Introduction
Oral ulceration is a common presenting complaint in otolaryngology. There are many recognised causes of oral ulceration. These include local trauma, aphthous ulceration, drug-related ulceration, malignancy and oral ulceration as part of a systemic disorder. This article presents an interesting case of oral ulceration with dual pathology in an elderly patient.
Case report
A 73-year-old woman was referred to the ENT casualty department with a four-month history of pharyngeal pain and a one-month history of ulceration of the left buccal mucosa.
On examination, the patient had a 1 cm opening just anterior to the left palatine tonsil. Deep to this was a large cavity filled with sulphur granules. The tonsil itself appeared normal. In addition, there was a 2 cm, raised ulcer with a punched-out centre on the left buccal mucosa. The ulcer was firm and indurated on bimanual palpation. There were no other abnormalities on examination – specifically, no palpable neck mass and no pyrexia.
Relevant past medical history included gastric carcinoma five years previously, with a recent normal oesophogastroduodenoscopy (OGD), and ischaemic heart disease unsuitable for cardiac artery bypass grafting. Current medications included nicorandil, metoclopramide, isosorbide mononitrate, ramipril, spironolactone, aspirin, clopidogrel and ferrous sulphate. There was no history of tobacco or alcohol use.
There was a high suspicion that this was a malignant lesion, and so the patient was admitted for an urgent computed tomography scan and an examination under anaesthesia with biopsy.
Computed tomography scanning from the skull base to the arch of the aorta revealed an ill-defined, 2–3 cm, soft tissue mass in the left tonsillar fossa, extending into the left parapharyngeal space. The mass contained clumps of coarse calcification with cavitation extending laterally to within a few millimetres of the inner surface of the mandible. There was no evidence of bony involvement. Several small, level two nodes were present. The conclusion of the report suggested that the appearance was likely to be in keeping with an infective process such as actinomycosis or tuberculosis (Figure 1).
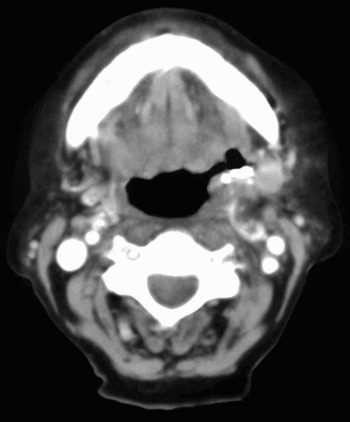
Fig. 1 Axial computed tomography scan showing a 2–3 cm soft tissue mass in the left tonsillar fossa, extending into the left parapharyngeal space.
Examination under anaesthesia with biopsy was performed, and two separate specimens were submitted for histopathology. The first, from the left tonsillar region, revealed features of chronic inflammation. Examination of the debris from the cavity revealed small bacterial colonies of actinomyces. There was no evidence of malignancy. The second biopsy, from the left buccal mucosa, revealed active, non-specific, chronic inflammation with a tendency for the inflammatory cell infiltrate to involve the striated muscle and vascular channels. The possibility of a drug reaction, in particular to nicorandil, was suggested. Again, there was no evidence of malignancy.
Specimens were sent for bacteriological examination. They failed to reveal any growth after 24 hours. However, the patient had been taking antibiotics.
Discussion
This case report describes a patient with two unusual conditions: chronic actinomyces causing a pharyngeal sinus, and ulceration of the left buccal mucosa caused by nicorandil.
Actinomycosis is a rare, chronic, suppurative bacterial disease which is caused by branching, filamentous, gram-positive bacilli of the actinomycosis family. Most major medical centres report approximately one case per year.Reference Belmont, Behar and Wax1 Actinomycosis can form an abscess in the tissues that develops into a hard, red-purple lump. This can break through the skin, forming a pus-discharging lesion.Reference Stewart and Sulek2
Actinomycosis was first reported as an infection in humans in 1845 by Langenbeck, who attributed it to a fungus. Later, in 1876, Bollinger used the name ‘lumpy jaw disease’ because of the disease's presentation in cattle. In 1877, Harz named the infecting organism actinomyces, which means ‘ray fungus’, as it was believed that the organism was a fungus. However, in 1891, Israel and Ponfick delineated the anaerobic nature of actinomyces and isolated it from humans. It was not until the 1960s that Waksman showed actinomyces to be a gram-positive bacteria.Reference Rippon3
Since identification in the 1960s, five species of actinomyces have been identified: Actinomyces israelli, A bovis, A naeslundii, A viscousus and A odontolyticus. These are all gram-positive rods which are strict or facultative anaerobes.Reference Rippon3
The pathogenesis of actinomycosis still remains unclear. Precipitating factors which are thought to lead to human infection in the cervicofacial region include dental caries, dental manipulation and maxillofacial trauma.Reference Belmont, Behar and Wax1 However, no such precipitating factors were noted in our patient, despite investigation by the oral surgeons.
Actinomycosis has been known to involve virtually every anatomical site in the body.Reference Bhargava, Bhusnurmath, Sundaram, Raman, Al Okbi, Al Abri and Date4 In 1938, Cope classified actinomycosis into three distinct forms: cervicofacial (50 per cent), pulmonothoracic (30 per cent) and abdominopelvic (20 per cent).Reference Belmont, Behar and Wax1 However, the presenting clinical manifestations can be confusing because they often mimic other disease processes. The current case report presents a patient who was found to have cervicofacial actinomycosis, the commonest form.
The diagnosis of actinomycosis is often difficult to make on clinical grounds, due to the disease's varied presentation. In order to confirm the diagnosis of actinomycosis, two of the following conditions must be present: positive cultures, sulphur granules or biopsy specimens showing the organism.Reference Benhoff5 In our case, the patient's diagnosis was confirmed by the presence of sulphur granules and a pathology report confirming the presence of bacterial colonies of actinomyces. Culture samples in this case were negative, but the organism is known to be difficult to isolate in culture.Reference Stewart and Sulek2
The current recommended therapy includes four weeks of high dose intravenous penicillin, followed by a three- to six-month course of oral penicillin, continuing treatment even after total resolution of symptoms. Other antimicrobials that have been found to be effective include tetracycline, erythromycin and clindamycin.Reference Benhoff5 Our patient was commenced on a 12-week course of 1 g amoxicillin thrice daily, as recommended by the bacteriologist.
As well as cervicofacial actinomycosis, this patient also suffered from oral ulceration caused by nicorandil. This is a potassium channel activator which is used for the long-term treatment of ischaemic heart disease. Over recent years, nicorandil has been reported to have precipitated persistent ulcerative stomatitis in a small percentage of patients.Reference O'Sullivan6
The ulcers induced by nicorandil are very painful and distressing for patients. Clinically, they appear as large, deep, persistent ulcers that have punched-out edges.Reference Healy, Smyth and Flint7 The ulcer that was found in our patient fits with the classical description of a nicorandil-induced ulcer. However, one must have a high index of suspicion and have taken a thorough history in order for the diagnosis to be considered.
• Actinomycosis of the head and neck region, although rare, is an important entity to the otolaryngologist, as it can often masquerade as other conditions, including oropharyngeal malignancies
• Nicorandil is a potassium channel blocker used in the treatment of ischaemic heart disease. It has been recently recognised as a cause of persistent ulcerative stomatitis
• This case report describes a patient with two unusual conditions: chronic actinomyces causing a pharyngeal sinus, and ulceration of the left buccal mucosa caused by nicorandil
The treatment of Nicorandil-induced ulceration is to reduce or discontinue the medication. The ulcers are usually poorly responsive to topical steroids. Discussion with a cardiologist is often required prior to changing medication. Alteration of the nicorandil dose is usually sufficient to promote ulcer healing and to prevent further recurrence.Reference Healy, Smyth and Flint7 Our patient was referred to a cardiologist with a view to discontinuing the nicorandil.
Conclusion
This case report highlights several important issues. Actinomycosis of the head and neck region, although rare, is an important entity to the otolaryngologist as it can often masquerade as other conditions, including oropharyngeal malignancies. Therefore, it is important to have a high index of suspicion in order to make an accurate and timely diagnosis. Early investigation and treatment can then allow the patient to make a quick and full recovery.
This also applies to nicorandil-induced oral ulceration. A high index of suspicion, combined with a thorough patient history, is required to diagnosis and manage this potentially reversible condition.
The other important aspect of the current case is that one must always be alert to the possibility of dual pathology. Our patient was suspected of having an oropharyngeal malignancy, when in fact she had two independent, potentially reversible conditions: drug-induced oral ulceration and infective oral ulceration. Both these conditions were able to be treated, allowing the patient to make a full recovery.



