gave appropriate consent.
A high resolution computed tomography (CT) scan of the sinuses showed the left frontal sinus to be filled with soft attenuation tissue, thought to be CSF, although no definite leak was demonstrated (Figure 1). A BrainLab (Munich, Germany) infrared image guidance navigation system was used, with fluorescein injected via a lumbar drain to aid in localising any potential areas of CSF leak. A decision was made to use an endoscopic modified Lothrop approach in order to prevent future sinusitis and to identify other potential leaks.

Fig. 1 Coronal computed tomography scan showing complete opacification of the left frontal sinus.
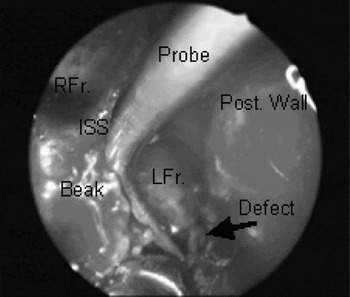
The left fronto-ethmoidal recess was identified and found to have new bone formation. The frontal beak and the new bone were drilled and a septectomy performed. The right fronto-ethmoidal recess was identified and enlarged. The inter-sinus septum was drilled out and wide access obtained. No CSF leak was evident in the previously repaired area; however, a new, 3 × 3 mm dehiscence was identified in the left lateral frontal sinus wall (Figure 2). Despite the defect being in the most lateral area of the sinus, it was easily reached using conventional frontal sinus instruments through the wide access. The access was further enhanced by inserting the endoscope through the left nasal cavity and the instruments through the right.

Fig. 2 Endoscopic view of the frontal sinuses following a modified Lothrop approach, demonstrating the defect in the lateral wall of the left frontal sinus (arrow), and a frontal probe within the sinus cavity. RFr = right frontal sinus; LFr = left frontal sinus; ISS = inter-sinus septum; post = posterior
The defect was closed with fat, fascia lata and free mucosal grafts interspersed with fibrin glue (TisseelTM, Baxter Corporation, Mississauga, Ontario, Canada), then covered with Gelfoam (New York, USA). The left nasal cavity was packed with a Whitehead varnish pack.
Post-operatively, antibiotics were prescribed and the lumbar drain left in situ, draining 10 ml/hr for the first post-operative week. After one week, the drain was clamped then removed, the nasal pack was removed and the antibiotics stopped. The patient was then discharged home with no complications. There was no recurrence or complications at 12 months' follow up.
Discussion
The endoscopic transnasal modified Lothrop approach has been used to treat chronic sinusitis that fails to resolve with less aggressive surgery. Recently, it has also been utilised to excise frontal sinus osteomas.Reference Ulualp, Carlson and Toohill3 However, it has not previously been described as an approach for the repair of CSF leaks.
The endoscopic modified Lothrop procedure was first described by Draf Reference Draf4 and popularised by Gross et al. Reference Gross, Gross, Becker, Moore and Phillips5 The procedure is one of the many techniques that are used for revision endoscopic sinus surgery for persistent frontal sinus disease that has failed primary endoscopic repair. The procedure was devised as an alternative to open approach osteoplastic frontal sinus obliteration for the treatment of refractory frontal sinusitis.
The endoscopic modified Lothrop procedure involves removing the upper nasal and inter-frontal sinus septums and the frontal sinus floor. This creates a common drainage pathway for both frontal sinuses and also creates better access to the lateral aspects of the frontal sinuses. This transnasal approach avoids external incisions and their associated morbidity; however, the technique has been said to be limited in patients with frontal sinuses that have a narrow antero-posterior depth, narrow frontal sinus floor and hard bone in the nasal beak.Reference Sonnenburg and Senior6
The endoscopic approach has become the preferred technique for the surgical management of patients with CSF leaks, with the literature reporting an 85–100 per cent success rate for endoscopic repair of CSF leaks. This compares favourably with reported success after transcranial repair.Reference Carrau, Snyderman and Kassam7 It was found that patients with high BMI (Body Mass Index = weight (Kg)/height2 (m2)), massive skull base defects and spontaneous CSF leaks have a higher repair failure rate.Reference Lindstrom, Toohill, Loehrl and Smith8 Spontaneous CSF leaks are difficult to repair surgically, with a recurrence rate of 25–87 per cent, compared with less than 10 per cent for most other cases.Reference Mirza, Thaper, McClelland and Jones9 The use of a lumbar drain is recommended when a previous repair has been attempted, and also in patients at a high risk of failure.Reference Hegazy, Carrau, Snyderman, Kassam and Zweig10
• Cerebrospinal fluid (CSF) leaks can occur in the frontal sinus
• Frontal sinus CSF leaks are usually repaired through either an open osteoplastic or transnasal endoscopic approach
• This case illustrates the use of standard nasal endoscopic instrumentation for repair of these leaks, through the wider access afforded by the endoscopic modified Lothrop procedure
Expansion of the endoscopic approach together with improved equipment and experience have led to CSF leaks of the anterior, sellar and parasellar skull base becoming easily accessible. However, defects that extend superiorly or laterally within the posterior table of the frontal sinus have traditionally necessitated an extracranial osteoplastic flap with or without obliteration,Reference Woodworth, Schlosser and Palmer1, Reference Marshall, Jones and Robertson2 due to limited access and difficulty in instrumentation.
The present case illustrates the fact that CSF leaks in poorly accessible areas of the frontal sinus can be repaired using the endoscopic modified Lothrop procedure. The method not only gives access to the posterior wall of the fronto-ethmoidal recess but allows for access both superiorly and laterally. Although reports on endoscopic repair of the posterior fronto-ethmoidal recess exist,Reference Chatrath and Saleh11 they do not describe use of the modified Lothrop method. In the present patient, any part of the frontal sinus could be accessed using this approach. Furthermore, the modified Lothrop method was also used for the concurrent treatment of sinusitis. It must be noted, however, that this patient had average-sized frontal sinuses. We would envisage that the access may be more difficult in patients with very large frontal sinuses, possibly necessitating the design and production of longer curved instruments for such anatomically challenging cases.