Introduction
Tympanoplasty is a common otological intervention, with the primary goals of a healthy middle-ear cavity and improved hearing. In the literature, various factors are reported to affect surgical outcomes in tympanoplasty, such as age, perforation size and location, condition of the contralateral ear, graft type, and middle-ear and mastoid bone pneumatisation.Reference Zollner1,Reference Yegin, Celik, Simsek, Masallah, Olgun and Aylin2
The middle ear is a very complex anatomical structure. It is a narrow chamber located in the tympanic part of the temporal bone, covered with mucosa, and contains air. It transmits vibrations from the outer-ear canal to the inner ear through the tympanic membrane and ossicles. At birth, the middle-ear cavity is filled with air. The main factor in the postnatal development of middle-ear volume is skull growth in the vertical axis. The middle-ear volume in adult individuals is 1.5 times larger than that in infants.Reference Virapongse, Rothman, Kier and Sarwar3 Although there is an increase in middle-ear volume with age, a strong correlation has not been shown between the two.Reference Kavakli, Ogeturk, Yildirim, Karakas, Karlidag and Sarsilmaz4 It has been reported that middle-ear volume is larger in males than in females.Reference Ikui, Sando, Haginomori and Sudo5 The middle ear is posteriorly connected to mastoid cells through the aditus ad antrum. The mastoid air system is one of the most important structures for the functional balance of the middle ear. Mastoid air cells are the air reservoir for the middle ear and play an important role in the physiological functions of the middle ear by taking part in the regulation of heat and pressure.Reference Lee, Jun, Kim, Jung and Yeo6 The development of the mastoid air cell system is completed at an age of about 10 years in females and 15 years in males.Reference Diamant7,Reference Koc, Ekinci, Bilgili, Akpinar, Yakut and Han8
While many studies have reported a success rate of 60–99 per cent for tympanoplasty in adults, this success range is reduced to 35–94 per cent for the paediatric age group.Reference Inwood, Wallace and Clarke9 Incomplete Eustachian tube function and continued development of mastoid pneumatisation in the paediatric group are considered to be the reasons for tympanoplasty failure.Reference Kaya, Benzer, Gode, Sahin, Bilgen and Kirazli10 The decrease in the degree of mastoid pneumatisation may adversely affect the transmission of sound waves through the middle ear and the prognosis of middle-ear disease.Reference Yegin, Celik, Simsek, Masallah, Olgun and Aylin2,Reference Csakanyi, Katona, Josvai, Mohos and Sziklai11,Reference Luntz, Malatskey, Tan, Bar-Meir and Ruimi12
Mastoid pneumatisation has been calculated quantitatively using several methods based on water weight, acoustics and a pressurised transducer.Reference Silbiger13–Reference Andreasson and Mortensson15 Recent and significant advances in computed tomography (CT) have provided better images of the anatomical features of the temporal bone.Reference Lee, Jun, Kim, Jung and Yeo6 For this purpose, multiplanar reconstruction is used.Reference Lee, Jun, Kim, Jung and Yeo6,Reference Koc, Ekinci, Bilgili, Akpinar, Yakut and Han8 This method allows simple and accurate measurements of the degree of mastoid and middle-ear pneumatisation.
To the best of our knowledge, there is no previously published study investigating the effects of mastoid and middle-ear pneumatisation volume, measured using high-resolution CT, on the success of tympanoplasty in paediatric patients. The current study aimed to reveal the effects of mastoid and middle-ear pneumatisation volume on the anatomical and functional success of type 1 tympanoplasty in paediatric patients.
Materials and methods
This retrospective study was conducted in a tertiary healthcare institution with the approval of the clinical research ethics committee (approval number: 2020/17-1). Written informed consent was obtained from the parents or guardians of the children prior to surgery. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Forty-five paediatric patients who were diagnosed with chronic otitis media and who underwent type 1 cartilage tympanoplasty between January 2013 and January 2020 were included. Temporal bone high-resolution CT was performed on all patients to exclude middle-ear pathologies and ossicular chain defects and to determine the presence of soft tissue in the antrum requiring mastoidectomy. The side effects of radiation were explained to all parents prior to high-resolution CT, as was the reason why the high-resolution CT was planned.
The criteria for admission to the study were: the absence of ear drainage for the last three months prior to surgery, no evidence of inflammation, and the absence of ossicular pathology and mastoiditis on high-resolution CT images of the temporal bone. Patients were excluded from the study if they had: ossicular chain defects, cholesteatoma, tympanosclerosis, a history of previous ear surgery, refractory otorrhoea or craniofacial anomaly, and irregular follow-up records. Further excluded were those without pre-operative audiological examination records or temporal bone high-resolution CT images.
For all the patients, in addition to age and gender, the audiological examination findings for the operated ears, the post-operative condition of the graft, and the middle-ear and mastoid volume, were recorded. The minimum post-operative follow-up period of the patients was six months.
Type 1 cartilage tympanoplasty was performed in all patients under general anaesthesia using the retroauricular approach and the overlay–underlay technique. Conchal cartilage was used as the graft tissue. Anatomical success was defined as an intact graft without perforation, lateralisation and a dry ear. The anatomical success of tympanoplasty was evaluated at the sixth post-operative month.
The pre- and post-operative pure tone audiometry tests of the patients were examined, and the bone conduction, air conduction and air–bone gap (ABG) values were recorded. The results of pure tone audiometry were calculated at four frequencies (0.5, 1, 2 and 3 kHz). The changes between the pre- and post-operative ABG values were evaluated. An ABG value of 20 dB HL or less was considered to indicate functional success.
High-resolution computed tomography
All CT images were evaluated by a specialist radiologist (AK). The high-resolution CT images were taken in the axial plane using a Toshiba Aquilion 64-slice CT device (Toshiba Medical, Tokyo, Japan) at 1 mm intervals, without intravenous contrast material administration. Coronal and sagittal multiplanar reconstruction images were constructed. Sections were obtained in such a way as to include the entire temporal bone and important surrounding structures.
Using the segmentation tool in the Horos picture archiving and communication system viewer software,16 regions of interest were manually drawn in each section in the axial and coronal planes based on the conventional anatomical boundaries around the middle ear (Figure 1a) and mastoid bone (Figure 1b). Pneumatised areas were then identified with the threshold algorithm for the air values (Figure 2a and b). Subsequently, manual corrections were performed in each section, and separate regions of interest were created for the air spaces in all sections. These areas were combined with the volume calculator in the Horos picture archiving and communication system viewer to determine the total air volume in cubic centimetres, and three-dimensional (3D) images of the air volume were obtained (Figure 3).

Fig. 1. Using the segmentation tool, regions of interest were manually drawn in each section in the axial and coronal planes, based on the conventional anatomical boundaries around the middle ear (a) and mastoid bone (b). R = right; L = left

Fig. 2. Pneumatised areas were identified with the threshold algorithm for the air values, for the middle ear (a) and mastoid (b). R = right; L = left

Fig. 3. Three-dimensional reconstruction of pneumatisation of a left mastoid bone. L = left
Statistical analysis
Mean, standard deviation, median, minimum and maximum values were used as descriptive statistics for continuous data, with percentages as discrete data. The Shapiro–Wilk test was conducted to examine the conformity of continuous data to the normal distribution. The Wilcoxon test was undertaken for the pre- and post-operative comparison of continuous data, and for comparison of the values between the operated and healthy sides. The Mann–Whitney U test was used to compare volume values according to graft and functional success. The IBM SPSS® Statistics version 20 software program was used for statistical analyses, and p < 0.05 was accepted as the statistical significance limit.
Results
The age of the 45 patients included in the study ranged from 8 to 18 years, with a mean value of 13.33 ± 3.05 years. Of the patients, 46.7 per cent were male and 53.3 per cent were female. Tympanoplasty was performed on the right ear in 42.2 per cent of patients and on the left ear in 57.8 per cent. Disease was unilateral in 77.8 per cent of patients (n = 35) and was bilateral in 22.2 per cent (n = 10) (Table 1).
Table 1. Patient characteristics

SD = standard deviation
The mean pre-operative bone conduction value was 5.87 ± 3.01 dB HL, and the mean post-operative bone conduction value was 6.16 ± 3.59 dB HL. There was no statistically significant difference between the pre- and post-operative bone conduction values (p = 0.739). The mean pre- and post-operative air conduction values were 28.13 ± 10.59 dB HL and 15.58 ± 9.24 dB HL, respectively, indicating a statistically significant difference (p < 0.001). The mean pre- and post-operative ABG values were 22.62 ± 9.91 dB HL and 9.42 ± 7.85 dB HL, respectively. A statistically significant difference was found between the pre- and post-operative ABG values (p < 0.001) (Table 2).
Table 2. Comparison of pre- and post-operative bone conduction, air conduction and air–bone gap in operated ears

SD = standard deviation
For the operated ears, the mean hearing gain value was 13.20 ± 9.71 dB HL. The mastoid volume in the operated ears ranged from 0.05 to 7.22 cm3, with a mean of 1.89 ± 1.59 cm3. The middle-ear volume of these ears varied between 0.28 and 0.65 cm3, with a mean value of 0.47 ± 0.10 cm3 (Table 3). Anatomical success was achieved in 82.2 per cent of the operated patients and functional success was achieved in 68.9 per cent (Table 4).
Table 3. Hearing gain, and mastoid and middle-ear volume in operated ears

SD = standard deviation
Table 4. Graft and functional success rates in operated ears

The mean mastoid volume was 2.09 ± 1.66 cm3 for the patients with successful grafts and 0.98 ± 074 cm3 for those in the graft failure group. A statistically significant difference was found between the mean mastoid volume values of the graft success and failure groups (p = 0.037). However, there was no difference between these two groups in terms of the mean middle-ear volume (p = 0.827) (Table 5).
Table 5. Comparison of mastoid and middle-ear volume in operated ears for graft success and failure groups

*n = 37; †n = 8. SD = standard deviation
When the functional success group was compared with the functional failure group, no statistically significant difference was observed in relation to the mean mastoid volume and middle-ear volume values (p = 0.492 and p = 0.941, respectively) (Table 6).
Table 6. Comparison of mastoid and middle-ear volume in operated ears for functional success and failure groups

*n = 14; †n = 31. SD = standard deviation
The mean mastoid volume of the operated ears was 1.89 ± 1.59 cm3, and that of the intact ears was 2.63 ± 2.09 cm3. A statistically significant difference was detected between the mastoid volume values of the operated and healthy sides (p = 0.046). The mean middle-ear volume values of the operated and intact ears were 0.47 ± 0.10 cm3 and 0.47 ± 0.11 cm3, respectively, revealing no statistically significant difference between the two sides (p = 0.394). The statistical comparison results of the post-operative bone conduction, air conduction and ABG values between the operated and healthy ears are given in Table 7.
Table 7. Comparison of post-operative parameters in operated and intact ears
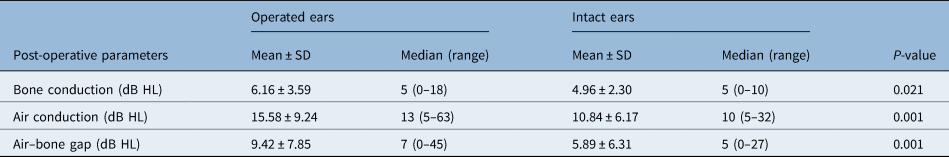
SD = standard deviation
Discussion
As a result of our study, we found that the mastoid pneumatisation volume of the ears with anatomical graft failure was smaller than those of the ears with anatomical graft success in patients who had undergone paediatric tympanoplasty. The mastoid pneumatisation system is a good air reservoir for the middle ear, and the function of the middle-ear cavity is closely related to the degree of pneumatisation of this system.Reference Csakanyi, Katona, Josvai, Mohos and Sziklai11,Reference Kim, Kim, Jeon, Kim, Moon and Lee17 In addition to publications advocating that mastoid development is a genetically determined process, there are those reporting that various environmental factors such as infectious and serous otitis media can limit this development.Reference Lee, Jun, Kim, Jung and Yeo6,Reference Kim, Kim, Jeon, Kim, Moon and Lee17,Reference Merenda, Koike, Shafiei and Ramadan18 Aoki et al.Reference Aoki, Mitani, Tuji, Hamada, Utahashi and Moriyama19 showed that the growth of mastoid cells and the transmucosal gas exchange function of the middle ear were closely related to histopathological changes in the middle-ear mucosa due to middle-ear infections.
The anatomical structure of mastoid cells poses a challenge to accurately measuring the volume; however, 3D measurement techniques have enabled the calculation of true volume. Casale et al.Reference Casale, Shaffrey and Kesser20 compared the mastoid–middle-ear volume calculation technique in temporal bone high-resolution CT with tympanometry, and revealed that radiological measurements were more reliable in this calculation.
Although we identified several publications evaluating mastoid volume in healthy paediatric patients, there were only limited data on paediatric patients with chronic otitis media in this area. Hamada et al.Reference Hamada, Utahashi and Aoki21 showed that severe inflammatory and infectious events in the middle-ear mucosa caused strong suppression of mastoid pneumatisation. Csakanyi et al.Reference Csakanyi, Katona, Josvai, Mohos and Sziklai11 reported that the mastoid volume of children with otitis media with effusion was smaller than that of healthy children (2.82 ± 1.51 ml vs 10.05 ± 5.3 ml). This is supported by the findings of our study, which revealed that the mean mastoid volume of the healthy ears (2.63 ± 2.09 cm3) was significantly higher compared with that of the operated ears (1.89 ± 1.59 cm3).
In contrast to mastoid volume, when we examined middle-ear volume on the intact and operated sides (0.47 ± 0.10 cm3 and 0.47 ± 0.11 cm3, respectively), we did not observe a significant difference. The middle-ear volume values we obtained were similar to the high-resolution CT measurements of healthy control groups reported in the literature.Reference Kavakli, Ogeturk, Yildirim, Karakas, Karlidag and Sarsilmaz4,Reference Kurkcuoglu, Kurkcuoglu, Inancli, Enoz, Pelin and Zagyapan22 The longer vertical elongation of the head being the main factor in the development of middle-ear volume, the middle ear being larger in men than in women, the absence of a significant difference between the middle-ear volume of healthy and diseased ears, and, lastly, the similarity between the previously reported middle-ear volume values of the completely healthy individuals and the data of our chronic otitis media patients suggest that the determinants of middle-ear volume may be genetic rather than environmental factors. Clearer conclusions will be drawn from further studies conducted with different ethnic groups and larger populations.
Although mastoid pneumatisation plays an important role in middle-ear functioning, different findings have been presented regarding the effect of reduced pneumatisation on tympanoplasty success. Holmquist and Bergström showed that the tympanoplasty success rate was high in ears with sufficient mastoid volume even if Eustachian tube function was impaired.Reference Holmquist and Bergström23 In a study conducted with paediatric patients, Merenda et al.Reference Merenda, Koike, Shafiei and Ramadan18 examined the effect of tympanometric volume on tympanoplasty success, and showed that a tympanometric volume of 3 cm3 or above correlated with the success of this surgery. Thus, the authors recommended choosing the time for surgery when the tympanometric volume value was above 3 cm3 in paediatric patients, to increase tympanoplasty success rates. However, in that study, the area evaluated as tympanometric volume included the external ear canal, middle-ear and mastoid cavity volume. Takahashi et al.Reference Takahashi, Sato, Nakamura, Naito and Umeki24 showed that the lack of mastoid pneumatisation and Eustachian tube mechanical obstruction on high-resolution CT imaging negatively affected tympanoplasty results. In contrast, Metin et al.Reference Metin, Kaptan, Dogan, Yazici, Bayraktar and Gocmen25 found no significant relationship between mastoid pneumatisation and graft success and hearing gain in patients undergoing type 1 tympanoplasty and antrostomy. Yegin et al.Reference Yegin, Celik, Simsek, Masallah, Olgun and Aylin2 examined the effect of mastoid pneumatisation on graft success in type 1 tympanoplasty in adult patients and concluded that the degree of mastoid pneumatisation did not affect the operation's success.
Our study draws attention to factors other than those described in the literature that could affect the success of tympanoplasty in paediatric patients with chronic otitis media. We found that mastoid volume was higher in patients with anatomically successful grafts; however, higher mastoid volume did not affect functional success in a statistically significant manner. Casale et al.Reference Casale, Shaffrey and Kesser20 evaluated the relationship between mastoid–middle-ear volume and conductive hearing loss in patients with an isolated tympanic membrane perforation, and showed that hearing loss incidence was higher in ears with a small mastoid–middle-ear volume compared to those with a large volume. Similarly, Mehta et al.Reference Mehta, Rosowski, Voss, O'Neil and Merchant26 reported that the size of the middle-ear volume and the degree of hearing loss were inversely correlated, independently of other variables. However, in both studies, no data were presented concerning the effect of volume values measured in high-resolution CT on post-operative hearing outcomes. In this respect, we consider our study to have the features of a preliminary investigation guiding future research.
• The effects of mastoid and middle-ear volume on the anatomical and functional success of type 1 tympanoplasty in paediatric patients were examined
• Mastoid pneumatisation volume was a positive factor affecting surgical success in paediatric tympanoplasty
• Middle-ear volume had no significant effect on functional and anatomical success
This study has certain limitations. Because of its retrospective design, patients’ records obtained from medical charts may have been inaccurate or missing. The limited number of patients and the absence of a completely healthy control group were other limiting factors. Patient- and disease-related factors that may affect anatomical and functional outcomes should also not be overlooked. Finally, we investigated the anatomical and functional outcomes only at the sixth post-operative month.
Conclusion
We determined that mastoid pneumatisation affected the anatomical success of cartilage tympanoplasty in paediatric patients. The middle-ear volume was not affected by middle-ear pathologies, and it had no effect on the anatomical and functional success of tympanoplasty. However, further studies are needed to evaluate the outcomes in larger patient groups over a longer follow-up period.
Competing interests
None declared












