Introduction
Tracheal stenosis post laryngectomy has always been a dilemma for both the surgeon and the patient. It can result in the patient having a permanent tracheostomy, a silicone stomal tube or a button to ensure stoma patency, which is often inconvenient and not cosmetically pleasing. Many may have to undergo revision stomaplasty. If neglected, the stenosis can progress and result in airway obstruction, representing a medical emergency.
An adequate tracheostoma is said to be approximately three-quarters of the size of a thumb, whereby the thumb is sufficient to obstruct the tracheostoma for patients with a tracheoesophageal puncture and voice prosthesis to vocalise. Tracheostomal stenosis can be caused by surgical technique or patient factors.
Surgical techniques involving excess peristomal skin not excised during tracheocutaneous anastomosis, and the use of a vertical tracheal incision, have been associated with stenosis.Reference Griffith and Luce1 Other factors include: incorporating a transverse neck dissection wound as part of the superior border of the stoma, the usage of braided sutures and failure to ensure a tension-free tracheocutaneous anastomosis. Failure to release the sternal head of the sternocleidomastoid may result in a deep and retracted tracheostoma.
Patient factors associated with tracheostomal stenosis include: perichondritis secondary to exposed cartilage, especially if it involves the upper tracheal rings; use of a tracheal cannula that is regarded as a foreign body; and an anatomically small trachea. Tracheal size is not strictly a factor, but stenosis is worse in a small trachea compared to a larger trachea with regard to the airway available for respiration.
Radiation, administered either pre- or post-operatively, was thought to be a contributing factor, via endarteritis, with subsequent scarring and fibrosis; however, opinions are divided. Griffith and LuceReference Griffith and Luce1 showed that pre-operative radiotherapy, and combined pre- and post-operative radiotherapy, were not significant in the development of tracheostomal stenosis. These findings were supported by Kuo et al.Reference Kuo, Ho, Wei and Lam2
The current paper describes a new technique of end tracheal stomaplasty performed during laryngectomy. This innovative surgical technique is a modified version of the star and petal techniques.
Surgical technique
The neck area is cleaned and draped. A total laryngectomy is performed with or without neck dissection. The bilateral sternal heads of the sternocleidomastoid muscle are released. A horizontal incision is made through the trachea, separating it from the larynx superiorly. The posterior tracheal wall is released from the oesophagus at the tracheoesophageal groove. The fish mouth technique for creating a tracheostoma post laryngectomy can be described in four facile steps, as described below.
Step one
A circle incision shape is marked at the midline of the neck where the tracheostoma is planned. Ideally, the incision should be lower and not incorporate the existing transcervical incision superiorly (Figure 1).
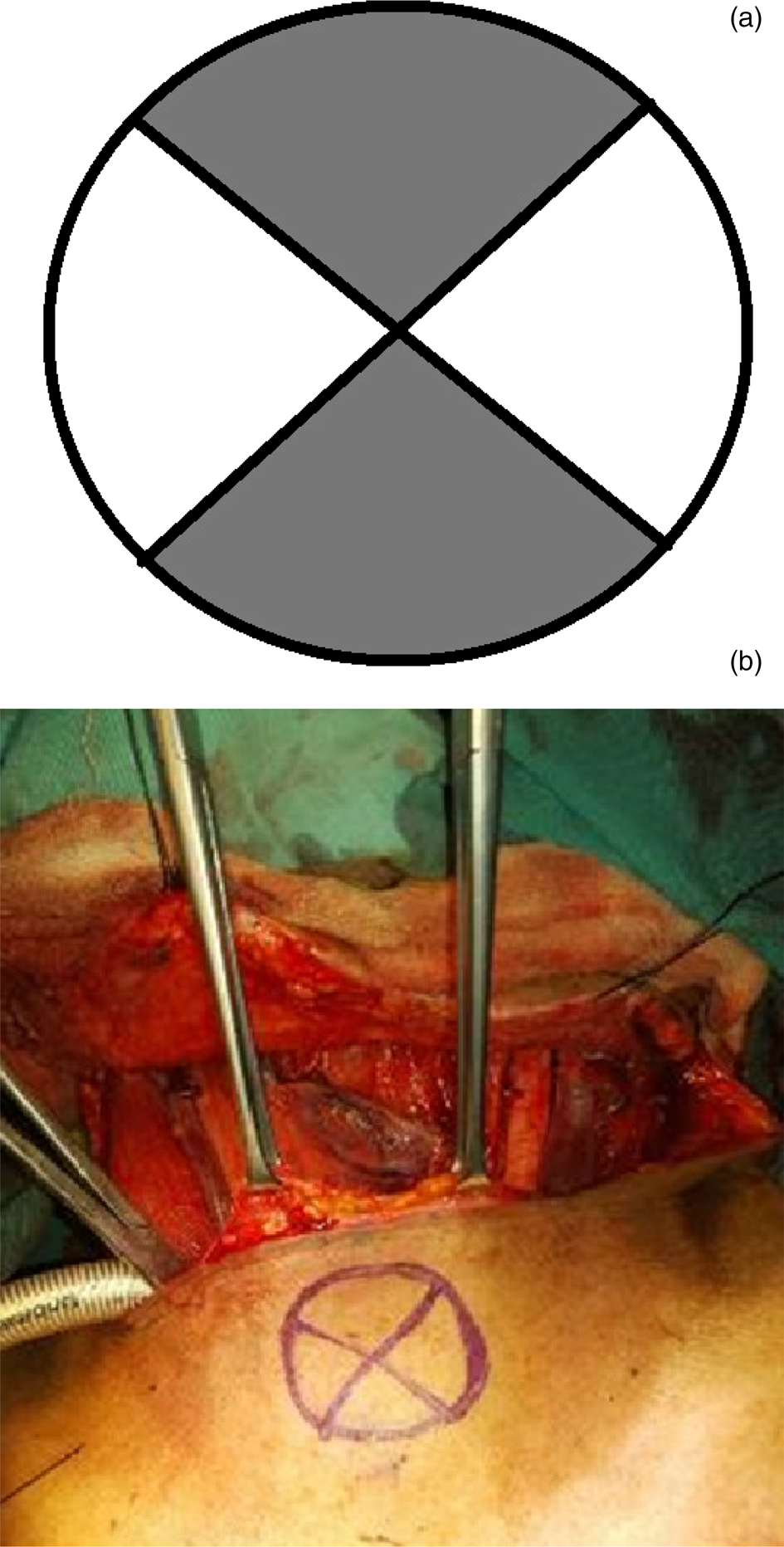
Fig. 1. (a) The superior and inferior (grey) quadrants represent the discarded flaps. (b) Stoma placement is marked inferiorly to the transcervical incision.
Step two
Two incisions are made within the circle (crossing each other), resembling an ‘X’ shape, to form four flaps. The superior and inferior skin flaps of the ‘X’ are excised and discarded, leaving the two lateral skin flaps at the 9 and 3 o'clock positions (Figure 2).
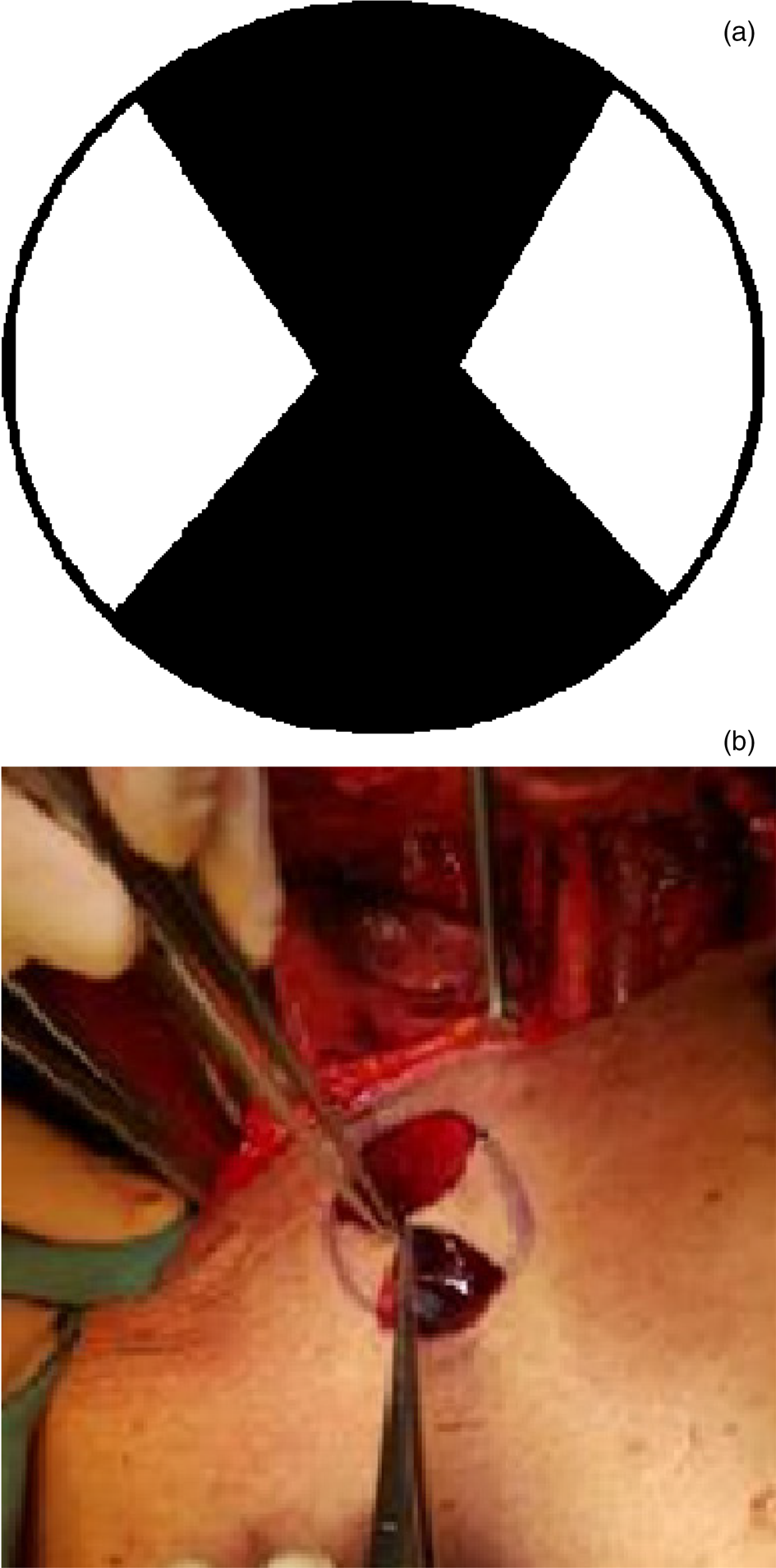
Fig. 2. (a) The superior and inferior skin flaps are cut along their outer circumference, leaving these (black) areas void of skin superiorly and inferiorly. (b) The remaining skin flaps at the 3 and 9 o'clock positions are held by tissue grasping forceps.
Step three
A horizontal incision is made at the 3 and 9 o'clock positions of the lateral tracheal wall to form a cleft. The depth of the incision is approximately one tracheal ring deep (Figure 3).
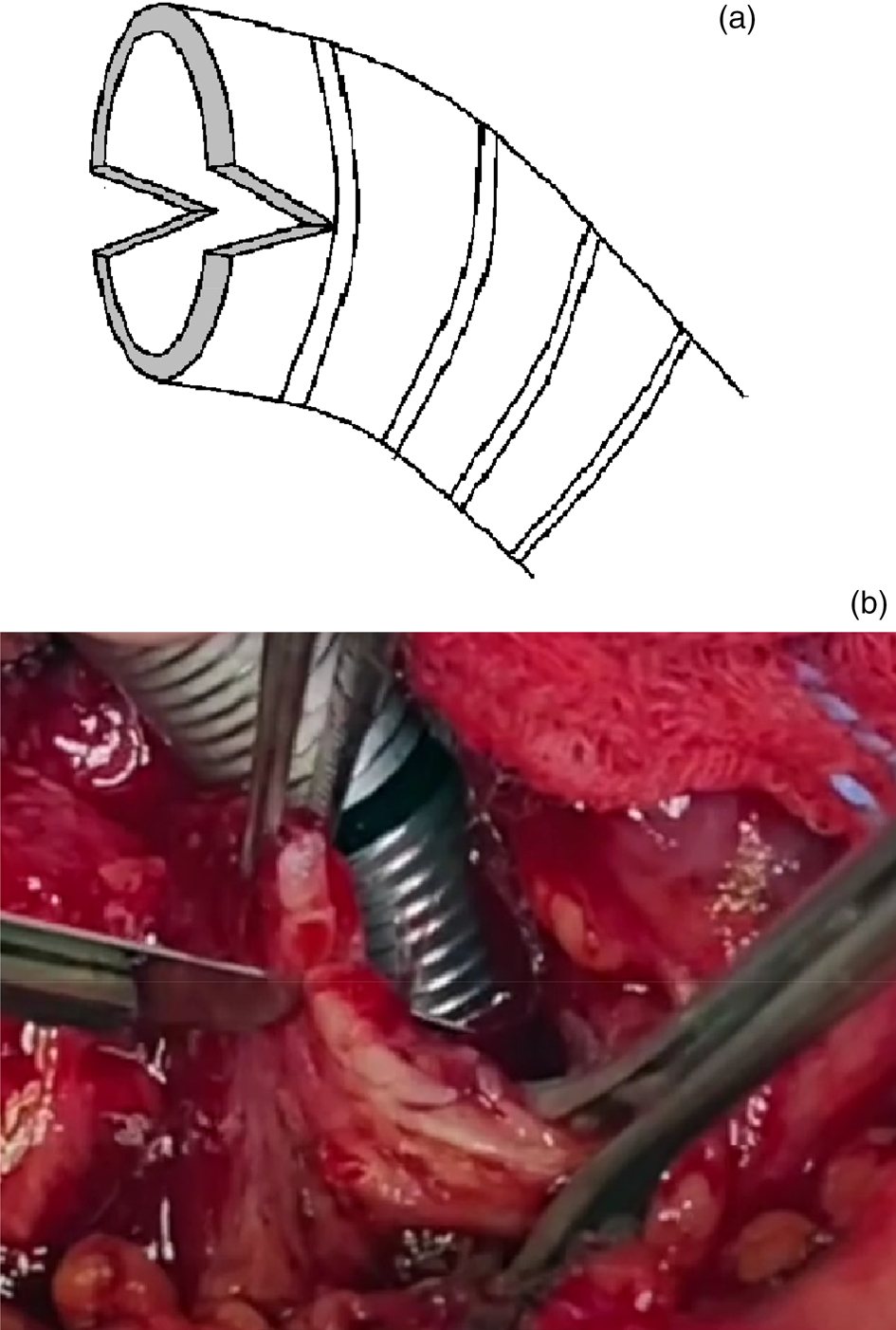
Fig. 3. (a & b) Both horizontal incisions at the lateral tracheal wall are similar in depth, forming a valley on either side. This increases the superior inferior diameter along the vertical axis of the trachea.
Step four
The two lateral skin flaps are sutured within the lateral tracheal clefts (made by the two horizontal incisions) and sutured with a non-absorbable suture. The triangular apex of the skin flap is first sutured to the inferior-most region of the tracheal cleft via an interrupted technique. The sutures are then placed proximally to the base of the flap and surrounding the tracheocutaneous junctions at the superior and inferior tracheal arc. Care is taken to not expose any tracheal cartilage. Exposed cartilage should be covered with skin and sutured (Figure 4).
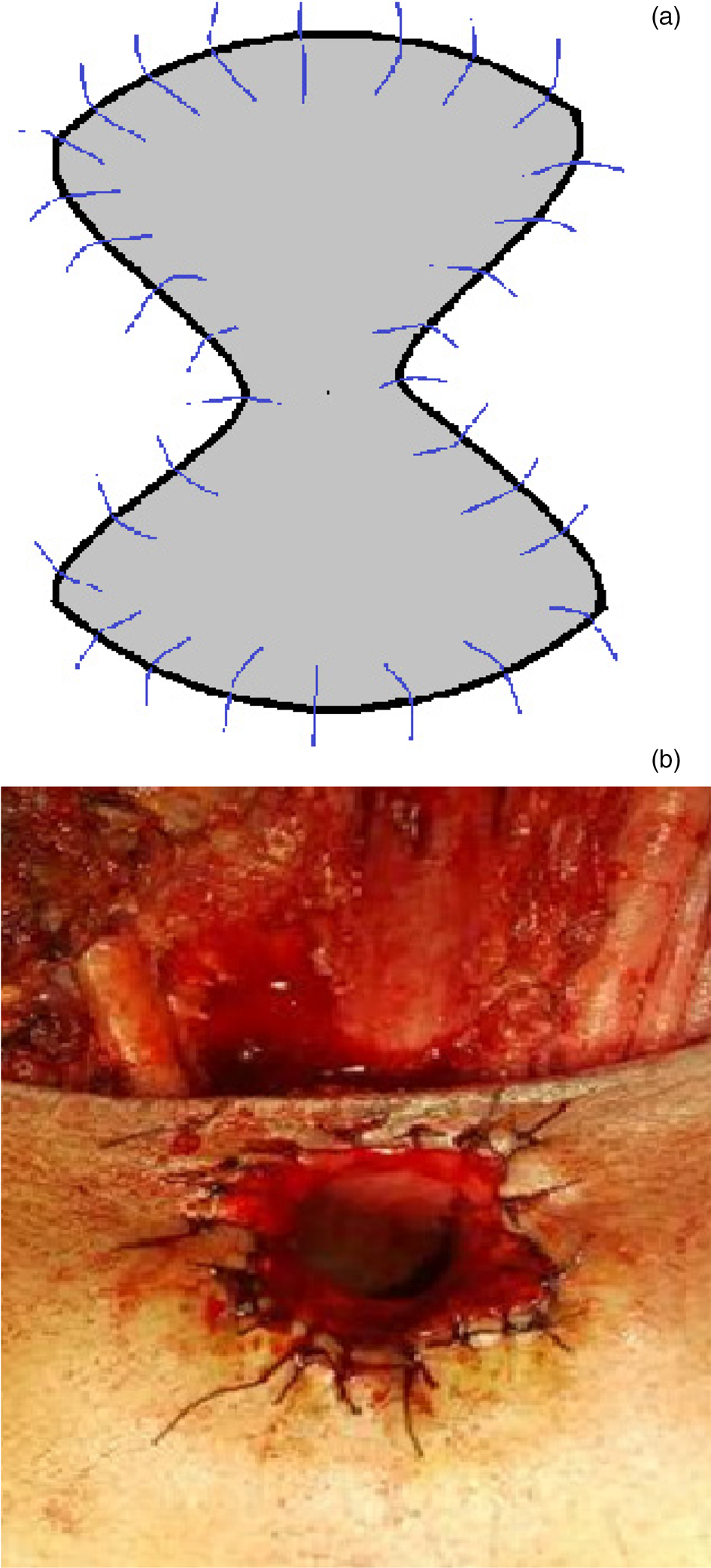
Fig. 4. (a) The skin flaps are sutured within the valley of the lateral tracheal wall incisions. The increase in the vertical axis of the tracheal opening, with a skin flap sutured inwards on either lateral side of the trachea, gives the impression of a fish mouth. (b) Non-absorbable monofilament sutures are used.
The procedure results in an elongated, broadened and elliptical tracheostoma that resembles the mouth of a fish (Figure 5).
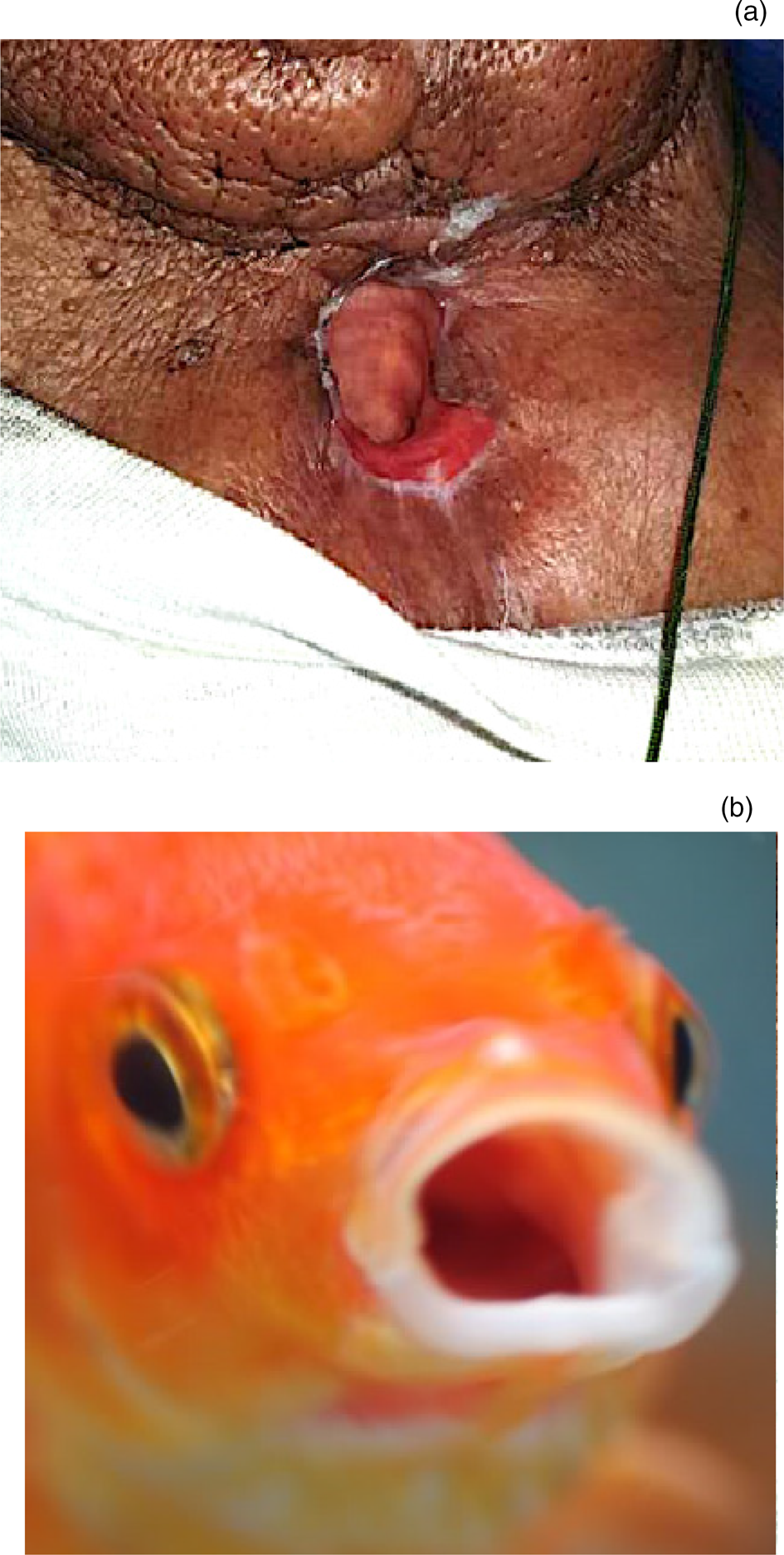
Fig. 5. (a) The tracheostoma three months after a total laryngectomy, (b) performed using a technique in which the end result resembles an open fish mouth.
Discussion
Many techniques have been described to avoid tracheal stenosis. The fish mouth technique is an innovative technique to prevent tracheostomal stenosis. Other techniques previously described in the literature to prevent tracheal stenosis are the star technique described by Lam et al.Reference Lam, Wei, Wong and Ong3 and the petal technique described by Lucioni et al.Reference Lucioni, Rizzotto, Pazzaia and Serafini4 All three procedures involve a flap advancement technique.
The hallmark paper by Lam et al.Reference Lam, Wei, Wong and Ong3 (1983) described a zig-zag technique or a serrated suture line along the tracheocutaneous junction. Some even refer to it as the classic star technique. An ‘X’-shaped oblique incision is made on the skin, and the four skin flaps located at 12, 3, 6 and 9 o'clock are sutured to the underlying trachea. One in 25 patients (4 per cent) in that study developed tracheostomal stenosis post procedure.Reference Lam, Wei, Wong and Ong3 Kuo et al.Reference Kuo, Ho, Wei and Lam2 described a similar technique, with a 15 per cent stenosis rate.
Two decades later, Lucioni et al.Reference Lucioni, Rizzotto, Pazzaia and Serafini4 (2003) described the petal technique used for revision of tracheostomal stenosis. Two incisions in the shape of a petal are cut at the 4 and 8 o'clock positions and the skin is excised. The inferior skin flap between the petals is retracted inferiorly and sutured to the inferior apex of the trachea.Reference Lucioni, Rizzotto, Pazzaia and Serafini4 Forty out of 59 patients in that study had an immediate satisfactory outcome.Reference Lucioni, Rizzotto, Pazzaia and Serafini4
There are three cardinal requirements for an adequate tracheostoma: it needs to be large enough for respiration and secretions, self-sufficient (therefore not requiring a stent), and adequate for thumb occlusion for speech production.Reference Capper and Bradley5
Lam et al.Reference Lam, Wei, Wong and Ong3 described skin flaps sutured to the trachea at all four quadrants: superior, inferior, right lateral and left lateral. In Lucioni's petal technique,Reference Lucioni, Rizzotto, Pazzaia and Serafini4 only the inferior skin flap is sutured to the trachea. In our improved technique, the superior and inferior flaps are discarded; therefore, the superior and inferior quadrants of the skin surrounding the tracheostoma are excised and not advanced inwards into the trachea. Only the right and left lateral borders are advanced inwards by the lateral skin flaps.
Similar to the petal technique, the fish mouth technique spares the upper tracheostomal arch. Lucioni and colleagues’Reference Lucioni, Rizzotto, Pazzaia and Serafini4 claim that tracheal stenosis does not involve the posterior wall of the trachea which consists of the trachealis muscle and is void of circumferential tracheal cartilage. The superior arch will be sutured to the posterior tracheal wall when the trachea is brought out as a stoma. The void of skin superiorly in the fish mouth technique allows for adequate clearing at the superior tracheostomal border, to accommodate a primary or secondary tracheoesophageal puncture for a voice prosthesis. The fish mouth technique has a strong advantage for preventing stoma stenosis as it is conducted during a laryngectomy. The petal technique, in contrast, is performed during stomaplasty, after the stoma stenosis has occurred. Therefore, the former technique is preventative, whilst the latter represents the salvaging or repairing of a stoma stenosis.
The star technique was described, by Lam et al.,Reference Lam, Wei, Wong and Ong3 prior to the invention of a voice prosthesis placement with a tracheoesophageal puncture, such that a tracheoesophageal puncture will not be possible with this technique, or will be too close to the apex of the superior skin flap that is advanced into the trachea. This predisposes the tracheoesophageal puncture to contraction, granulation and infection. The fish mouth technique allows for adequate clearing at the superior border of the tracheostoma which is void of a skin flap superiorly. This subsequently also allows adequate access, with easy visualisation for cleaning of a voice prosthesis by patients using a mirror.
The two lateral skin flaps advanced into the lateral tracheal wall incision should not exceed 90 degrees or one-quarter of the circumferential diameter of the tracheostoma. Similarly, the depth of the two horizontal incisions on the lateral tracheal wall should not be too deep and not exceed that of two tracheal rings. This is to avoid excessive pull by the skin flap laterally. This results in a very broad and elliptical tracheostoma. Excessive pull laterally may compromise the integrity of the superior arc and result in collapse of the superior arc. In such cases, the patient may require a cannula or button to ensure stoma patency.
Exposed cartilage should be avoided at all costs, to prevent tracheostomal stenosis secondary to perichondritis. The authors prefer a straight horizontal cut of the trachea when separating it from the larynx, instead of bevelling; the latter exposes tracheal cartilage, which may lead to necrosis and infection.Reference Capper and Bradley5 Failure to release the sternal heads of the sternocleidomastoid may result in lateral compression or vertical slits.Reference Montgomery6
Non-absorbable monofilament sutures are preferred to absorbable braided sutures, as the former glide easily and have fewer infection risks, with no pits between filaments to harbour bacteria.Reference Parell and Becker7 Interrupted sutures are favoured, as a failure in one knot will not be catastrophic to the integrity of the other knots. However, sutures at the tracheocutaneous junction may trap mucus and tracheal secretions, and one should therefore be aware of crusting. Frequent toileting is required to reduce bacterial load and risk of infection. Care should be taken when removing the sutures, especially those at the apex of the advancement flap which is situated deep within the trachea, to prevent an airway foreign body.
Post-operatively, no cannula (or tracheostomy tube) is used as the tracheostoma is often large enough for respiration. A cannula is only used if the patient still requires post-anaesthesia ventilation with a tube cuff; this is removed once the patient has been weaned off the ventilator.
Modifications to the technique can be made in several ways if needed. For instance, significant tumour involvement of the anterior neck may require local or free flap reconstruction surrounding the superior arc of the tracheostoma. In cases of subglottic involvement, adequate tracheal release is pertinent for tracheal mobilisation in order to achieve a tension-free anastomosis. No technique change is required in a pre-radiated neck, unless there is tumour involvement of the soft tissue.
Conclusion
The fish mouth tracheostoma is an innovative and easily reproducible technique suitable for modern-day voice rehabilitation with primary or secondary tracheoesophageal puncture surgery for a prosthesis. Indeed, it may considerably reduce the incidence of tracheostomal stenosis.
Acknowledgement
The authors would like to thank the medical doctors of the Department of Otorhinolaryngology, Head and Neck Surgery, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia, for their assistance in performing this surgical technique on the patients.
Competing interests
None declared







