Introduction
Chronic rhinosinusitis is one of the most common healthcare problems, with evidence suggesting a significant and continuous increase in its incidence.Reference Fokkens, Lund, Mullol, Bachert, Alobid and Baroody1 According to a general population survey, chronic rhinosinusitis affects up to 11.9 per cent of the US populationReference Hirsch, Stewart, Sundaresan, Young, Kennedy and Scott Greene2 and up to 10.9 per cent of the population in Europe.Reference Hastan, Fokkens, Bachert, Newson, Bislimovska and Bockelbrink3 This chronic condition has a major impact on quality of life.Reference Phillips, Hoehle, Bergmark, Caradonna, Gray and Sedaghat4,Reference Hoehle, Phillips, Bergmark, Caradonna, Gray and Sedaghat5
Conservative treatment of chronic rhinosinusitis is aimed at reducing inflammation, controlling the infection, and restoring the function of nasal mucosa and sinuses. Nasal irrigation with saline, unlike maxillary sinus irrigation, is common within the framework of conventional treatment of chronic rhinosinusitis.Reference Wei, Adappa and Cohen6 Its impact is mostly mechanical (removal of discharge), but some claim that it can also have a certain anti-inflammatory effect.Reference Snidvongs, Chaowanapanja, Aeumjaturapat, Chusakul and Praweswararat7 Direct maxillary sinus puncture has the advantage of irrigating the sinus without the need for surgery.
We hypothesised that the use of direct maxillary sinus puncture with saline irrigation in chronic rhinosinusitis without polyps would provide added value when used in combination with systemic antibiotics, and therefore potentially prevent the need for sinus surgery in some patients. This work evaluated the effectiveness of maxillary sinus saline irrigation combined with systemic antibiotics versus systemic antibiotics alone in patients with chronic rhinosinusitis without polyps.
Materials and methods
Ethical approval
The study was approved by the Carmel Medical Center's institutional review board and was registered in clinicaltrials.gov (NCT00335309).
Patients and study design
In this prospective randomised controlled trial, patients of ages 18–80 years with chronic rhinosinusitis without polyps diagnosed according to the European Position Paper on Rhinosinusitis and Nasal Polyps 2020 criteriaReference Fokkens, Lund, Mullol, Bachert, Alobid and Baroody1 for chronic rhinosinusitis and who had symptoms for at least three months were randomly assigned into either study or control cohorts. Patients with nasal polyps, with prior sinonasal surgery or cranio-facial trauma, isolated frontal or sphenoid sinusitis, cranial deformity, allergic fungal sinusitis, sinusitis of dental origin, bleeding predisposition, allergy to penicillin or who were immunocompromised were excluded from the study.
All patients were referred by community otolaryngology specialists, provided signed informed consent before enrolment, and had maxillary or ethmoidal sinusitis that was confirmed by computed tomography (CT) scan. Randomisation was completed by an independent person according to a 1.5:1 ratio within blocks of 10, generated using a random number generator (www.random.org). Allocation was concealed from the investigators (see Figure 1).
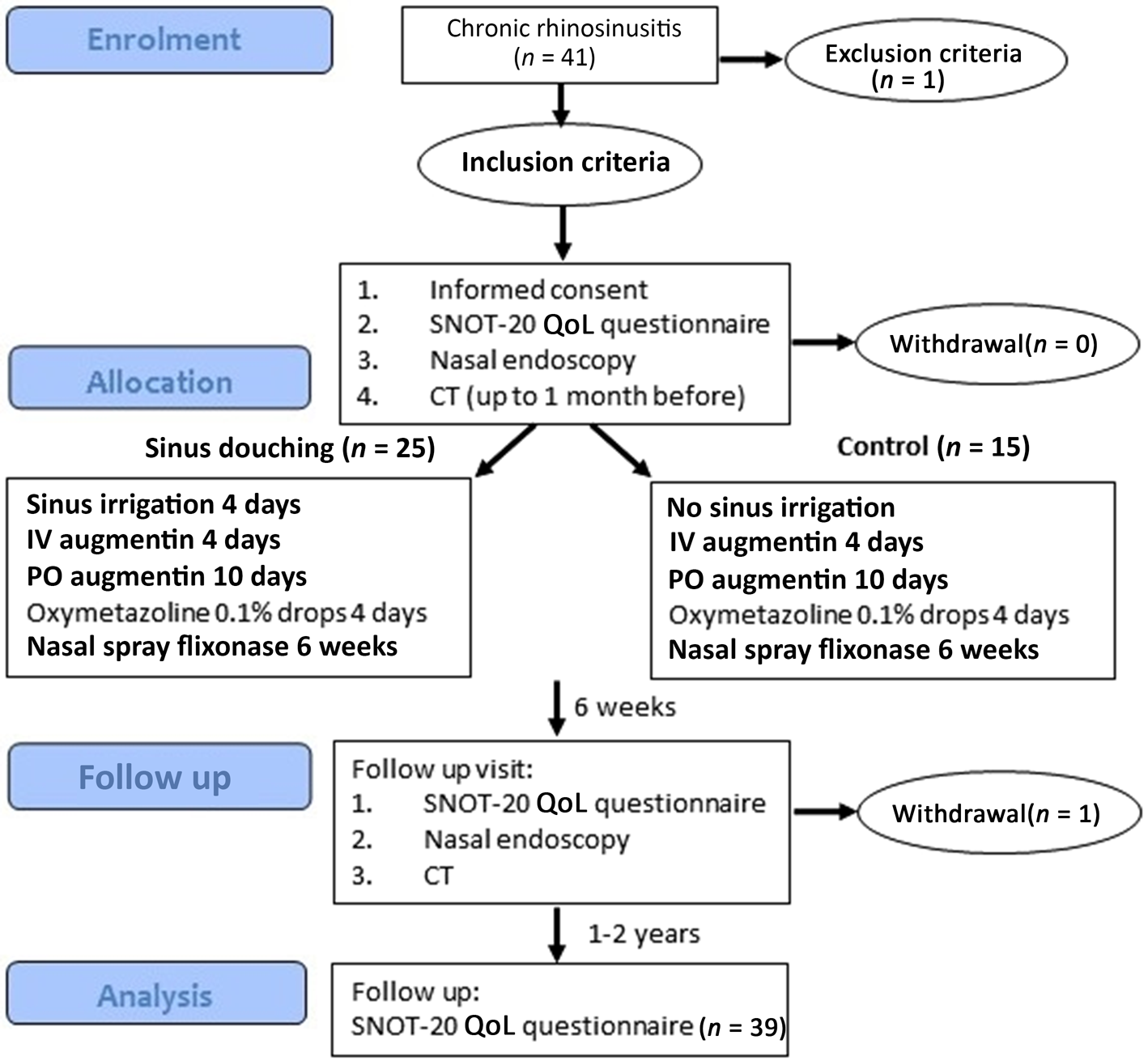
Fig. 1. Graphic chart describing the study process. SNOT-20 = Sino-Nasal Outcome Test-20; QoL = quality of life; CT = computed tomography; IV = intravenous; PO = per os
All patients were treated with systemic antibiotics that included intravenous (IV) amoxicillin with clavulanic acid (1000 mg, 3 times daily for 4 days and further administration of Augmentin® 875 mg twice daily for an additional 10 days). Patients also received nasal oxymetazoline 0.1 per cent drops (two drops in each nostril twice daily) for four days and fluticasone nasal spray (50 mcg/spray) in each nostril, twice daily, for six weeks. Of note, this treatment protocol was designed and executed before the European Position Paper on Rhinosinusitis and Nasal Polyps 2020 guidelines were published. Therefore, topical steroids and saline nasal irrigation were not included.
Direct sinus irrigation technique
Only patients in the study group received maxillary sinus saline irrigation (Figure 2). The irrigation was performed using the SinoJect system (Atos, New Berlin, USA), which includes a silicon tube that is inserted into the maxillary sinus after local anaesthetisation of the inferior meatus with cotton wool soaked in a mixture of naphazoline 0.1 per cent and pantocaine 2 per cent for 20 minutes. The tip of the silicon tube extruded about 1 cm from the nostril and was secured in the maxillary sinus via its arrow-shaped head. The sinus was irrigated by a physician, during hospitalisation, with 100 ml normal saline warmed to room temperature, twice daily, for 4 consecutive days.

Fig. 2. Direct maxillary sinus irrigation technique. Irrigation was performed using the SinoJect system, which includes a silicon tube fixed to the inferior meatus and inserted under local anaesthesia. Image courtesy of O Ronen.
Outcome measures
A nasal endoscopy exam and CT scan were performed before and six weeks after the irrigation protocol. CT scans carried out up to one month before enrolment were eligible to be used as pre-treatment scans. In addition, patients were asked to complete the Sino-Nasal Outcome Test (SNOT-20) quality of life questionnaire before and six weeks after treatment.
The SNOT-20 questionnaire was divided into its four domains: rhinological, ear and facial symptoms, sleep and psychological symptoms, and the two independent questions on ‘cough’ and ‘waking-up tired’.
Nasal endoscopy provided an objective assessment of the nasal mucosa. The endoscopic appearance of each side of the nasal mucosa was scored according to the nature of the discharge (0: no discharge, 1: clear, 2: thick and purulent) and the condition of the mucosa (0: normal; 1: mild hyperplasia without erythema; 2: prominent hyperplasia with erythema). Physicians performing the endoscopy were blinded to treatment allocation. The CT scans were independently scored according to the Lund–Mackay system by two blinded rhinologists.Reference Lund and Mackay8
Patients who showed improvements were followed up, while those who did not show improvement were offered alternative treatments (irrigation if they were assigned to the control group or endoscopic sinus surgery).
One to two years after hospitalisation, patients filled out another SNOT-20 questionnaire.
Failure in the study group (irrigation) was defined as persistent symptoms requiring endoscopic sinus surgery. Failure in the control group was defined as progression beyond the standard basic treatment (i.e. congestion relievers and antibiotics or, alternatively, persistent symptoms requiring endoscopic sinus surgery).
Statistical analysis
The data analysis was performed using SPSS® statistical software (version 24.0). In order to compare demographic and clinical characteristics between the two cohorts, a chi-squared test was performed for categorical variables and an independent t-test was performed for continuous variables. Repeated measures were used to examine whether there was a difference in the mean values of SNOT-20 between the different time points and between the study and control cohorts, and a comparison in pairs was performed using the paired t-test with Bonferroni correction. Pre-treatment and post-treatment results in each group were compared using McNemar's test. A linear mixed model was used to determine whether there is a difference in post-CT total scores between the two groups. A p-value less than 0.05 was considered statistically significant. Two-tailed tests were used, unless otherwise mentioned. The sample size calculation was 25 ± 3 patients and 22 patients for continuous primary endpoints, with an enrolment ratio of 1.5:1, α = 0.05 and a power of 80 per cent; therefore, 33 patients were needed.
Results
A total of 41 patients participated in the study; 24 were assigned to the study group and 15 were assigned to the control group. One to two years after the beginning of the study, 36 patients (92.6 per cent) completed the SNOT-20 questionnaire (Figure 1). Patient demographic data and baseline characteristics, including age, gender, common symptoms and duration of symptoms were similar between the two groups (Table 1). No adverse outcomes or effects were recorded. There were no complications related to the insertion or withdrawal of the irrigation system.
Table 1. Patient demographic data and baseline clinical characteristics

* n = 24; †n = 15. SD = standard deviation
Primary outcomes
Sino-Nasal Outcome Test-20
Overall pre-irrigation SNOT-20 scores were relatively similar between study cohorts. Only the pre-treatment psychological symptoms (the control group had a lower score; p = 0.023) and the pre-treatment ‘waking-up tired’ item (the control group had a lower score; p = 0.027) were significantly different between cohorts. Following treatment, SNOT-20 values in each treatment arm showed an improvement between time points in each group separately (p < 0.0001), but no differences were found between cohorts (Figure 3). In both cohorts, the pre-treatment subdomain scores were statistically higher in both groups, study and control, when compared with the post-treatment scores.

Fig. 3. Mean Sino-Nasal Outcome Test-20 scores in each treatment group over time. Pre-treatment meant completing the questionnaire before irrigation, and post-treatment meant completing the questionnaire during post-treatment follow up (after six weeks) and late post-treatment meant questionnaire completion during a telephone call after one to two years. P < 0.0001 was obtained for each group separately. SNOT-20 = Sino-Nasal Outcome Test-20
Endoscopy
Endoscopic evaluation score is presented for each side separately. In order to avoid compromising the statistical significance of the test, each nasal side was assessed separately, and only the ‘affected’ side was accounted for in the study. A total of 39 patients participated in the study; 16 of them had bilateral disease. Therefore, a total of 55 affected sides were assessed (32 in the study group and 23 in the control group).
Endoscopy scores in the study group were higher (higher disease severity) than in the control group (see Appendix 1). Endoscopy scores were divided into two severity categories (i.e. endoscopic scoring with grade 0–1 and endoscopic scoring with grade 2 and above). No baseline difference in the proportions of abnormal endoscopy scores (grade more than 2) was found between the control and study group. An adjusted model for predicting abnormal endoscopy, with group as an independent variable, controlling for patients with bilateral presentation and using the pre-treatment endoscopy result before treatment, found no significant differences between the two groups (control group: 47 per cent; 95 per cent confidence interval (CI), 25–70 versus study group: 32 per cent; 95 per cent CI, 16–54).
The study group showed a statistically significant reduction in the percentage of abnormal endoscopy scores after treatment in the endoscopic examination before and after treatment (p < 0.0001) whereas the control group did not (Appendix 2 and 3). However, when considering nasal endoscopy scores by ordinal numbers (1–4) and not by dichotomy division (0–1, 2–4), no statistically significant differences were found between the study and control groups (Appendix 2 and 3).
Computed tomography scan
The agreement among the two rhinologists pre-treatment was κ = 91.2 per cent (95 per cent CI, 82.8–99.6). An adjusted model for predicting abnormal CT osteomeatal complex, with group as an independent variable, controlling for patients with bilateral presentation, and using the CT osteomeatal complex result before treatment, showed no significant change between the two groups (adjusted odds ratio (control vs study) = 1.3; 95 per cent CI, 0.40–4.3; p = 0.665; adjusted proportions of abnormal endoscopy after treatment in control group = 47 per cent; 95 per cent CI, 23–73 vs 40 per cent; 95 per cent CI, 20–64 in the study group). Both groups showed a decrease in abnormal CT osteomeatal complex scores (study group: p = 0.001; control group: p = 0.039; Appendix 4).
Baseline total mean CT values did not differ between the study and the control group. A linear mixed model with post-treatment CT score as a dependent variable and group as an independent variable found no difference between arms (–0.81; 95 per cent CI, –2.34 to 0.73). Both treatment protocols led to a statistically significant decrease in total CT score within six weeks (p < 0.001; Figure 4).

Fig. 4. Mean computed tomography (CT) scores determined according to Lund–Mackay score per treatment arm. An improvement can be seen in the two groups after the treatment, but there is no difference between the groups. The mean difference in the study group was 2.25 and was 2.26 in the control group.
Treatment failure
A total of 4 patients from the study group (16.7 per cent; 95 per cent CI, 6.7–35.9) were classified as therapeutic failures since they required endoscopic sinus surgery. Four patients in the control group (26.7 per cent; 95 per cent CI, 10.9–52.0) were defined as therapeutic failures. No statistically significant inter-cohort differences in failure rates were found (p = 0.686). Of note, three patients from the control group who underwent irrigation after the study terminated reported significant and long-term relief several weeks after the irrigation.
Discussion
Main findings of our study
The present study compared the efficacy of saline maxillary sinus irrigation compared with medical treatment of chronic rhinosinusitis, tailored to patients who took part in the study. No statistically significant difference was found between the study and control groups in terms of SNOT-20 and CT indices. That is, the sinus puncture irrigation added no value to the conventional treatment according to these indices. However, endoscopic examination identified improvements in the post-treatment appearance of the sinuses and nasal mucosa in the irrigation group.
Saline sinus irrigation may effectively relieve the acute phase of the disease, as suggested by the significant relief achieved in the three patients from the control group who underwent irrigation after the study terminated.
A comparison with other studies
Previous controlled studies also reported on a limited advantage of maxillary sinus irrigation.Reference von Sydow, Axelsson and Jensen9–Reference Friedman, Hamilton, Samuelson, Maley, Wilson and Venkatesan13 A review published in 2012 examining the literature regarding nasal saline irrigations in chronic rhinosinusitis management found that the irrigations significantly reduced inflammation and enhanced clinical responses.Reference Khianey and Oppenheimer14 Another review conducted in 2013 concluded that saline nasal irrigations are a useful supplement in treating the symptoms of chronic rhinosinusitis in comparison to spray.Reference Achilles and Mosges15
Sino-Nasal Outcome Test 20 for evaluation
The SNOT-20 questionnaire was chosen as it has a proven validity and correlation with imaging tests.Reference Wabnitz, Nair and Wormald11 It is important to note that the patient population treated in this study suffered from more severe rhinosinusitis than the population examined in other studies.Reference Pynnonen, Mukerji, Kim, Adams and Terrell12,Reference Achilles and Mosges15 Nevertheless, a significant 23 to 28-point improvement in SNOT-20 scores was achieved in both groups. These improvement values are similar to those obtained following endoscopic sinus surgery.Reference Colclasure, Gross and Kountakis16 In view of this, it is likely that initial conventional treatment for severe rhinosinusitis provided significant relief by reducing nasal discharge and oedema and by clearing the tract of secretions, bacteria, allergens and inflammatory mediators. The improvement cannot be attributed to the nasal irrigation, since no statistically significant difference was observed between the treatment arms.
Endoscopic evaluation
Although improvements were measured in both the study and the control groups, endoscopically evaluated mucosa appearance was superior in patients undergoing combination when compared with standard therapy. In the study group, the difference was statistically significant. The endoscopic appearance is likely to improve under conventional treatment with supplemental irrigation. Other studies also showed improved endoscopic appearance after treatment.Reference Moshaver, Velazquez-Villasenor, Lavigne and Witterick17,Reference Ragab, Lund and Scadding18
Evaluation by computed tomography
CT scan scores aligned with clinical manifestations and showed improvement after conventional treatment with and without irrigation. That is, the improvement could not be attributed to the maxillary sinus irrigation, since no statistically significant difference was observed between the treatment arms. Other studies showed similar degrees of efficacy of saline sinus irrigation and antibiotics in patients with refractory chronic rhinosinusitis, as assessed by clinical index and CT scans.Reference Moshaver, Velazquez-Villasenor, Lavigne and Witterick17
Study strengths
In contrast to other recent studies,Reference Moshaver, Velazquez-Villasenor, Lavigne and Witterick17,Reference Lavigne, Tulic, Gagnon and Hamid19 this study was both prospective and controlled. The study showed that conventional conservative treatment is effective for initial therapy of severe chronic rhinosinusitis. It suggests that for most patients with the above characteristics, direct sinus saline irrigation might serve as a bridging treatment until surgical intervention. Another advantage of this study is its long follow-up period, with short-term outcomes measured six weeks after treatment and long-term outcomes measured up to 2 years after initial treatment.
This study was also the first one to assess the efficacy of sinus irrigation assessment both by subjective and by objective clinical indices (both CT and endoscopy).
Study limitations
Although all the treated patients had involvement of the maxillary sinus, some had involvement of other sinuses as well. Direct maxillary sinus irrigation did not itself clear the content of other sinuses, although it could clear the middle meatus and reduce the bacterial biofilm burden and associated local inflammation.
Patients were treated with amoxicillin and clavulanic acid rather than with roxithromycin, which has become the drug of choice after this study was conducted. A culture was not obtained since the treatment was empiric and patients were not immunosuppressed. Of note, direct culture of the maxillary sinus was not performed for patients in the control group. Detailed information on previous treatment, including antibiotic regimens, was not uniformly collected, and therefore was not included in the analysis.
The study was designed to examine long-term relief in patients with chronic disease. Therefore, information on either short-term relief or on the initial maxillary washings was not collected.
It is important to note that patients with nasal polyposis were not included in this study, and the conclusions of the current study are not applicable to this subgroup.
Although the irrigation schedule (twice daily for four days) is common, recent studies suggest that sinus irrigation may have to be done once every few months. In this study, post-treatment responses were examined over a relatively long time period, during which no irrigations were performed.
The study involved all patients admitted to the hospital to receive IV antibiotics. This would be difficult to introduce and justify in other healthcare systems. Future research should address the outcomes and health economics of all study arms.
Although the sample size had sufficient statistical power, both the study and the control groups were small.
Looking into the future
A follow-up study should examine the long-term efficacy of the conventional treatment, possibly with addition of sinus irrigation once every few months, in comparison to surgical treatment (endoscopic sinus surgery). This option might be relevant for patients with isolated maxillary sinusitis, those unfit or unwilling to undergo surgery, or as a bridging procedure before surgery. In addition, direct sinus irrigation with substances other than saline, such as steroids and or antibiotics, should be assessed.
• This study assessed the effectiveness of direct maxillary sinus irrigation for the management of chronic rhinosinusitis without polyps
• Endoscopy findings, quality of life, and computed tomography (CT) evaluations were performed over two years following treatment
• CT scores significantly improved in both treatment arms, with no difference between treatments
• Post-treatment nasal endoscopy findings were significantly improved from baseline in the study group but were similar to those of the control group
• Sino-Nasal Outcome Test-20 scores showed improvement in both treatment arms, but with no differences between groups
• In patients with chronic rhinosinusitis without polyps, maxillary sinus irrigation combined with antibiotics and nasal steroids had no beneficial effect
Conclusion
In patients with chronic rhinosinusitis without polyps, direct maxillary sinus irrigation does not have a beneficial effect over conservative treatment alone. A small number of patients eventually required surgical intervention; therefore, a long-term follow-up study should examine the efficacy of conservative treatment in comparison with surgery for chronic rhinosinusitis without polyps.
Acknowledgements
We wish to thank Mrs Tobie Kuritsky and CBR Migal for editorial assistance.
Competing interests
None declared
Appendix 1. Baseline endoscopy and CT parameters by treatment arm

Appendix 2. Distribution of the endoscopy score categories (0–1 and equal to or more than 2) in the two treatment arms, before versus after treatment.

The number in the column indicates the number of patients in the scoring category. Both groups showed a decline in the number (percentage) of patients with an endoscopy score equal to or more than two after the treatment. (a) Study. Pre-treatment: number of patients with endoscopy score 2–4, 28 (87.5 per cent; 95 per cent confidence interval (CI), 71.9–95.0). Post-treatment: number of patients with endoscopy score 2–4, 11 (34.4 per cent; 95 per cent CI, 20.4–51.7). (b) Control. Pre-treatment: number of patients with endoscopy score 2–4, 16 (69.6 per cent; 95 per cent CI (49.1–84.4). Post-treatment: number of patients with endoscopy score 2–4, 12 (52.2) 95 per cent CI (33.0–70.8).
Appendix 3. When considering nasal endoscopy scores as ordinal numbers (1–4), no statistically significant difference was measured between the study and control arms (p = 0.223).

Appendix 4. Computed tomography (CT) osteomeatal complex score (Lund–Mackay: 0, no occlusion and 2, occlusion) distribution, before versus after treatment.

The number in the column indicates the number of patients in the scoring category. Both arms showed a decline in the number (percentage) of patients with a CT score equal to two after the treatment. (a) Study. Pre-treatment: number of patients with CT osteomeatal complex score 2, 28 (87.5 per cent; 95 per cent confidence interval (CI), 71.9–95.0). Post-treatment: number of patients with CT osteomeatal complex score 2, 15 (46.9 per cent; 95 per cent CI, 30.9–63.6). (b) Control. Pre-treatment: number of patients with CT osteomeatal complex score 2, 20 (86.7 per cent; 95 per cent CI, 67.9–95.5). Post-treatment: number of patients with CT osteomeatal complex score 2, 13 (56.5 per cent; 95 per cent CI, 36.8–74.4). OMU = ostiomeatal complex







