Introduction
Cochlear implantation is widely accepted as a safe surgical technique for rehabilitation of some types of acquired and congenital hearing loss. Although the surgical technique is well described and standardised (for the most part), there is a lack of consensus concerning the optimal method for fixation of the internal receiver/stimulator. Various fixation techniques have been described, including subperiosteal tight pocket, drilling bone implant bed fixation with or without tie-down sutures, and use of platinum wire ties, ionomeric bone cement, titanium mesh, or a Gore-Tex® patch to secure the implant, although the optimal method has yet to be reported.Reference Adunka and Buchman1–Reference Rudel and Zollner4
Preventing migration of the receiver/stimulator is crucial, as it can lead to wound complications, damage or displacement of the electrode, and extrusion of the implant, all of which can result in the necessity for revision surgery, despite efforts to protect the implant. The present study aimed to determine the effect of the subperiosteal tight pocket technique versus the bone recess with suture fixation technique on the revision cochlear implantation rate and complications.
Materials and methods
The medical records of patients who underwent cochlear implantation performed by two senior surgeons (LS and SS) at Hacettepe University, School of Medicine, Department of Otolaryngology, Ankara, Turkey (a tertiary referral centre), between October 2002 and January 2016, were retrospectively reviewed. Revision cases were identified and included in the study. Patient demographics, the reason for revision, device type and receiver/stimulator fixation technique were recorded. Patients who underwent primary surgery at a different hospital were excluded from the study. The cochlear implants used were manufactured by Cochlear (Sydney, Australia), Advanced Bionics (Valencia, California, USA) and Med-El (Innsbruck, Austria). The reasons for device failure were grouped as hard and soft failure in accordance with the criteria.Reference Balkany, Hodges, Buchman, Luxford, Pillsbury and Roland5
Regarding the fixation method, one surgeon preferred bone recess with suture fixation (between 2002 and 2016), whereas the other preferred subperiosteal tight pocket (between 2002 and 2012, not applied in the last four years as the surgeon no longer works in our clinic). The patients were retrospectively divided into two groups according to receiver/stimulator fixation technique. The study protocol was approved by the Hacettepe University Ethics Committee (approval number: GO 16/376-22).
The surgical technique (transmastoid facial recess approach) was the same in both groups, except for the receiver/stimulator fixation technique. Patients in group one underwent the subperiosteal tight pocket technique, without drilling an implant bed or suture fixation. Patients in group two underwent the bone recess with suture fixation technique, which consisted of drilling a bone implant bed, with a fixating single tie-down suture connecting the periosteal flap to the single bone hole anterior to the implant bed subcortically.
Statistical analysis was performed using IBM SPSS Statistics for Windows software, version 23.0 (IBM, Armonk, New York, USA) and Microsoft Excel spreadsheet software (Microsoft, Redmond, Washington, USA). Descriptive analysis was performed and data were compared between groups using Pearson's chi-square test. Independent samples were compared via the student's t-test. The level of statistical significance was set at p < 0.05.
Surgical technique
General anaesthesia was used in all patients.
Bone recess with suture fixation technique
For the patients in group two, a curvilinear incision approximately 3–4 cm long and 1 cm posterior to the post-auricular crease was used. The skin flap was elevated approximately 2 cm posteriorly from the incision using monopolar cautery. Then, a periosteal incision was made through the periosteum, from the linea temporalis superiorly to the mastoid tip inferiorly (it is important to make the periosteal incision 1 cm posterior to the skin incision, so as to avoid the possibility of wound dehiscence and extrusion of the implant). Then, a cortical mastoidectomy was performed.
Following mastoidectomy, the bone implant bed was prepared. The surgeon was situated in front of the patient, and the periosteum was elevated posteriorly to create a subperiosteal pocket for a dummy implant.Reference Sennaroglu, Sarac and Turan6 After marking the edges of the dummy implant on the mastoid bone, a custom-fit bone implant bed was drilled until it fully accommodated the dummy implant. A proper groove connecting the implant bed and mastoidectomy cavity was drilled for the electrode lead.
Next, for receiver/stimulator fixation, a single hole anterior to the implant bed was drilled and connected subcortically with extreme care to ensure the underlying dura was not injured (Figures 1 and 2).Reference Sennaroglu, Sarac and Turan6 A size 4-0 Vicryl® or Prolene® suture was passed from this hole, and then the needle was passed from the periosteum and the suture ends were clamped (Figures 3–5). The facial recess was opened and a cochleostomy was made. The implant receiver/stimulator was placed in the bone bed and a fixating suture was tied (Figure 6). The electrode was then inserted into the cochlea and the ground electrode (if present) was placed subperiosteally.
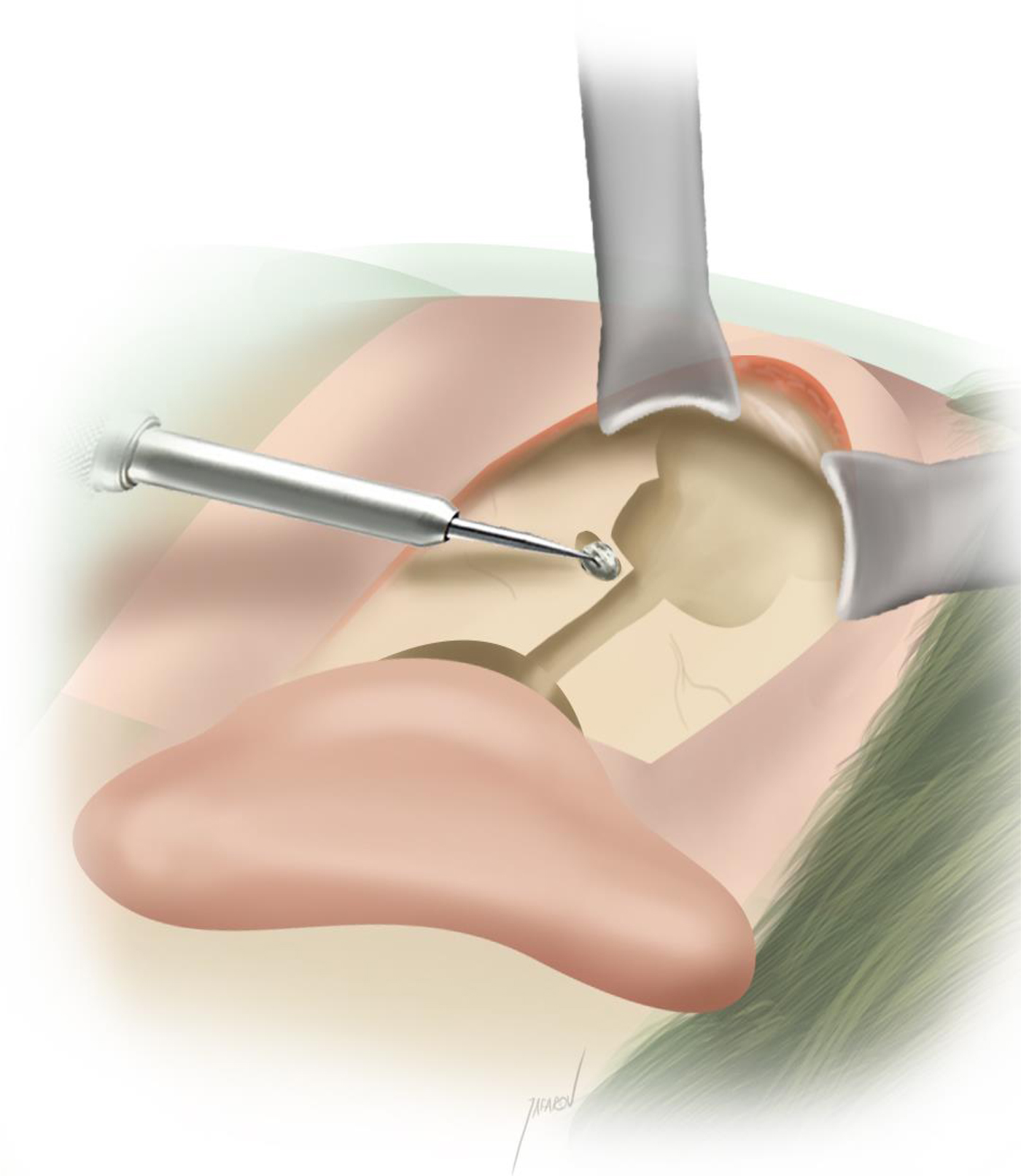
Fig. 1 A single hole anterior to the implant bed was drilled.

Fig. 2 A subcortical connection between the single hole and the implant bed was drilled.

Fig. 3 The suture end was passed through the connecting hole.

Fig. 4 The needle was passed through the periosteal flap.

Fig. 5 The suture ends were clamped.

Fig. 6 Final appearance of the implant after the fixating suture was tied.
The periosteum was closed using continuous locked sutures and the skin incision was then closed using size 4-0 Vicryl interrupted subcuticular sutures. A mastoid dressing was placed over the surgical field.
Subperiosteal tight pocket technique
For the patients in group one, surgery was identical to that in group two, except for the fixation technique. Following periosteal incision and elevation of the anterior-based periosteal flap, a custom-fit tight pocket was created in the parietal region using a periosteal elevator in the subperiosteal plane. The pocket was gradually enlarged and continuously assessed using a dummy implant. Maximum pocket size did not exceed the size of the dummy implant by more than 5 mm, so as to maintain the tightness of the musculoperiosteal flap and secure the receiver/stimulator safely in position. An implant bed was not drilled and sutures were not used (Figure 7).

Fig. 7 Final position of the implant in the subperiosteal pocket technique. The implant bed was not drilled and fixating suture was not used.
Results
A total of 1514 primary cochlear implantations were performed by 2 senior surgeons between October 2002 and January 2016. The receiver/stimulator fixation technique used was the bone recess with single tie-down suture fixation method in 1180 cases (78 per cent), versus the subperiosteal tight pocket method in 334 cases (22 per cent).
In all, 61 revision implantations were performed, of which 9 were excluded from the study because the primary surgery was performed at another hospital. Of the remaining 52 cases, 29 (56 per cent) were male and 23 (44 per cent) were female. Mean age at the time of primary cochlear implantation was 15 years (range, 2–55 years). Mean time from primary surgery to revision surgery was 39.75 months (34.5 ± 22.3 months in group 1 and 44.2 ± 38.3 months in group 2; p = 0.282). The overall revision rate was 3.43 per cent (n = 52); the revision rate was 7.18 per cent (24 of 334) in group 1 versus 2.37 per cent (28 of 1180) in group 2, and the difference was significant (p < 0.001).
None of the patients who underwent revision surgery were aged less than two years. Table I summarises the demographic features of the revision cases. External ear canal obliteration was performed in one patient with chronic otitis media. In another patient, re-implantation was not possible because of extensive fibrosis and total demineralisation of the cochlea, but auditory brainstem implantation was performed subsequently. Because of implant device failure, two patients in group one underwent revision surgery twice. Electrode insertion during revision surgery was full in all cases, except for three cases of partial insertion. There were no intra-operative complications in any of the revision cases. Table II shows the distribution of cochlear implants according to the three device manufacturers.
Table I Demographic features of revision cases

Data represent numbers (and percentages) of cases. *n = 24; †n = 28; ‡n = 52.
Table II Types of cochlear implants

Data represent numbers (and percentages) of cases.
The primary surgery device failure rate was 3.17 per cent. Device failure was the most common reason for revision in both groups. There was a significant difference in the device failure rate between group one (6.88 per cent (23 out of 334)) and group two (2.11 per cent (25 out of 1180)) (p < 0.001). The overall rates of hard failure and soft failure were 1.18 per cent and 1.99 per cent, respectively. There was no significant difference in hard failure and soft failure rates between group one and group two (p = 0.322 and p = 0.418, respectively). Re-implantation was performed because of an infected implant in two patients (one in each group) and was conducted in two patients in group two because of skin flap failure. Table III lists the reasons for re-implantation.
Table III Reasons for revision implantation

Data represent numbers (and percentages) of cases. *n = 24; †n = 28; ‡n = 52.
Discussion
According to the literature, there is a lack of consensus concerning the most effective receiver/stimulator fixation technique. The receiver/stimulator fixation technique not only determines the shape of the incision, but is critical for avoiding device and wound complications. As reported by Davids et al., soft tissue complications can lead to device migration and failure.Reference Davids, Ramsden, Gordon, James and Papsin7 Numerous fixation techniques have been described for overcoming such problems. Some researchers suggest using such external materials as titanium mesh, a Gore-Tex patch, Dacron® and platinum wire ties, and plate fixation, whereas others recommend subperiosteal pocket and suture fixation.Reference Adunka and Buchman1–Reference Djalilian, King, Faust, Smith and Levine3, Reference Shelton and Warren8 The shape of the post-auricular incision has evolved since it was described in 2002 by O'Donoghue and Nikolopoulos.Reference O'Donoghue and Nikolopoulos9 Based on our experience, modified minimal access surgery, as described by Sennaroğlu et al.,Reference Sennaroglu, Sarac and Turan6 makes it possible to perform the time-consuming work of drilling holes for tie-down sutures using a smaller post-auricular incision than is possible with other surgical methods.
In addition to patient characteristics and potential complications, the most important factors determining the receiver/stimulator fixation technique are surgeon experience and preference. Traditionally, the creation of a bone implant bed with fixating sutures anchored to the drill holes was used to secure cochlear implants. A survey of cochlear implant surgeons by Yoshikawa et al. reported that approximately 80 per cent preferred drilling a bone implant bed in adult and paediatric patients, and that 50 per cent preferred an additional fixation method, including sutures and screws.Reference Yoshikawa, Hirsch and Telischi10 Despite the ubiquity of fixing the device to bone, some researchers suggest that it is unnecessary and associated with the risk of complications. Jethanamest et al. reported no receiver/stimulator migration or intra-operative complications in 62 patients whose devices were secured via the subperiosteal tight pocket technique – without a bone implant bed or sutures – and concluded that the technique is safe and effective for cochlear implant surgery.Reference Jethanamest, Channer, Moss, Lustig and Telischi11 Similar to the present study, Güldiken et al. compared the subperiosteal tight pocket and standard techniques in 148 cochlear implantation patients.Reference Güldiken, Orhan, Yigit, Basaran, Polat and Gunes12 They reported no instances of migration or complications in either group. They concluded that the subperiosteal technique is preferable, because of ease of implementation, a low risk of complications and reduced surgical duration; however, device failure rates, which we think might be associated with fixation technique, and revision rates, were not reported.
The overall revision rate of 3.43 per cent in the present study is comparable to earlier reports. Sunde et al. reported a 4.1 per cent revision rate for 439 cochlear implant surgical procedures performed between 2000 and 2012.Reference Sunde, Webb, Moore, Gluth and Dornhoffer13 In 2010, Alexander et al. reported a revision rate of 4 per cent in a study that included 320 paediatric patients.Reference Alexander, Caron and Woolley14 They compared three fixation methods (intraosseous suture ligature, Prolene mesh with titanium screws, and a small periosteal pocket with periosteal sutures) and did not observe device migration, device extrusion or intracranial complications in any of the groups. In the present study, the revision rates (7.18 per cent vs 2.37 per cent) and device failure rates (6.88 per cent vs 2.11 per cent) were significantly higher in group one (subperiosteal tight pocket technique).
The present findings seem to support Shelton and Warren's theory that micro-movement of the fantail can lead to wire fatigue and fantail damage;Reference Shelton and Warren8 however, obvious migration of the receiver/stimulator, and electrode and intra-operative complications, were not observed in either of the present study groups. In addition, we think that disrupted anatomical layers cannot maintain the tightness required to fix the receiver/stimulator to bone during revision surgery. Therefore, bone recess with suture fixation should be preferred for both initial implantation and revision implantation (regardless of the fixation technique used during initial implantation).
The cosmetic profile should also be a consideration when choosing the receiver/stimulator fixation technique. We think lowering the profile of the implant as much as possible is important, not only for protecting the device from damage because of external trauma, but also for achieving a natural symmetrical appearance. Güldiken et al. compared the subperiosteal pocket technique versus bone recess technique, and both the researchers and the patients’ parents reported a little bulging of the skin covering the receiver/stimulator in the subperiosteal pocket group; however, visual analogue scale scores did not differ significantly between the groups.Reference Güldiken, Orhan, Yigit, Basaran, Polat and Gunes12 Although cosmetic concerns could be seen as a minor factor associated with the choice of receiver/stimulator fixation technique, they are especially important to patients with bilateral implants. Using the same fixation technique in both ears in bilateral cases is essential for achieving a symmetrical appearance.
• Accurate fixation of the cochlear implant receiver/stimulator is crucial in cochlear implant surgery
• Various fixation methods have been described previously
• Bone recess and suture fixation method has lower revision and device failure rates than subperiosteal tight pocket method
Surgical duration is another concern during cochlear implant surgery, and it is highly dependent on the fixation technique. As the duration of surgery decreases, so does the exposure to anaesthesia and the cost of surgery. It was reported that surgery duration was significantly lower (up to 30 per cent) for the subperiosteal pocket technique in previous studies.Reference Güldiken, Orhan, Yigit, Basaran, Polat and Gunes12, Reference Sweeney, Carlson, Valenzuela, Wanna, Rivas and Bennett15 Although surgery duration was not analysed in the present study, it is known that drilling a bone implant bed and suture fixation prolongs surgery, but experienced surgeons can complete cochlear implant surgery in 30–40 minutes. The time saved by using other fixation methods does not offset the increased risk of revision surgery.
The retrospective design of the present study is a limitation, which we think is counterbalanced by the large patient population.
Conclusion
Cochlear implantation is a safe and effective method for achieving hearing restoration. Fixation of the receiver/stimulator is a crucial part of the surgical procedure. It should be performed with meticulous care, so as to avoid device migration and complications, both of which can lead to revision surgery. The present findings show that the bone recess with suture receiver/stimulator fixation technique is associated with a lower revision rate than the subperiosteal pocket technique. Therefore, we think the bone recess with suture technique should be the preferred method of receiver/stimulator fixation.
Competing interests
None declared.












