Introduction
Duplication of the internal jugular vein (IJV) is a rare anatomical finding with an estimated incidence of approximately 0.4 per cent among the general population.Reference Prades, Timoshenko, Dumollard, Durand, Merzougui and Martin1 Twelve such cases have been published in the English language literature.Reference Prades, Timoshenko, Dumollard, Durand, Merzougui and Martin1–Reference Downie, Schalop, Mazurek, Savitch, Lelonek and Olson9 However, only two cases of bilateral IJV duplication have been reported (one being a cadaveric finding).
We present a case of bilateral IJV duplication, and we review the literature on IJV duplication (both unilateral and bilateral) with particular regard to the presentation, diagnosis and clinical significance of this finding.
Case report
A 21-year-old woman presented to the ENT clinic with a one-year history of intermittent, right-sided neck swelling. During each episode, she complained of associated dyspnoea and dysphagia. The swelling occurred once a month, lasting one to two days. She had no other significant past medical history.
On examination, there was no obvious swelling. A systemic ENT examination was unremarkable.
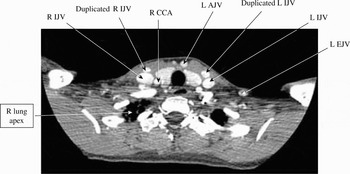
A branchial cyst was suspected and a computed tomography (CT) scan requested. The scan showed bilateral duplicated IJVs running anterior to the main venous channels, commencing at the angles of the mandible (Figure 1). Inferiorly, both sets of duplicated IJVs united at the sternal notch and drained into the left brachiocephalic vein (Figure 2). On three-dimensional, surface-rendered views, apparently normal anterior and exterior jugular veins were well demonstrated (Figures 3 to 5).
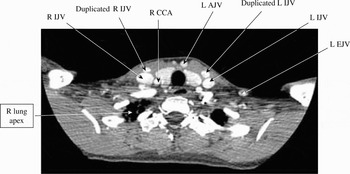
Fig. 1 Axial, post-contrast computed tomography scan at the level of the lung apices. R = right; L = left; IJV = internal jugular vein; AJV = anterior jugular vein; EJV = external jugular vein; CCA = common carotid artery

Fig. 2 Coronal, reformatted computed tomography image showing the duplicated right internal jugular vein (IJV) draining into the left brachiocephalic vein. R = right; L = left; BCV = brachiocephalic vein

Fig. 3 Three-dimensional, surface-rendered, computed tomography image showing both duplicated internal jugular veins (IJVs). R = right; L = left; EJV = external jugular vein; AJV = anterior jugular vein

Fig. 4 Three-dimensional, surface-rendered, computed tomography image showing the duplicated left internal jugular vein (IJV). L = left; EJV = external jugular vein

Fig. 5 Three-dimensional, surface-rendered, computed tomography image showing the duplicated right internal jugular vein (R IJV).
The diagnosis was explained to the patient and reassurances given. No active intervention was undertaken.
The patient was symptom-free for one year. However, her symptoms then recurred, with an additional sensation of neck tightness. Again, conservative treatment was instigated, and the patient's symptoms improved without surgical intervention.
Discussion
The IJVs are the major venous drainage channels in the head and neck. They begin at the jugular foramen, run lateral to the carotid artery in the carotid sheath, and join the subclavian vein behind the sternoclavicular joints to form the brachiocephalic veins. The anatomical course of the jugular veins is usually very consistent; however, anomalies do occur, which may present as a neck swelling or be an incidental (‘subclinical’) finding.Reference Denys and Uretsky10 It has been observed by Downie et al. that previous reports of IJV anomalies have used the terms ‘duplicated’ and ‘fenestrated’ interchangeably, and these authors have proposed more accurate usage of these terms.Reference Downie, Schalop, Mazurek, Savitch, Lelonek and Olson9 The main difference between these two conditions is that duplicated IJVs comprise two separate branches along the whole length of the normal pathway, whereas in fenestrated IJVs the two branches reunite before draining into the subclavian veins.Reference Downie, Schalop, Mazurek, Savitch, Lelonek and Olson9 Downie et al. have suggested that the development of fenestrated and duplicated IJVs differs, because phlebectasia (i.e. congenital dilatation of veins) is only found in duplicated IJVs. However, such a suggestion is debatable due to the limited number of cases.
To our knowledge, 12 cases of duplicated IJVs have been reported: 10 unilateral and two bilateral. Only three cases presented with clinical symptoms, and were subsequently diagnosed on imaging. Of the nine subclinical cases, six were intra-operative findings during neck dissection, two were incidental findings from a head CT investigation for a cerebrovascular event, and one case was a finding from cadaveric dissection. A detailed summary of the 12 cases is given in Table I.
Table I Previous reports of duplicated internal jugular veins: summary

* Both cases. CT = computed tomography; US = ultrasound; MRA = magnetic resonance angiography; R = right; bilat = bilateral; L = left; Y = yes; N = no
• Duplicated internal jugular veins (IJVs) are a rare anomaly with an approximate incidence of 0.4 per cent
• They are usually subclinical, but can present with transient neck swelling
• The presented case had duplicated IJVs with the clinical features of dysphagia and dyspnoea, in addition to the usual neck swelling
• Head and neck surgeons, radiologists and intensive care practitioners should all be aware of this rare anomaly
Of the three cases presenting with clinical features, the only complaint was neck swelling upon straining or performing the Valsalva manoeuvre. Notably, phlebectasia was found only in the three patients with duplicated IJVs. All other cases were incidental findings and had no symptoms prior to the discovery of duplicated IJVs. It would appear that duplicated IJVs, present in isolation, are usually subclinical unless associated with phlebectasia. As most duplicated IJVs are discovered as incidental findings, the prevalence of this anomaly is undoubtedly underestimated.
To date, no complications have been reported due to the presence of duplicated IJVs; however, intra-operative discovery of this anomaly certainly makes neck dissection more time-consuming and potentially more difficult. Fortunately, the majority of patients now undergo imaging prior to major neck surgery, which should identify the condition.
One point worthy of discussion is the use of the duplicated IJV for central venous access. It is important for any surgeon, physician or intensive care practitioner to be aware of this rare anatomical finding, as cannulation of a duplicated IJV may lead to an unusual course on follow-up radiographs. Similarly, radiologists should be aware of such anomalies when reporting imaging of the neck; a finding of duplicated IJVs should be clearly documented in the patient's medical records, and explained to them.
Conclusion
Over the last decade, advances in imaging and the development of surgical approaches have revealed more cases of duplicated IJVs. The presented case provides additional information regarding clinical presentation, as our patient not only had intermittent neck swelling but also dyspnoea and dysphagia. Clinicians should be aware of the rare possibility of duplicated IJVs in patients presenting with neck swellings. If such an anomaly is diagnosed, we would conclude that a conservative approach is indicated, as there is currently no evidence that duplicated IJVs cause any adverse health outcome.