Introduction
Pyriform fossa sinus tracts are widely cited as accounting for 3–10 per cent of all branchial anomalies, and arise from the failed obliteration of the third and fourth branchial structures.Reference James, Stewart, Warrick, Tzifa and Forte 1 Although third and fourth sinus tracts may be embryologically and anatomically distinct, this difference can only truly be perceived on extensive surgical exploration of the neck and mediastinum. Additionally, as management of the two pathologies is identical, recent authors have argued that this distinction is clinically unimportant,Reference Huang, Peng and Hsu 2 and that these anomalies should be referred to collectively as pyriform fossa sinus tracts.Reference Lachance and Chadha 3
Pyriform fossa sinus tracts are most commonly encountered in children, who present with neck abscess, recurrent infections and suppurative thyroiditis, overwhelmingly occurring on the left side of the neck.Reference Josephson and Black 4 There are published cases of pyriform fossa sinus tracts in adults;Reference Kruijff, Sywak, Sidhu, Shun, Novakovic and Lee 5 however, because of their small numbers, they are often excluded by literature reviews.Reference Lachance and Chadha 3
The diagnosis of pyriform fossa sinus tracts can be made from a variety of investigations, with direct visualisation on laryngoscopy being the most definitive.Reference Josephson and Black 4 The management of pyriform fossa sinus tracts has evolved over the years, from the traditional approach of total surgical excision of the sinus tract towards less invasive endoscopic cauterisation of the sinus opening.Reference Derks, Veenstra, Oomen, Speleman and Stegeman 6
This paper describes a highly unusual presentation of pyriform fossa sinus tract, with an interesting pathological sequela, and the unique use in an adult of a specific management technique.
Case report
A 79-year-old female presented to our institution with a large left-sided neck mass and severe odynophagia of 3 days’ duration. She had visited her primary care physician the day prior to hospital presentation, who prescribed the patient a course of oral antibiotics. However, symptom progression triggered emergency department attendance. The patient was previously healthy, with past diagnoses limited to hypertension and fully treated breast carcinoma. She had never previously suffered from similar symptoms.
The patient's airway was compromised, with an oxygen saturation level of 91 per cent on room air and a respiratory rate of 29 breaths per minute. Flexible nasendoscopy revealed fullness of the left lateral and retropharyngeal walls, and a swollen left arytenoid. Initial laboratory investigations provided evidence of an infectious aetiology, with a neutrophil count of 17 300 cells/μl (indicating neutrophilia) and a C-reactive protein level of 523 mg/dl.
The patient was started on intravenous piperacillin/tazobactam (Tazocin®), metronidazole and dexamethasone. A nasogastric tube was placed given the severity of odynophagia.
Computed tomography (CT) was the initial imaging modality. This demonstrated a ring-enhancing lesion adjacent to the thyroid, on the left, prompting further investigation.
Magnetic resonance imaging (MRI) revealed large-volume, loculated collections extending from the left thyroid region, superiorly through the neck, to the left submental space (levels II–IV), with deep extension into the left parapharyngeal space, retropharyngeal spaces, hypopharynx and the left carotid space (Figure 1a–c). Additionally, inferior extension into the thoracic inlet had produced radiologically mild superior mediastinitis. The diffusion pattern favoured a fluid collection of 95 × 50 × 35 mm in maximal size, which was indistinguishable from the left lobe of the thyroid gland, with a normal right thyroid lobe. Furthermore, the left internal jugular vein (IJV) appeared thrombosed, with evidence of thrombophlebitis from the infrahyoid neck to the distal portion of the left sigmoid dural venous sinus, through the jugular foramen. These findings were confirmed during ultrasound-guided aspiration, where 2 ml of frank pus was aspirated.

Fig. 1 Magnetic resonance imaging scans of the neck (T2-weighted turbo inversion recovery magnitude sequences), showing axial (a), coronal (b) and sagittal (c) sections of the 95 × 50 × 35 mm fluid collection.
The investigations indicated a diagnosis of acute suppurative thyroiditis, deep neck abscess formation and radiologically evidenced Lemierre's syndrome. The underlying aetiology was unclear, although a pyriform fossa sinus tract was mooted.
The patient was taken to the operating theatre on the 2nd day of admission for abscess incision and drainage, and endoscopic evaluation. Drainage was performed via a 5 cm collar incision. The thyroid isthmus was divided with bipolar diathermy. Over 20 ml of pus was drained from the deep neck spaces and 20 ml of serosanguinous fluid was aspirated from the left lobe of the thyroid gland. Following washout, two corrugated drains were strategically placed with north to south angulation across loculations, to allow gravity-assisted drainage.
Subsequently, a pharyngoscope was utilised to visualise the larynx and local internal structures. Endoscopic assessment of the larynx revealed no abnormalities. In order to assess the left pyriform fossa, the pharyngoscope was heavily angulated, exiting opposed to the right oral commissure. A lesion in the left pyriform apex was identified. External pressure to the left side of the neck caused the expression of pus from the lesion, and on closer inspection a deeply penetrating fistula could be seen (Figure 2). An intra-operative diagnosis of pyriform sinus fistula was made, and endoscopic management was elected.
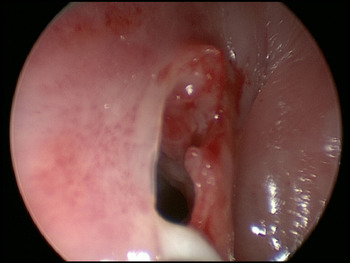
Fig. 2 Endoscopic image of the deeply penetrating fistula arising from the left pyriform sinus apex (with white pus exiting the tract lumen into the hypopharynx, along the floor of the sinus mouth).
Laryngeal suction and cupped forceps enabled cold dissection of the lesion, with subsequent monopolar diathermy electrocauterisation (20 W) used sparingly circumferentially at the entrance to the fistula tract. Fibrin glue (Tisseel™) was immediately available and chosen to obliterate the sinus tract. Using the manufacturer-provided endoscopic applicator, 2 ml of Tisseel was applied to the sinus until no pharyngeal communication remained (Figure 3).

Fig. 3 Endoscopic image of the lesion immediately following fibrin glue application.
The patient recovered well post-operatively. Pus aspirate cultures revealed moderate Gram-positive cocci growth and scanty Gram-positive rod growth on microscopy, both sensitive to amoxicillin. No anaerobes were cultured. Blood cultures were negative. She remained on intravenous antibiotics as an in-patient for 10 days following surgery, without oral antibiotics on discharge. Following haematology consultation, the patient was started on a three-month course of Coumadin® (warfarin) in light of the IJV thrombosis.
At one-, four- and seven-month office follow-up evaluations, the patient was symptom-free, with no obvious sinus tract visible on flexible nasolaryngoscopy. The patient was counselled on further treatment options, with a choice primarily between surgical management involving thyroidectomy and sinus tract excision, or watchful waiting with interval repeat scanning. The patient chose the latter, and MRI four months post-operatively showed no sinus recurrence or fluid collection.
Discussion
The case of pyriform fossa sinus tract described in this paper, which presented as a left-sided neck abscess and suppurative thyroiditis, is classical. However, this patient was much older than other adult cases described in the literature.Reference Kruijff, Sywak, Sidhu, Shun, Novakovic and Lee 5 , Reference Parker, Clary and Courey 7 Furthermore, unusually, this patient had no previous symptoms or presentations. In addition, the co-existence of IJV thrombophlebitis with a branchial infection is rare, although it has been previously reported.Reference Lwin and Lohani 8
-
• Pyriform fossa sinus tracts classically present as neck abscess, recurrent infections and suppurative thyroiditis in children
-
• Acute, de novo presentation of a pyriform fossa sinus tract in a geriatric patient is highly unusual
-
• The co-existence of internal jugular vein thrombophlebitis with a branchial infection is rare, but has been previously reported
-
• Endoscopic and open surgical management have comparable results, but the former is less invasive and has lower morbidity, and should be a first-line treatment
-
• Endoscopic cauterisation by laser, electrocautery and trichloroacetic acid appear to have comparable efficacy
-
• This paper describes the first use of fibrin glue to obliterate a pyriform fossa sinus tract in an adult
While the potential for an underlying pyriform fossa sinus tract was raised by CT and MRI, a definitive diagnosis was made by direct visualisation of the pyriform fossa sinus tract opening on laryngoscopy. The pyriform fossa sinus tract seen in this patient was deemed to be a fourth branchial arch anomaly, as the opening was at the apex of the pyriform sinus, rather than more cranially, which is a characteristic of third arch anomalies. However, surgical exploration of the sinus tract would have been required to confirm fourth branchial arch aetiology.
The ability to diagnose and treat pyriform fossa sinus tracts in one procedure, while simultaneously performing incision and drainage of a neck abscess, is one of the advantages that has led authors to propose endoscopic cauterisation ahead of open surgical excision of the sinus tract.Reference Derks, Veenstra, Oomen, Speleman and Stegeman 6 Recent reviews have suggested that endoscopic and open surgical management have comparable results, but as endoscopic treatment is less invasive and has lower morbidity, it should be a first-line treatment for pyriform fossa sinus tracts.Reference Josephson and Black 4 , Reference Derks, Veenstra, Oomen, Speleman and Stegeman 6
There have been several techniques described for cauterising the internal openings of pyriform fossa sinus tracts. The most common of these techniques are electrocautery, laser and trichloroacetic acid, all of which appear to have comparable efficacy.Reference Lachance and Chadha 3 Fibrin glue is a multifunctional sealant used in a range of surgical settings. In the treatment of pyriform fossa sinus tracts, fibrin glue has been described as an aid to open surgeryReference Piccioni, Bottazzoli, Nassif, Stefini and Nicolai 9 and as an adjunct to laser cauterisation.Reference Huang, Peng and Hsu 2 However, it has only once been previously described as the sole method for pyriform fossa sinus tract closure in a paediatric setting, and in that case there was no recurrence.Reference Cigliano, Cipolletta, Baltogiannis, Esposito and Settimi 10 Minimally invasive surgery and endoscopic application of fibrin glue was chosen in this case because of the atypical presentation in a previously well septuagenarian. The morbidity and potential complications associated with a more radical operation (involving thyroidectomy, and extensive neck and mediastinal exploration for complete excision of the tract) would not be insignificant in the elderly. Hence, a less invasive technique was adopted as the first-line treatment to manage the acute situation, with close surveillance follow up to ensure complete resolution and the absence of any symptom recurrence.
The case described highlights an unusually late presentation of pyriform fossa sinus tract with the clinical correlate of Lemierre's syndrome. The condition was successfully managed endoscopically. This is only the second published case utilising fibrin glue as the principal method of pyriform fossa sinus tract closure, and the first in an adult.





